Abstract
Objective: The authors sought to assess spirituality in depressed patients and evaluate whether the degree of initial depressive symptoms and response to pharmacotherapy treatment has a correlation with degree of spirituality and belief in God.
Methods: Our participants included 84 patients who presented to a depression/anxiety clinic for naturalistic treatment of their depressive illness over the course of two years. All patients met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision criteria for major depression, as confirmed by structured interviews using the Structured Clinical Interview for DSM-IV, and were treated with selective serotonin reuptake inhibitors for eight weeks.
Measurements: Patients were evaluated at baseline and after treatment using the Montgomery Asberg Depression Rating Scale, the Beck Hopelessness Scale, the Dysfunctional Attitude Scale, and the Spiritual Orientation to Life scale.
Results: At baseline, patients reporting greater spirituality had significantly lower measures of hopelessness, dysfunctional attitudes, and depressive symptoms. Those who believed in God had a greater mean change score than those who did not on the Montgomery Asberg Depression Rating Scale, the Beck Hopelessness Scale, and the Dysfunctional Attitude Scale, with the Montgomery Asberg Depression Rating Scale showing the greatest mean change score. Significant correlations were detected between the Spiritual Orientation to Life scale score and the Montgomery Asberg Depression Rating Scale, the Beck Hopelessness Scale, and the Dysfunctional Attitude Scale pre-scores, post-scores, and change scores.
Conclusion: The findings suggest that greater spirituality is associated with less severe depression. Moreover, the degree to which the measures of depressive symptom severity, hopelessness, and cognitive distortions improved over the course of eight weeks was significantly greater for those patients who were more spiritual.
Keywords: Spirituality, religiosity, depression, major depressive disorder
IN MEMORIAM
Eric D. Peselow, MD, the first author, passed away during the publication of this article. Dr. Peselow was a unique teacher, clinician, and human being who made an unforgettable impact on everyone with whom he interacted. We will always remember Dr. Peselow as an honest, direct, and true-to-self psychiatry professor. May he rest in peace.
INTRODUCTION
Major depressive disorder (MDD) is one of the leading causes of emotional suffering and is projected to become the second leading cause of overall disease burden worldwide by the year 2020.1 Spirituality has been long neglected in depression largely due to predominance of the disease model with its emphasis on risk factors rather than protective factors,2 Freud’s legacy of pathologizing religion,2 and a lower percentage of psychiatrists who espoused a belief in God. Using data collected in 2003, Curlin et al3 showed that 65 percent of psychiatrists reported believing in God, compared to 77 percent of all physicians (p=0.01). This undoubtedly had an impact on the degree and kind of attention paid to spiritual or religious ideas in both treatment and research that caused the influence of faith to be overlooked for so long. Psychiatry is only recently focusing on spirituality as a potentially important variable in understanding depression and its treatment. It is important to note that the amorphous and multidimensional nature of faith manifested as both religiosity and spirituality can, at first glance, make it a difficult variable to incorporate into research. However, despite these factors, in recent years increased attention has been paid to these related fundamental elements of human experience.
Humans have long made use of religion and spirituality to counter depression and other emotional illnesses. For example, the results of several studies have suggested that intrinsic religiosity and spirituality are negatively associated with depression.4-9 Although many often use the terms religiosity and spirituality synonymously, they are not quite the same, and there have been many approaches in attempting to define the two. Traditionally, religion, which can be positive and negative, substantive and functional, was perceived as a broadband construct, with an emphasis on personal religiousness and a lack of an explicit distinction between religion and spirituality.10,11 In contrast, the modern approach depicted religion as more of a narrowly defined construct that was external, institutional, substantive, and negative as opposed to the polarized spirituality that was personal, relational, functional, and positive.10,11 Zinnbauer et al,10 however, argue for an alternative approach that can “distinguish between the constructs without polarizing them,” as can be seen in Pargament’s11 definition of the two terms. According to Pargament,11 religion is “a search for significance in ways related to the sacred,” encompassing both sacred ends as well as sacred means and pathways to perhaps secular ends. Spirituality, which is a direct search for the sacred, can then be viewed as a part of religion where people come across, preserve, and transform what they believe is sacred in their lives.12 Though religion and spirituality are closely related, we chose to focus on the latter since previous studies have shown that not all areas of religion may be effective.
The purpose of this paper is to assess spirituality as measured by a specific scale in depressed patients treated in an outpatient anxiety and depression clinic with selective serotonin reuptake inhibitors (SSRIs), such as escitalopram, sertraline, or paroxetine, and evaluate whether the degree of initial depressive symptoms and response to pharmacotherapy treatment has a correlation with not only the degree of spirituality, but also the belief in God (defined as “believers” vs. “non-believers”). Furthermore, we hope to better understand the factors involved in the relationship between depression and spirituality by assessing hopelessness and dysfunctional attitudes.
METHOD
Study population. Our group evaluated 84 patients who presented to an urban depression and anxiety clinic for naturalistic treatment of their depressive illness over the course of two years. All patients met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV TR) criteria for a major depressive episode. Patients at the time of presentation signed voluntary informed consents for the collection of clinical data upon presentation and during the natural course of antidepressant treatment according to the Institution Review Board-approved protocol. Patients were initially evaluated with a modified Structured Clinical Interview for DSM-IV (SCID) to confirm the diagnosis of major depression.13
Outcome measures. Montgomery Asberg Depression Rating Scale (MADRAS).14 The MADRS is a 10-item scale to measure the severity of depressive symptoms. It includes 10 items, each of which has a rating scale from 0 (no symptom) to 6 (symptom present and severe). Each item assesses one symptom of depression. These include apparent sadness, reported sadness, inner tension, reduced sleep, reduced appetite, concentration difficulties, lassitude, inability to feel, pessimistic thoughts, and suicidal thoughts. Remission is defined as MADRS scores of 8 or less, response as MADRS scores of 9 to 14, and non-response as MADRS scores of above 14. The MADRS has a high intra-class correlation (r=0.93, p<0.0001).14
Beck Hopelessness Scale (BHS).15 The BHS is a 20-item self-report scale measuring three major aspects of hopelessness: feelings about the future, loss of motivation, and expectations.15 It includes 20 statements, each of which has a true or false response to endorse a pessimistic statement or deny an optimistic statement.15 The BHS has an internal consistency—Cronbach alpha—ranging from 0.82 to 0.93 and a test-retest reliability of 0.66.15
Dysfunctional Attitude Scale (DAS).16 The DAS is a 40-item self-report inventory measuring dysfunctional beliefs such as cognitive distortions frequently found to be elevated during depression. It includes 40 statements, each of which has a 7-point scale (i.e., totally agree, agree very much, agree slightly, neutral, disagree slightly, disagree very much, totally disagree). These include concerns about approval from others, prerequisites for happiness, and perfectionist standards. The DAS has an internal consistency— Cronbach alpha—of 0.93 and a test-retest reliability of 0.73 (p<0.001).16
Spiritual Orientation to Life (SOL) scale.17,18 The SOL, a modified version of Feagin’s “Orientation to Life and God Scale” designed to “capture an orientation to life and God that incorporates aspects of religion and spirituality,” is a 7-item scale rated on a 1- to 5-point range (total 7-35 points) with the lowest score on the first six items indicating greater spirituality.17 The SOL scale focuses on internal spiritual practices and experiences, with the exception of item 7, which inquires about frequency of attendance at spiritual or religious gatherings.17,18 The internal consistency—Cronbach’s alpha—of the SOL is 0.86.17
Belief in God. The patients were asked if they believe in God (yes/no) to identify believers versus non-believers.
Study procedures. The patients were clinically treated for their depression with one of three SSRIs: escitalopram, sertraline, or paroxetine. The choice of treatment was based on clinical grounds, incorporating factors such as history of previous response and potential side effects, with the hope of achieving the best possible results for the patient. After eight weeks of treatment with one of the above SSRIs, the patients were evaluated again using the MADRAS, the BHS, and the DAS.
Statistical analysis. Demographic variables such as age, onset of illness, gender, whether this was a first major depressive episode, and the dose for each individual medication, were tabulated. The MADRAS, BHS, and DAS were examined pretreatment, post-treatment, and with respect to change scores, and compared between believers versus non-believers. A Univariate analysis was used since Levine’s test of equality demonstrated that the error variance were equal across each respective group for MADRAS, BHS, and DAS scores. Since the prescores of the MADRAS, BHS, and DAS for believers were each significantly different from non-believers, the pre-scores were used as a covariant in each analysis. The SOL scale correlation with changes in the MADRAS, BHS, and DAS scales, was examined. P-values less than 0.05 were considered as statistically significant. Statistical analysis was performed using SAS version 9.1 for Windows (SAS Institute Inc., Cary, NC, USA, 2003).
RESULTS
Demographic variables for believers (N=68) versus non-believers (N=16) are shown in Table 1. The percentage of individuals who reported a belief in God in this sample was 81 percent (this is lower than the 92% of Americans who reported that they believe in God19). There were no significant differences with respect to age, age of onset of illness, number of years ill, and whether this depressive illness was a first. There was, however, a difference in gender distribution between the two groups in that more men were non-believers than women (31.4% of men vs. 10.2% of women; t=2.50, p<0.02). Of note, this disparity is also seen in national averages in which consistently more men than women were identified as non-believers.19 Patients received one of three antidepressants: escitalopram (N=34), sertraline (N=28), or paroxetine (N=22).
TABLE 1.
Demographic characteristics of believers vs. non-believers
| DEMOGRAPHICS | BELIEVERS N=68 | NON-BELIEVERS (N=16) | SIGNIFICANCE |
|---|---|---|---|
| Age | 40.1 (SD 15.1) | 40.3 (SD 15.5) | t=0.04 NS |
| Gender | 24 men/44 women | 11 men/5 women | t=2.50, p<0.02* |
| Age of onset | 30.0 (SD 11.3) | 33.1 (SD 15.5) | t=0.89 NS |
| Years ill | 10.1 (SD 12.3) | 7.1 (SD 12.3) | t=0.91 NS |
| First episode? (yes/no) | 31 yes/33 no | 9 yes/7 no | t=0.89 NS |
| DOSE OF MEDICATION | |||
| Escitalopram | 19.4 (SD 5.6), N=27 | 18.6 (SD 6.3), N=7 | t=0.36 NS |
| Sertraline | 187.0 (SD 42.6), N=19 | 195.0 (SD 57.0), N=5 | t=0.36 NS |
| Paroxetine | 45.0 (SD 5.6), N=22 | 50.0 (SD 5.0), N=4 | t=1.22 NS |
Statistically significant; NS: not significant
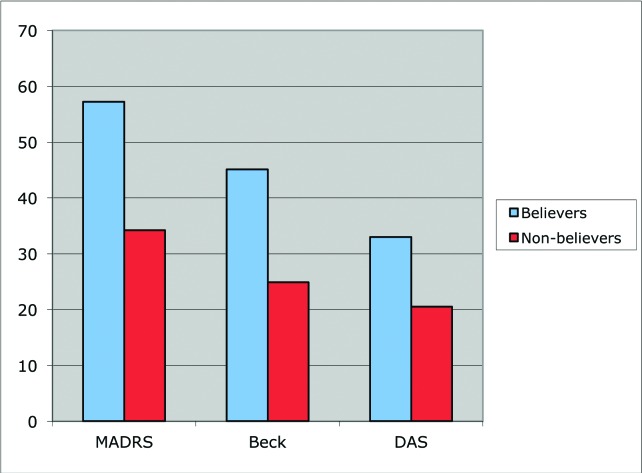
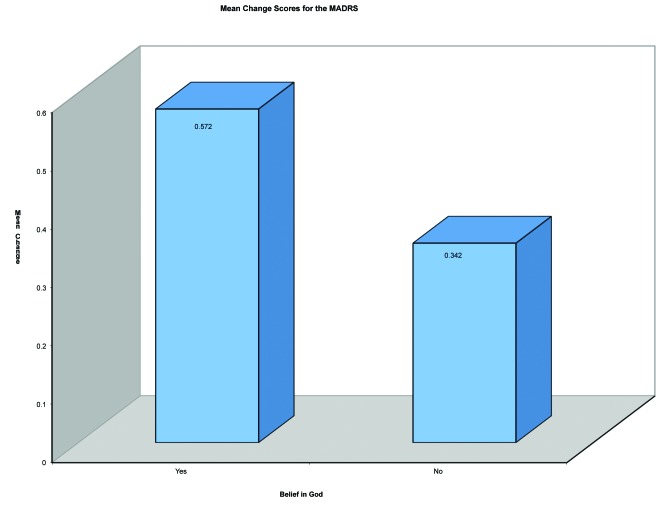
At baseline, the mean MADRAS pre-score for believers was 24.29 vs. 31.06 for non-believers (F=19.485, df=1, 82, p<0.0001) (i.e., believers were significantly less depressed compared to non-believers before treatment). Univariate analyses showed that the MADRAS, BHS, and DAS score changes were more significant for those people who were believers (N=68) compared to non-believers (N=16) as depicted in Figure 1. Believers had a significantly greater mean change score (57% decrease) than non-believers (34% decrease) (F=4.41, df=1, 81, p<0.01) as shown in Figure 2.
FIGURE 1.
Percent changes in mean MADRS scores, BHS scores and DAS scores for believers vs. non-believers
FIGURE 2.
Mean change in MADRS score for believers vs. non-believers
The BHS prescores for believers were significantly lower from non-believers (average BHS prescore for believers was 12.56 vs. 14.94 for non-believers (F=16.255, df=1.82, p<0.0001). The BHS change scores showed no significant differences between believers and non-believers (F=2.099, df= 1.81, p=0.151). Believers however, did have a numerically higher mean change score (43.7% decrease) than non-believers (30.8% decrease).
The DAS pre-scores were significantly lower in believers compared to non-believers; average DAS pre-score for believers was 163.43 versus 191.63 for non-believers (F=19.419, df=1, 82, p<0.0001). There was no significant difference between the DAS change scores for believers and non-believers (F= 1.135, df=1, 81, p=0.290). Believers, however, had a numerically higher mean change score (32.0% decrease) than non-believers (24.7% decrease).
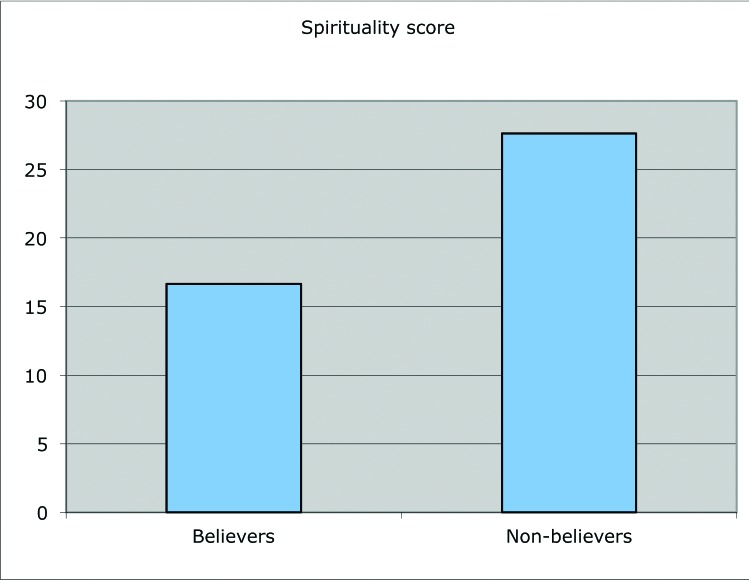
With respect to the SOL scale score (where lower score meaning greater spirituality), believers had a lower score than non-believers; mean score 16.64 (SD=4.2) vs. 27.63 (SD=2.2). This difference was highly significant (t=10.07 p<0.0001) (Figure 3).
FIGURE 3.
Mean spirituality scores for believers vs. non-believers (lower SOL scores denote higher spirituality)
A correlational analysis between the SOL score and the MADRAS, BHS, and DAS pre-scores, post-scores, and change scores were all significant. There was a significant negative correlation between the MADRAS change score and SOL score (r=-0.41, p<0.0001); the BHS change score and SOL score (r=-0.447, p<0.0001); and the DAS change score and SOL score (r=-0.392, p<0.0001). The lower SOL score signified a greater degree of spirituality, which correlated with a higher change score. Correlations between the prescores of the MADRAS (r=0.452, p<0.0001) the BHS (r=0.488, p<0.0001) and DAS (r=0.542, p<0.0001) were all significantly positively correlated with the spirituality score. Correlations between the post-scores of the MADRAS (r=0.525, p<0.0001), the BHS (r=0.538, p<0.0001) and DAS (r=0.532, p<0.0001) were also significantly positively correlated with the SOL score.
The change scores of the MADRAS, BHS, and DAS were unrelated to the particular medication taken when compared in separate one-way ANOVAs (p=0.681, p=0.854, and p=0.884, respectively).
DISCUSSION
At presentation, even with a diagnosis of depression, the patients in our study who reported greater spirituality had significantly lower measures of hopelessness, dysfunctional attitudes, and depressive symptoms. This suggests that greater spirituality is associated with less severe depression and possibly a lower morbidity from depressive illness. Moreover, the degree to which each of these measures improved over the course of eight weeks was significantly greater for those patients who were more spiritual according to MADRAS scores. However, a belief in God did not correlate with a significant change in hopelessness or dysfunctional attitudes, although the mean change in scores was numerically greater for believers.
It is important to note that the spirituality scale used in this study, the SOL, attempts to measure ‘intrinsic”religiosity,’ which is like the spiritual aspect of religion. Intrinsic religiosity is the inner spiritual framework that endows life with meaning and guides behavior and choices. “Extrinsic religiosity,” on the other hand, is the visible and outward signs of religious devotion, which may or may not correlate with inner beliefs.20 Prior studies exploring the relationship between spirituality and depression have shown similar results for intrinsic religiosity and spirituality and have identified that both are negatively associated with depression. For instance, McCullough et al6 found that those with high levels of “intrinsic religious motivation,” “religious salience,” and religious involvement were at reduced risk for depression.6
Comparable trends were also found among those with health problems. Nelson et al,7 in studying terminally ill cancer and acquired immunodeficiency syndrome (AIDS) patients, described a substantial negative association between intrinsic religiosity and depression.7 Moreover, Koenig et al5 have shown that in medically ill older patients, greater intrinsic religiosity predicted a shorter time to recovery from a depressive episode. Koenig et al21 also looked specifically at intrinsic religiosity as well as frequency of church attendance and private religious activities and found that only intrinsic religiosity was significantly related to shorter time to depression remission. Simoni et al,8 who found that spirituality scores were negatively correlated with depression in a group of human immunodeficiency virus (HIV)-positive Puerto Rican women, also found in their study that church attendance/membership, though often associated with spirituality, did not correlate with lower depression scores. To further demonstrate this, Nelson et al,7 in their assessment of the terminally ill, found no relationship between extrinsic religiosity and depression. Though religion comprises spirituality, the aforementioned studies show that the two affect depression in varying ways and to different degrees. While intrinsic religiosity overlaps with spirituality and produces similar results, extrinsic religiosity seems to have much less of a correlation.
Surprisingly, our findings were in contradiction to Schettino et al,22 who reported no significant associations between spirituality and treatment response; however, they found a strong curvilinear relationship between religiosity and treatment response, i.e., a moderate level of religiosity (as opposed to lower or higher levels), was significantly associated with greater reduction in depressive symptom severity and more likelihood of remission. This might be due to the methodology of spirituality measurement, where in our study the SOL captured spirituality, intrinsic religiosity, and orientation to both life and God, rather than focusing on only one’s relationship with God. Zinnbauer et al10 emphasized that the sacred is not only restricted to God, but can also include other significant objects that are transformed when explicitly imbued with divine qualities, which would make the SOL a more inclusive measure.
Several studies have attempted to identify the mediating factors between depression and spirituality. For example, Simoni et al8 suggested that increased self-esteem and an increased sense of mastery were particularly important, while Murphy et al23 identified lower levels of hopelessness associated with religious beliefs as being directly related to less depression. Likewise, Koenig et al21 suggested that depression is offset by “religious coping” explained as “the use of religious beliefs or behaviors to facilitate problem-solving to prevent or alleviate the negative emotional consequences of stressful life circumstances.” While our study showed that both belief in God and greater spirituality correlated with a significant decrease in depression, only spirituality was associated with a decrease in hopelessness and dysfunctional attitudes, once again stressing that spirituality is not just associated with God or a higher being. We found that in individuals with greater spirituality, a response to treatment includes both an improvement in mood and greater hopefulness.23 Our analysis does not allow us to attribute causation to spirituality, but there is room to theorize about the nature of the relationship between these entities. The search for the sacred, which defines spirituality, can encompass anything from higher powers to psychological attributes;10 thus, it could be worth taking a closer look at how the different classes that comprise the sacred, perhaps faith and meaning, affect depression.
Griffith24 highlighted the important goal for clinicians to be “spiritually informed” about the role of spirituality and religion in patients’ lives, and emphasized the effort that needs to be made to understand how patients describe and experience faith. Solomon25 suggested that faith offers hope, and there may be a synergistic relationship between spirituality and resolving depression mediated by greater hopefulness.25 Furthermore, based on Fowler’s idea of the Stages of Faith,26 one’s faith is constantly changing depending on one’s stage of development in life and as one gains more knowledge and experience, which makes it harder and more complicated to measure faith.
On the other side, meaning is a more universal concept. Frankl, who worked through four Nazi death camps and suffered from the loss of his family, believes that life is a “quest for meaning” and suffering leads to a need for such, for “suffering ceases to be suffering at the moment it finds a meaning.”27 To further emphasize this, Breibart et al28 believe that spirituality and meaning buffer against depression, hopelessness, and the wish for an accelerated death among terminally ill end-of-care patients. Because different components of the sacred seem to create differing effects, it may be beneficial for a future study to focus on the finer distinctions of spirituality.
The above findings suggest that an assessment of spiritual beliefs and encouraging discussion of spirituality would need to play a more active role in treatment of depression. Asking patients what goals they would set for themselves for a more meaningful life was identified as one of the ways to do this.29 Moreover, Lomax et al30 advocate for the adoption of the spiritual assessment as a core competency for psychotherapy education during training of future generations of psychiatrists. Therefore, we may need to help our patients, as appropriate, to explore their own spiritual beliefs, to endow life with ultimate meaning in order to obtain the maximum benefits from the treatments that we offer.
Limitations. There are several shortcomings of our study, which should be taken into account. The study had a limited sample size, and the population is largely Caucasian living in the Northeast; thus, these results may not be generalizable to other populations. Furthermore, we did not continue to assess the patients beyond the initial treatment phase, and thus cannot comment whether the improvement in depression, dysfunctional attitudes, and hopelessness were sustained over time. Finally, we cannot identify what it is about spirituality or intrinsic religiosity that mediates this improvement or whether this factor is in fact causative.
CONCLUSION
Spirituality can constitute a system of meaning that emphasizes hope, adaptation, insight, and the belief that circumstances are not senseless or meaningless. The study findings suggest that greater spirituality is associated with less severe depression. Moreover, the degree to which the measures of depressive symptom severity, hopelessness, and cognitive distortions improved over the course of eight weeks was significantly greater for those patients who were more spiritual. Given the above study and literature findings, mental health professionals might consider including an assessment of spiritual beliefs and encourage discussion and use of spirituality to improve treatment outcome of depression.
ACKNOWLEDGMENT
The authors wish to acknowledge the contributions of Dr. Nawara Y. Dawoud to the evolution of this manuscript.
Footnotes
FUNDING:There was no funding for the development and writing of this article.
FINANCIAL DISCLOSURES:None of the authors have a conflict of interest in the conduct and reporting of this study. Dr. IsHak has received grants in associated research areas as listed below: NARSAD on Quality of Life in Major Depression, Pfizer Monotherapy in Major Depression, that ended on December 31st, 2011.
References
- 1.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 2.Hassed CS. Depression: dispirited or spiritually deprived? Med J Aust. 2000;173:545–547. doi: 10.5694/j.1326-5377.2000.tb139326.x. [DOI] [PubMed] [Google Scholar]
- 3.Curlin FA, Odell SV, Lawrence RE, et al. The relationship between psychiatry and religion among US. physicians. Psychiatr Serv. 2007;58:1193–1198. doi: 10.1176/appi.ps.58.9.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gartner J, Larson D, Allen G. Religious commitment and mental health: a review of the empirical literature. J Psychol Theol. 1991;19:6–25. [Google Scholar]
- 5.Koenig H, George L, Peterson B. Religiosity and remission of depression in medically ill older patients. Am J Psychiatry. 1998a;155:536–542. doi: 10.1176/ajp.155.4.536. [DOI] [PubMed] [Google Scholar]
- 6.McCullough M, Larson D. Religion and depression: a review of the literature. Twin Research. 1999;2(2):126–136. doi: 10.1375/136905299320565997. [DOI] [PubMed] [Google Scholar]
- 7.Nelson CJ, Rosenfeld B, Breitbart W, Galietta M. Spirituality, Religion and Depression in the Terminally Ill. Psychosomatics. 2002;43:213–220. doi: 10.1176/appi.psy.43.3.213. [DOI] [PubMed] [Google Scholar]
- 8.Simoni JM, Ortiz MZ. Mediational models of spirituality and depressive symptomatology among HIV-positive Puerto Rican women. Cultur Divers Ethnic Minor Psychol. 2003 Feb;9(1):3–15. doi: 10.1037/1099-9809.9.1.3. [DOI] [PubMed] [Google Scholar]
- 9.Balbuena L, Baetz M, Bowen R. Religious attendance, spirituality, and major depression in Canada: a 14-year follow-up study. Can J Psychiatry. 2013;58(4):225–32. doi: 10.1177/070674371305800408. [DOI] [PubMed] [Google Scholar]
- 10.Zinnbauer BJ, Pargament KI, Scott AB. The emerging meanings of religiousness and spirituality: Problems and prospects. J Pers. 1999;67(6):889–919. [Google Scholar]
- 11.Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality: implications for physical and mental health research. Psycholog Relig Spritual. 2008;S(1):3–17. doi: 10.1037/0003-066x.58.1.64. [DOI] [PubMed] [Google Scholar]
- 12.Pargament KI. The Psychology of Religion and Coping. New York: Guilford Press; 1997. [Google Scholar]
- 13.Williams JB, Gibbon M, First MB, et al. The Structured Clinical Interview for DSM-III-R (SCID). II. multisite test-retest reliability. Arch Gen Psychiatry. 1992;49(8):630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- 14.Asberg M, Montgomery SA, Perris C, et al. A comprehensive psychopathological rating scale. Acta Psychiatr Scand Suppl. 1978;(271):5–27. doi: 10.1111/j.1600-0447.1978.tb02357.x. [DOI] [PubMed] [Google Scholar]
- 15.Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42(6):861. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 16.Beck AT, Brown G, Steer RA, Weissman AN. Factor analysis of the dysfunctional attitude scale in a clinical population. Psychologic Assess. 1991;3:478–483. [Google Scholar]
- 17.Goldfarb LM, Galanter M, McDowell D, et al. Medical student and patient attitudes toward religion and spirituality in the recovery process. Am J Drug Alcohol Abuse. 1996;22(4):549–561. doi: 10.3109/00952999609001680. [DOI] [PubMed] [Google Scholar]
- 18.Galanter M, Dermatis H, Bunt G, et al. Assessment of spirituality and its relevance to addiction treatment. J Subst Abuse Treat. 2007;33(3):257–264. doi: 10.1016/j.jsat.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 19. [December 1, 2013]. http://www.gallup.com/poll/147887/americans-continue-believe-god.aspx Gallup Poll May 5-8, 2011. More than 9 in 10 Americans continue to believe in God. Princeton, NJ: Gallup Organization; 2011.
- 20.Donahue MJ. Intrinsic and extrinsic religiousness: review and meta-analysis. J Pers Soc Psychol. 1985;48(2):400–419. [Google Scholar]
- 21.Koenig H, Parament K, Nielsen J. Religious coping and health status in medically ill hospitalized older adults. J Nerv Ment. 1998b;186:513–521. doi: 10.1097/00005053-199809000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Schettino JR, Olmos NT, Myers HF, et al. Religiosity and treatment response to antidepressant medication: a prospective multi-site clinical trial. Ment Health Relig Cult. 2011;14(8):805–818. doi: 10.1080/13674676.2010.527931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murphy PE, Ciarocchi JW, Piedmont RL, et al. The relation of religious belief and practices, depression, and hopelessness in persons with clinical depression. J Consult Clin Psychol. 2000;68(6):1102–1106. [PubMed] [Google Scholar]
- 24.Griffith LJ. Brief supportive psychotherapy for a patient with chronic. schizophrenia who is dying. Psychiatry (Edgmont). 2007;4(12):49–54. [PMC free article] [PubMed] [Google Scholar]
- 25.Solomon A. The Noonday Demon: An Atlas of Depression. First Touchstone Edition. New York: Simon & Schuster; 2002. [Google Scholar]
- 26.Fowler JW. Stages of Faith: The Psychology of Human Development and the Quest for Meaning. New York: Harper & Row; 1981. [Google Scholar]
- 27.Frankl V. Man’s Search for Meaning. Masachusetts: Beacon Press; 2006. [Google Scholar]
- 28.Breibert W, Gibson C, Poppito SR, et al. Psychotherapeutic interventions at the end of life: a focus on meaning and spirituality. Can J Psychiatry. 2001;49(6):366–372. doi: 10.1177/070674370404900605. [DOI] [PubMed] [Google Scholar]
- 29.Galanter M. Spirituality and the Healthy Mind: Science, Therapy and the Need for Personal Meaning. New York: Oxford University Press, Inc.; 2005. [Google Scholar]
- 30.Lomax JW, 2nd, Karff RS, McKenny GP. Ethical considerations in the integration of religion and psychotherapy: three perspectives. Psychiatr Clin North Am. 2002;25(3):547–559. doi: 10.1016/s0193-953x(01)00015-6. [DOI] [PubMed] [Google Scholar]