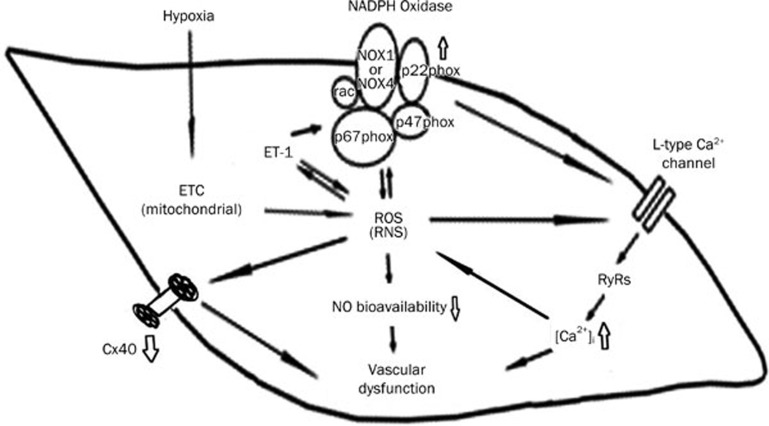
Figure 7.
The mechanisms underlying the abnormal vascular activity in hypoxic pulmonary artery. Hypoxia promotes the genesis of ROS from the electron transport chain (ETC) at mitochondria, and thereafter, increases ET-1. ET-1 activates NADPH oxidase which contains catalytic (NOX1-4) and modulating subunits (p22phox, p47phox, and p67phox). An increased ROS stimulates the L-type Ca2+ channels to increase calcium influx and subsequent intracellular Ca2+ release from RyRs. Increased [Ca2+]i in turn stimulates the formation of ROS. ROS serves as an inducer for activating NADPH oxidase, therefore, blocking calcium influx is able to suppress NADPH oxidase. An increase in ET-1 and NADPH oxidase play key roles in the development of hypoxia pulmonary hypertension. A reduction in NO availability and release contributes to abnormal activity of hypoxic pulmonary artery. CPU86017-RS relieves hypoxic pulmonary arterial abnormality via blocking NADPH oxidase and calcium influx in the vasculature.