Abstract
Background
The current study seeks to investigate the mechanisms through which mindfulness is related to mental health in a clinical sample of adults by examining a) whether specific cognitive emotion regulation strategies (rumination, reappraisal, worry, and non-acceptance) mediate associations between mindfulness and depression and anxiety, respectively, and b) whether these emotion regulation strategies operate uniquely or transdiagnostically in relation to depression and anxiety.
Methods
Participants were 187 adults seeking treatment at a mood and anxiety disorders clinic in Connecticut. Participants completed a battery of self-report measures that included assessments of depression and anxiety (Mood and Anxiety Symptom Questionnaire), and emotion regulation (Ruminative Response Scale, Penn State Worry Questionnaire, Emotion Regulation Questionnaire, Difficulties in Emotion Regulation Scale).
Results
Simple mediation analyses indicated that rumination and worry significantly mediated associations between mindfulness and anxiety symptoms, while rumination and reappraisal significantly mediated associations between mindfulness and depressive symptoms. Multiple mediation analyses showed that worry significantly mediated associations between mindfulness and anxiety symptoms and rumination and reappraisal significantly mediated associations between mindfulness and depressive symptoms.
Conclusion
Findings suggest that mindfulness operates through distinct and common mechanisms depending on clinical context.
Keywords: Mindfulness, Emotion Regulation, Depression, Anxiety
Mindfulness, the process of attending to present-moment sensations and experiences with a non-judgmental stance [1], has been consistently associated with lower rates of depression and anxiety and greater well-being [1–7]. Empirically-validated treatments for anxiety and depression that incorporate aspects of mindfulness practice have demonstrated good effect sizes for treatment outcomes [6]. In many new wave interventions, mindfulness skills are assumed to constitute a set of foundational or “core” abilities that promote the use of other cognitive or behavioral skills [8–10]. Despite the widespread acceptance of mindfulness principles within clinical practice, the precise mechanisms through which mindfulness is associated with symptoms of depression and anxiety are still not well understood.
Emotion regulation, which has received increasing support as a transdiagnostic process [11, 12], may be one pathway through which mindfulness promotes mental health. Emotion regulation has been conceptualized as processes through which individuals modulate their emotions in response to environmental demands in the service of goal s [13–18]. There is abundant evidence linking emotion regulation difficulties with psychopathology, and particularly with internalizing disorders such as depression and anxiety [11, 12]. There is also increasing evidence amassed mostly from community samples that trait mindfulness is associated with less use of maladaptive emotion regulation strategies [19–21] and reduced physiological emotional responding in the presence of stress [22]. Transdiagnostic models of emotion regulation suggest that particular emotion regulation skills may contribute to different forms of psychopathology [12]. Drawing from this framework, emotion regulation strategies might serve as the link between low mindfulness and anxiety or depression or they might operate as transdiagnostic mechanisms.
The present study addresses gaps in the literature linking mindfulness to symptoms of psychopathology by comparing possible emotion regulatory mechanisms through which mindfulness may be associated with depression and anxiety symptoms in a clinical sample of adults. In particular, we were interested in four emotion regulation strategies that have been associated with depression and anxiety and may be particularly relevant to mindfulness: reappraisal, non-acceptance, rumination, and worry.
The positive impact of mindfulness might occur through the process of reappraisal, as recently discussed by several others [23, 24]. Reappraisal involves reframing an emotion-eliciting experience or stimulus (usually negative) in a manner that alters the impact of that experience [16]. The tendency to use this emotion regulation strategy is associated with lower rates of depression and anxiety [25]. Mindfulness practice in community samples has been associated with increases in positive reappraisal, with these increases mediating reductions in stress [24]. Though developing reappraisal skills is not a specific goal of mindfulness practice, taking a nonjudgmental stance toward experience is in itself a form of reframing that may cultivate a more general tendency toward reappraisal of initial negative cognitions. This non-evaluative, nonjudgmental reappraisal or reframing may then lead to improvements in depression and anxiety symptoms [20; 26, 27].
Additional emotion regulation strategies that might underlie the processes through which mindfulness attenuates symptoms are rumination and worry, both of which involve cognitive overengagement in attempt to control or attenuate unpleasant emotional experiences. Rumination is characterized by repetitive thoughts about negative emotional experience, including contributing factors and potential consequences of the experience [28]. Higher levels of rumination have been frequently associated with lower levels of trait mindfulness [29, 30, 31] and with higher levels of depression and anxiety in community samples [32]. Furthermore, following a trial of Mindfulness-based Cognitive Behavioral Therapy (MBCT), reductions in rumination and increases in mindfulness mediated treatment effects on depressive symptoms in a community sample with remitted major depressive disorder [33]. Similarly, completing a course of Mindfulness-based Stress Reduction (MBSR) appears to increase levels of trait mindfulness and decrease levels of rumination in community samples [34, 35], changes that may be inversely correlated with sufficient statistical power [35]. The nonjudgmental aspect of mindfulness may mitigate the abstract self-evaluative thoughts characteristic of rumination (e.g., “Why do things turn out the way they do?”) [32], thereby reducing depression and anxiety.
Worry and rumination may also be mitigated by the emphasis on the present moment in mindfulness. The orientation to present circumstances encouraged in mindfulness practice is antithetical the focus on past failures in rumination [32] and the focus on future threats characteristic of worry [36]. Higher levels of self-reported trait mindfulness have been associated with less worry in community samples [37], and increases in mindfulness following mindfulness training have been associated with decreases in frequency and duration of worry [38, 39], as well as with physiological indices of worry such as respiratory rate [38]. Moreover, worry is a central feature of anxiety disorders [40], suggesting that decreases in frequency or severity of worry are associated with decreases in anxiety symptoms, including physiological arousal levels.
Non-acceptance of emotional experience, which has been described as a tendency to have negative meta-reactions to negative emotions [15] and as a tendency to avoid experiencing aversive emotions (i.e., anxiety, sadness) [1; 41] may also function as a mechanism through which mindfulness influences symptoms. Several studies of clinical and community samples have shown that increases in trait mindfulness are associated with decreases in non-acceptance of aversive emotion [22; 29, 30]. Participants who underwent a mindfulness manipulation (vs. unfocused attention) also showed greater wiliness to view upsetting images, suggestive of decreased emotional non-acceptance [22]. In turn, non-acceptance of emotional responses has been associated with higher levels of psychopathology, including anxiety and panic [42–44]. For example, non-acceptance of emotional responses has been highly associated with generalized anxiety disorder diagnosis [7, 45], and non-acceptance of emotions has been found to predict comorbidity between generalized anxiety disorder (GAD) and social anxiety disorder (SAD) [46].
The current study had two aims: a) to examine whether specific cognitive emotion regulation strategies (i.e., reappraisal, acceptance, rumination, and worry) mediate associations between mindfulness and depression and anxiety symptoms, respectively; b) to examine whether these emotion regulation strategies operate specifically or transdiagnostically in linking mindfulness with depression and anxiety symptoms. Our hypotheses were that rumination, which has been shown to operate as a transdiagnostic factor in anxiety and depression [47, 48], would be a common mechanism through which (lack of) mindfulness influences both anxiety and depression. Given that reappraisal has also been associated with fewer symptoms of both anxiety and depression [24, 25], we predicted that reappraisal would operate as a transdiagnostic mediator of mindfulness. In contrast, we hypothesized that non-acceptance would be mostly associated with anxiety symptoms because difficulty accepting and/or avoidance of threatening stimuli has been more strongly linked to anxiety than depression [43, 46]. We similarly hypothesized that worry would show specificity as a mediator of mindfulness and anxiety given its strong theoretical and empirical connection to anxiety [39].
Most previous studies of mindfulness and emotion regulation have used non-clinical samples. The current study utilized a clinical sample to investigate the generalizability of previous findings to treatment-seeking populations and to test our hypotheses in individuals suffering more intense symptoms of depression and anxiety. To maximize statistical power to examine meditational effects, we examined depression and anxiety symptoms with dimensional measures.
Method
Participants
The sample consisted of 187 adults ages 18–71 (M=38, SD=14.2) seeking treatment at a mood and anxiety disorders clinic in Connecticut. Participants identified as white (non-Hispanic; 78.8%), African-American (7.4%), Hispanic (8.5%), and ‘other’ (3.7%). Women comprised 64.6% of the sample.
Procedure
Participants completed a series of self-report measures assessing presenting symptoms and were administered a structured clinical interview for DSM-IV Axis I disorders (SCID-I) [49] by advanced doctoral student clinicians at intake. Diagnoses were reviewed by supervising psychologists and determined by consensus diagnosis using clinician severity ratings (CSR), as suggested by the Anxiety Disorders Interview Schedule (ADIS) [50]. Nearly all participants met criteria for at least one Axis I disorder (96%). The average clinical severity rating (CSR) was 5.3, with 95% of the sample scoring above the clinical mean CSR. The most prevalent Axis I diagnoses were generalized anxiety disorder (42.9%), major depressive disorder (20.1%) and social phobia (12.2%). Though Axis I diagnoses fell almost exclusively within the spectrum of mood and anxiety disorders, 5% of participants met criteria for other Axis I disorders (i.e., eating disorders, adjustment disorders).
All study procedures were conducted according to ethical principles outlined by the American Psychological Association. An Institutional Review Board approved the study and informed consent was obtained from participants prior to inclusion. Participants were not remunerated.
Measures
Anxiety symptoms were measured using the anxious arousal (AA) subscale of The Mood and Anxiety Symptom Questionnaire (MASQ) [51], which consists of 17 items assessing symptoms of physiological tension and hyperarousal specific to anxiety (e.g., “Startled easily”, “Hands were shaky”). We used the anxious arousal scale because this dimension best distinguishes anxiety from depression [52] and does not include items assessing worry. Depression symptoms were measured using the anhedonic depression (AD) subscale of the MASQ, which consists of 22 items measuring symptoms of anhedonia and low positive affect characteristic of depression (e.g., “Felt withdrawn from other people”). Again, we used the AD subscale because this dimension best distinguishes depression from anxiety [52]. For both subscales, participants rate how much they have experienced symptoms during the past month on a five-point Likert scale ranging from 1 (not at all) to 5 (extremely). The MASQ has shown good convergent and discriminant validity and reliability [52]. Internal consistency for the AA and AD subscales was good (α=.87).
Worry was measured using The Penn State Worry Questionnaire (PSWQ) [53], a 16-item inventory assessing frequency, severity, and perceived uncontrollability of worry. Participants rate how “typical or characteristic” each statement is of themselves on a 5-point Likert scale ranging from 1 (not at all typical) to 5 (very typical). The PSWQ has demonstrated strong internal consistency (α=.95) and good test-retest reliability [53]. Internal consistency in the current study was high (α=.92).
Rumination was measured with the The Ruminative Response Scale (RRS) [54] using the brooding subscale, which is composed of 5 items assessing the tendency towards repetitive, negative thinking (e.g., “I think about a recent situation, wishing it could have gone better”). Participants rate the frequency with which they use ruminative strategies using a 4-point Likert scale ranging from 1 (never) to 4 (always), and higher scores reflect higher frequencies of brooding [55]. The RRS has demonstrated high internal consistency (α=.89) [56]. Internal consistency for the brooding subscale in the current sample was good (α=.78).
Non-acceptance was measured using the non-acceptance subscale of The Difficulties in Emotion Regulation Scale (DERS) [15], which consists of 6-items assessing acceptance of emotional experience (e.g., “when I’m upset, I become irritated with myself for feeling that way”). Participants indicate how much each item applies to them on a 5-point scale ranging from 1 (not at all) to 5 (almost always). Higher scores indicate higher levels of difficulty accepting emotions [15]. The non-acceptance subscale has demonstrated high internal consistency (α=.85) [15], and internal consistency in the current study was high (α=.89).
Reappraisal was measured using the cognitive reappraisal subscale of the Emotion Regulation Questionnaire (ERQ) [57], which consists of 6 items assessing ability to positively reframe distressing emotional experience (e.g., “when I want to feel less negative emotion, I change what I’m thinking about). Participants rate the degree to which they use each strategy using a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree), and higher scores reflect higher use of reappraisal. The reappraisal subscale has demonstrated adequate internal consistency (α=.79). Internal consistency in the current study was very good (α=.91).
Mindfulness was measured with the total scale of The Five Facet Mindfulness Questionnaire (FFMQ) [19], a 39-item questionnaire assessing mindfulness in daily life. The FFMQ measures specific dimensions of mindfulness (e.g., nonreactivity, observing, acting with awareness, nonjudging, and describing) as well as overall mindfulness. Items are rated on a 5-point Likert-type scale, ranging from 1 (never or very rarely true) to 5 (very often or always true). To obtain an overall measure of mindfulness, all 39 items are summed, and higher scores reflect higher levels of self-reported mindfulness. The FFMQ has shown moderate to high internal consistency in non-meditators (α=.75–.91) [19]. Internal consistency for the FFMQ total scale was high in the current sample (α=.89).
Data Analytic Strategy
The nonparametric bootstrapping method recommended by Preacher and Hayes [58] was utilized to test for direct and indirect effects of mindfulness on symptoms of depression and anxiety. Bootstrapping offers the advantage of generating an empirical approximation of the sampling distribution through resampling of the full data set without assuming indirect effects are normally distributed. Direct and indirect effects were tested based on bootstrapped standard errors, with 5,000 bootstrap samples. Point estimates of indirect effects were considered significant if 95 % confidence intervals did not contain zero.
Simple and multiple mediation models were constructed to examine emotion regulation variables (i.e., rumination, reappraisal, non-acceptance, and worry) as mediators of associations between mindfulness and depression and anxiety, respectively. Simple mediation analyses test only one proposed mediator at a time; therefore, finding a significant effect does not rule out alternative mechanisms that may be associated with the mediator but not represented in the model. Multiple mediation analyses include all hypothesized mediators in the model simultaneously, each serving as a control for the other. Thus, multiple mediation analysis isolates the most fundamental mechanisms that might operate above and beyond the effects of related variables. We examined both types of mediation to better understand which strategies relate trait mindfulness to depression and anxiety symptoms most fundamentally.
Results
Means and standard deviations and bivariate correlations for all variables for the total sample are displayed in Table 1. Independent samples t-tests revealed no significant differences in mean scores between males and females.
Table 1.
Summary of Intercorrelations, Means, and Standard Deviations for Mindfulness, Emotion Regulation Variables, Depression, and Anxiety
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Mindfulness | - | ||||||
| 2. Rumination | −.59** | - | |||||
| 3. Non-Acceptance | −.53** | .40** | - | ||||
| 4. Worry | −.39** | .32** | .26** | - | |||
| 5. Reappraisal | .61** | −.38** | −.22** | −.30** | - | ||
| 6. Depression | −.38** | .33** | .24** | .20** | −.35** | - | |
| 7. Anxiety | −.21** | .24** | .12 | .24** | −.15* | .26** | - |
| M | 117.58 | 13.48 | 16.08 | 62.66 | 22.59 | 76.39 | 30.84 |
| SD | 16.03 | 3.12 | 6.55 | 12.87 | 7.23 | 12.95 | 10.82 |
Note.
p < .05,
p < .01.
Results of simple mediation analyses for each cognitive emotion regulation variable are presented in Table 2. Of the possible mediators examined with respect to depression, rumination (point estimate of −.0780; CI: −.1507 to −.0069) and reappraisal (point estimate of −.0903; CI: −.1779 to −.0140) significantly mediated the direct effect of mindfulness. Indirect effects of non-acceptance and worry, respectively, were not significant. Of the possible mediators with respect to anxiety, rumination (point estimate of −.0664; CI: −.1315 to− .0075) and worry (point estimate of −.0491; CI: −.0981 to −.0140) significantly mediated the direct effect of mindfulness. Reappraisal and non-acceptance did not significantly mediate the association between mindfulness and anxiety.
Table 2.
Summary of simple mediation analyses for the relationships between mindfulness and depression and anxiety
| Mediating Variable (M) | Effect of IV on M (a) | Effect of M on DV (b) | Direct effects (c′) | Indirect effect (a x b) | Total effects (c) |
|---|---|---|---|---|---|
| Depression | |||||
| Rumination | −.115 | .668 | −.223 | −.077* | −.305 |
| Reappraisal | .277 | −.327 | −.214 | −.090* | −.305 |
| Worry | −.311 | .059 | −.287 | −.018 | −.305 |
| Non-Acceptance | −.212 | .111 | −.282 | −.024 | −.305 |
|
| |||||
| Anxiety | |||||
| Rumination | −.115 | .582 | −.078 | −.067* | −.145 |
| Reappraisal | .277 | −.033 | −.136 | −.009 | −.145 |
| Worry | −.311 | .159 | −.095 | −.049* | −.145 |
| Non-Acceptance | −.212 | .011 | −.143 | −.002 | −.145 |
Note.
Significant point estimates (p < 0.05) as determined by absence of zero within the confidence interval (see Preacher and Hayes, 2008).
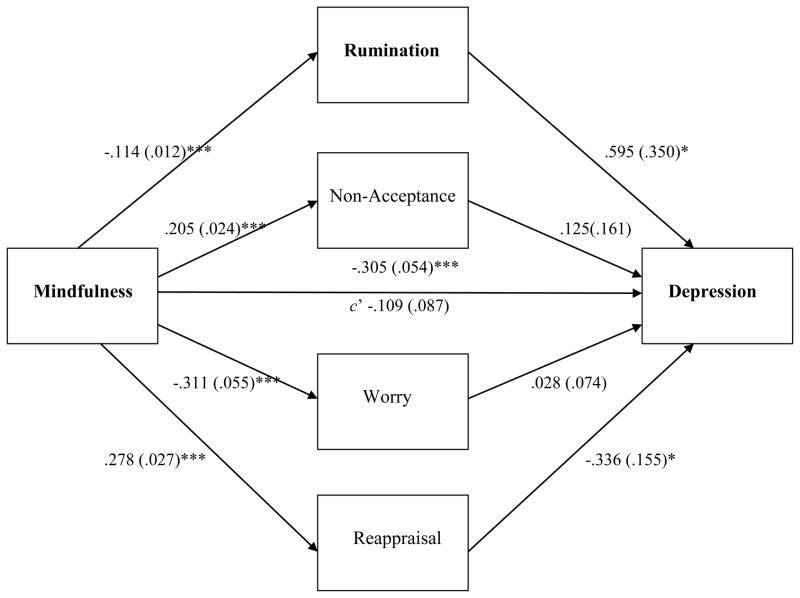
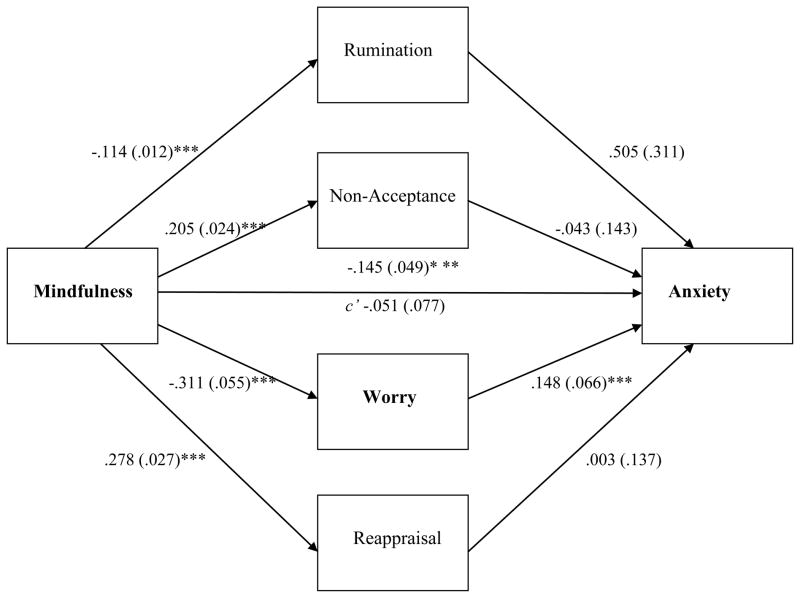
Figure 1 displays results of multiple mediation analyses examining rumination, reappraisal, worry, and non-acceptance simultaneously as mediators of associations between mindfulness and depression symptoms. The total indirect effect of mindfulness on depression through all four emotion regulation variables was significant (point estimate of −.1964; CI: −.3375 to −.0717). Regarding specific indirect effects of each emotion regulation variable in the multiple mediation model, rumination was a significant mediator of the effect of mindfulness on depression (point estimate of −.0670; CI: −.1445 to −.0038). Reappraisal was also a significant mediator of associations between mindfulness and depression (point estimate of −.0920; CI: −.1830 to −.0102). Figure 2 displays results of multiple mediation analyses examining rumination, reappraisal, worry, and non-acceptance as mediators of associations between mindfulness and anxiety symptoms. Again, the total indirect effect of mindfulness through the emotion regulation variables was significant (c= −.1448, p < .005). Analyses further revealed that when the four cognitive emotion regulation variables were entered as mediators simultaneously, only worry significantly mediated the influence of mindfulness on anxiety (point estimate of −.0447; CI: −.0932 to −.0130).
Figure 1.
Multiple Mediation Model for Mindfulness and Depression via Emotion Regulation. Unstandardized path coefficients and SE indicated above. The coefficient appearing above the line connecting mindfulness and depression represents the original path before mediators were added to the model. Significant indirect pathways are boldfaced. *** p <.001, * p < .05.
Figure 2.
Multiple Mediation Model for Mindfulness and Anxiety via Emotion Regulation. Unstandardized path coefficients and SE indicated above. The coefficient appearing above the line connecting mindfulness and anxiety represents the original path before mediators were added to the model. Significant indirect pathways are boldfaced. ***p < .001.
Discussion
The present study sheds further light on the mechanisms through which mindfulness is associated with mental health by showing that certain emotion regulation strategies significantly mediate the relationship between mindfulness and symptoms of depression and anxiety in a clinical sample of adults.
As hypothesized, rumination significantly mediated associations between mindfulness and both anxiety and depression when examined through simple mediation analysis. This finding is consistent with research indicating that rumination is a transdiagnostic factor in depression and anxiety [47, 48]. Theorists have argued that mindfulness practice may be a particularly potent antidote to rumination because rumination involves a self-critical questioning of one’s emotions and circumstances (e.g., “Why do I react the way I do?” and “Why do bad things happen to me?”) [28, 32]. The nonjudgmental, observing stance of mindfulness is antithetical to this self-critical questioning and may help ruminators disengage from it, thus reducing the effects of rumination on the maintenance of both depressive and anxiety symptoms [32, 59]. In addition, recent studies show that improving concrete thinking abilities and increasing experiential absorption in present experiences are critical for reducing rumination [59]. Mindfulness involves both of these processes in that it encourages individuals to observe and describe experiences in the present moment [1].
As predicted, in contrast to simple mediations, rumination showed specificity to depression symptoms in multiple mediation analyses. Worry and rumination share considerable conceptual overlap and are significantly correlated with each other [60]; both constructs can be considered forms of repetitive thinking involving overengagement with cognitions, but worry involves repetitive thinking and apprehensiveness about future negative outcomes, while rumination involves repetitive thinking about present and past negative events [61, 62]. This difference between results of simple vs. multiple mediations suggests that the transdiagnostic effects of mindfulness via reductions in rumination may stem from similarities between rumination and worry. Mindfulness may alleviate both depression and anxiety by combatting the repetitive or perseverative aspect of both types of thinking. However, when the unique aspects of worry and the other emotion regulation strategies are parceled out, reductions in rumination associated with mindfulness appear to be most relevant for depression and not anxiety.
Similarly, in multiple mediation analyses for mindfulness and anxiety, worry but not rumination emerged as a significant mediator, thus supporting our hypothesis that worry would demonstrate specificity as a mediator of mindfulness and anxiety. As worry has been highly implicated in anxiety disorders and anxiety symptoms [63–65] it is perhaps not surprising that when considering the relative contributions of all emotion regulation strategies, worry alone emerged as significant. We emphasize, however, that our measure of anxiety, the anxious arousal subscale of the MASQ, did not include items assessing worry. Although speculative, results suggest that mindfulness may reduce engagement informs of repetitive thinking (e.g., worry, rumination) in ways that have specific implications for anxiety and depression, respectively.
Our hypothesis for reappraisal was partially supported in that it significantly mediated depression but not anxiety symptoms. Results suggest that reappraisal may not operate as a transdiagnostic mediator of mindfulness. Findings for depression are consistent with previous studies indicating that reappraisal may mediate the influence of mindfulness on psychological distress [24] and with neuroimaging studies showing positive correlations between dispositional mindfulness and regions of the brain activated through reappraisal [66]. The cultivation of a nonjudgmental stance in mindfulness practice may aid depressed individuals in reconstruing the negative cognitions and emotions characteristic of depression as benign.
Contrary to our predictions, non-acceptance did not mediate associations between mindfulness and either anxiety or depression. Several interpretations are possible. Considering that 89.6%of our sample met DSM-IV criteria for an anxiety or depressive disorder diagnosis or both, it is possible that in populations exhibiting clinical levels of anxiety and depressive symptoms, non-acceptance is less salient a mechanism through which mindfulness attenuates symptoms. For these individuals, the intensity of symptoms, particularly physiological symptoms, may be overwhelming when focusing increased attention on them, rendering acceptance of aversive experience extremely difficult. This notion is also congruent with research showing increases in the observing component of mindfulness, which involves focusing attention on physiological experience, a re related to increases in anxiety [19; 67].
Alternatively, there may be nuanced differences between forms of acceptance that accounted for our results. Though acceptance plays a role in many evidence-based psychotherapies targeting anxiety (i.e., ACT, DBT), it is possible that non-acceptance is more relevant for mitigating symptoms of anxiety characterized by generalized cognitive distress and worry, rather than physiological symptoms of anxiety. In our study, non-acceptance was highly correlated with worry, but not anxious arousal, thus lending support to this possibility. Current findings on non-acceptance may also differ from previous findings due to differences in operational definitions and measurement scales. Many previous studies have assessed non-acceptance using the Acceptance and Action Questionnaire-II [AAQ-II; 68], while we used the DERS. Arguably, the AAQ-II conceptualizes acceptance as involving a more phenomenological willingness to experience distress, while the DERS, conceptualizes acceptance more cognitively, as the absence of negative meta-cognitions in response to one’s negative emotions. Future research might help clarify facets of acceptance and how they differentially relate to symptoms.
Limitations
Several study limitations warrant mention. Foremost, the cross-sectional design precludes causal interpretations of mediation analyses, and shared method variance due to reliance on self-report may have inflated observed relationships. Additionally, since our study examined symptoms of disorders rather than specific diagnoses, examine the same mechanisms with specific mood and anxiety disorders might be useful. Furthermore, as our study did not examine mechanisms of action following mindfulness-training, implications for mindfulness-based interventions are somewhat limited. Future studies should investigate whether self-reported trait mindfulness following mindfulness-training operates through similar mechanisms. Finally, generalizability of our results may also be limited because our sample was treatment-seeking and primarily Caucasian.
Conclusion
Findings of simple and multiple mediation analyses suggest that mindfulness impacts symptoms of depression and anxiety through both distinct and common emotion regulatory mechanisms. Rumination may be a mediating mechanism common to both anxiety and depression symptoms, operating transdiagnostically, while reappraisal may operate with specificity to depression symptoms and worry to anxiety symptoms. Taken together, findings highlight the importance of parceling out the unique components of emotion regulation processes to more precisely understand the mechanisms by which mindfulness attenuates symptoms of anxiety and depression.
References
- 1.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149:936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 2.Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10:125–143. [Google Scholar]
- 3.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2008;65:613–626. [Google Scholar]
- 4.Coffey KA, Hartman M, Frederickson BL. Deconstructing mindfulness and constructing mental health: Understanding mindfulness and its mechanisms of action. Mindfulness. 2010;1:235–253. [Google Scholar]
- 5.Greeson JM. Mindfulness Research Update: 2008. Complementary health practice review. 2008;14:10–8. doi: 10.1177/1533210108329862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hofman SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roemer L, Orsillo SM. Expanding our conceptualization of and treatment for generalized anxiety disorder: Integrating mindfulness/acceptance-based approaches with existing cognitive-behavioral models. Clinical Psychology: Science and Practice. 2002;9:54–68. [Google Scholar]
- 8.Linehan M. Cognitive behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- 9.Mennin DM, Fresco DM. Emotion regulation as an integrative framework for understanding and treating psychopathology. In: Kring AM, Sloan D, editors. Emotion Regulation and Psychopathology. New York: Guilford Press; 2010. pp. 356–379. [Google Scholar]
- 10.Hayes SC, McCurry SM, Afari N, Wilson KG. Acceptance and commitment therapy: A manual for the treatment of emotional avoidance. Reno, NV: Context Press; 1993. [Google Scholar]
- 11.Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Kring AM, Sloan DM. Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. New York: Guildford Press; 2010. [Google Scholar]
- 13.Campbell-Sills L, Barlow DH. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In: Gross JJ, editor. Handbook of emotion regulation. New York: Guilford Press; 2007. pp. 542–559. [Google Scholar]
- 14.Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: Methodological challenges and directions for child development research. Child Development. 2004;75:317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- 15.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology & Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- 16.Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998;2:271–299. [Google Scholar]
- 17.Gross JJ, Munoz RF. Emotion regulation and mental health. Clinical Psychology: Science and Practice. 1995;2:151–164. [Google Scholar]
- 18.Thompson RA. Emotion regulation: A theme in search of a definition. Monographs of the Society for Research in Child Development. 1994;59:25–52. [PubMed] [Google Scholar]
- 19.Baer RA, Smith G, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 20.Hill CLM, Updegraff JA. Mindfulness and its relationship to emotional regulation. Emotion. 2011:1–11. doi: 10.1037/a0026355. [DOI] [PubMed] [Google Scholar]
- 21.Roemer L, Lee JK, Salters-Pedneault K, Erisman SM, Orsillo SM, Mennin DS. Mindfulness and emotion regulation difficulties in generalized anxiety disorder: Preliminary evidence for independent and overlapping contributions. Behavior Therapy. 2009;40:142–154. doi: 10.1016/j.beth.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arch JJ, Craske MG. Laboratory stressors in clinically anxious and non-anxious individuals: The moderating role of mindfulness. Behaviour Research and Therapy. 2010;48:495–505. doi: 10.1016/j.brat.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Holzel BK, Lazar SW, Gard T, Schuman-Oliver Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6:537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- 24.Garland EL, Gaylord SA, Frederickson BL. Positive reappraisal mediates the stress-reductive effects of mindfulness: An upward spiral process. Mindfulness. 2011;2:59–67. [Google Scholar]
- 25.Martin RC, Dahlen ER. Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Personality and Individual Differences. 2005;39:1249–1260. [Google Scholar]
- 26.Carmody J. Evolving conceptions of mindfulness in clinical settings. Journal of Cognitive Psychotherapy. 2009;23:270–280. [Google Scholar]
- 27.Chambers R, Gullone E, Allen NB. Mindful emotion regulation: An integrative review. Clinical Psychology Review. 2009;29:56–572. doi: 10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 28.Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- 29.Kumar S, Feldman G, Hayes A. Changes in mindfulness and emotion regulation in an exposure-based cognitive therapy for depression. Cognitive Therapy Research. 2008;32:734–744. [Google Scholar]
- 30.Feldman G, Greeson J, Senville J. Differential effects of mindful breathing, progressive muscle relaxation, and loving-kindness meditation on decentering and negative reactions to repetitive thoughts. Behaviour Research and Therapy. 2010;48:1002–1011. doi: 10.1016/j.brat.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burg JM, Michalak J. The healthy quality of mindful breathing: Associations with rumination and depression. Cognitive Therapy and Research. 2011;35:179–185. [Google Scholar]
- 32.Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- 33.Shahar B, Britton WB, Sbarra DA, Figueredo AJ, Bootzin RR. Mechanisms of change in mindfulness-based cognitive therapy for depression: Preliminary evidence from a randomized controlled trial. International Journal of Cognitive Therapy. 2010;4:402–418. [Google Scholar]
- 34.Campbell TS, Labelle LE, Bacon SL, Faris P, Carlson LE. Impact of mindfulness-based stress reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: A waitlist-controlled study. Journal of Behavioral Medicine. 2012;35:262–271. doi: 10.1007/s10865-011-9357-1. [DOI] [PubMed] [Google Scholar]
- 35.Deyo M, Wilson KA, Ong J, Koopman C. Mindfulness and rumination: does mindfulness training lead to reductions in ruminative thinking associated with depression? Explore. 2009;5:265–271. doi: 10.1016/j.explore.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 36.Watkins ER. Constructive and unconstructive repetitive thought. Psychological Bulletin. 2008;134:163–206. doi: 10.1037/0033-2909.134.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feldman GC, Hayes AM, Kumar SM, Greeson JG, Laurenceau JP. Mindfulness and emotion regulation: the development and initial validation of the cognitive and affective mindfulness scale-revised (CAMS-R) Journal of Psychopathology and Behavioral Assessment. 2007;29:177, e190. [Google Scholar]
- 38.Delgado LC, Guerra P, Perakakis P, Vear MN, del Paso GR, Vila J. Treating chronic worry: psychological and physiological effects of a training programme based on mindfulness. Behaviour Research & Therapy. 2010;48:873–882. doi: 10.1016/j.brat.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 39.Robins CJ, Keng SL, Ekblad AG, Brantley JG. Effects of mindfulness-based stress reduction on emotional experience and expression: A randomized controlled trial. Journal of Clinical Psychology. 2011;68:117–131. doi: 10.1002/jclp.20857. [DOI] [PubMed] [Google Scholar]
- 40.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: 2000. Text Revision Ed. [Google Scholar]
- 41.Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 42.Gross JJ. Emotion regulation: Affective, cognitive and social consequences. Psychophysiology. 2002;39:281–291. doi: 10.1017/s0048577201393198. [DOI] [PubMed] [Google Scholar]
- 43.Hayes SC, Wilson KW, Gifford EV, Follette VM, Strosahl K. Emotional avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64:1152–1168. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- 44.Tull MT, Roemer L. Emotion regulation difficulties associated with the experience of uncued panic attacks: Evidence of experiential avoidance, emotional nonacceptance, and decreased emotional clarity. Behavior Therapy. 2007;38:378–391. doi: 10.1016/j.beth.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 45.Salters-Pedneault K, Roemer S, Tull MT, Rucker L, Mennin DS. Evidence of broad deficits in emotion regulation associated with chronic worry and generalized anxiety disorder. Cognitive Therapy and Research. 2006;30:469–480. [Google Scholar]
- 46.Mennin DS, McLaughlin KA, Flanagan TJ. Emotion regulation deficits in generalized anxiety disorder, social anxiety disorder, and their co-occurrence. Journal of Anxiety Disorders. 2009;23:866–871. doi: 10.1016/j.janxdis.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aldao A, Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research & Therapy. 2010;48:974–983. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 48.McLaughlin KA, Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy. 2011;49:186–193. doi: 10.1016/j.brat.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV TR Axis I Disorders, Research Version, Patient Edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 50.Di Nardo PA, O’Brien GT, Barlow DH, Waddell MT, Blanchard EB. Reliability of DSM-III anxiety disorder categories using a new structured interview. Archives of General Psychiatry. 1983;40:1070–1075. doi: 10.1001/archpsyc.1983.01790090032005. [DOI] [PubMed] [Google Scholar]
- 51.Watson D, Clark LA. Self-versus peer ratings of specific emotional traits: evidence of convergent and discriminant validity. Journal of Personality and Social Psychology. 1991;60:927–940. [Google Scholar]
- 52.Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: 1. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- 53.Meyer TJ, Miller M, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 54.Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27:248–259. [Google Scholar]
- 55.Nolan SA, Roberts JE, Gotlib IH. Neuroticism and ruminative response style as predictors of change in depressive symptomatology. Cognitive Therapy and Research. 1998;22:445–455. [Google Scholar]
- 56.Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after natural disaster: The 1989 Loma Preita earthquake. Journal of Personality and Social Psychology. 1991;61:115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- 57.Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Psychopathology and Behavioral Assessment. 2003;26:41–54. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- 58.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behaviour Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 59.Watkins E. Depressive rumination: Investigating mechanisms to improve cognitive behavioural treatments. Cognitive Behaviour Therapy. 2009:1. doi: 10.1080/16506070902980695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Roelofs J, Huibers M, Peeters F, Arntz A, van Os J. Rumination and worrying as possible mediators in the relation between neuroticism and symptoms of depression and anxiety in clinically depressed individuals. Behaviour Research and Therapy. 2008;46:1283–1289. doi: 10.1016/j.brat.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 61.Segerstrom SC, Tsao JCI, Alden LE, Craske MG. Worry and rumination: Repetitive thought as a concomitant and predictor of negative mood. Cognitive Therapy and Research. 2000;25:671–688. [Google Scholar]
- 62.Watkins E, Moulds M, Mackintosh B. Comparison between rumination and worry in a non-clinical population. Behaviour Research and Therapy. 2005;43:1577–1585. doi: 10.1016/j.brat.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 63.Borkovec TD, Alcaine OM, Behar E. Avoidance theory of worry and generalized anxiety disorder. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorders: Advances in research and practice. New York: Guilford Press; 2004. pp. 77–108. [Google Scholar]
- 64.Borkovec TD, Robinson E, Pruzinsky T, DePree JA. Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy. 1983;21:9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- 65.Mennin DS, Heimberg RG, Turk CL, Fresco DM. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behaviour Research and Therapy. 2005;42:1281–1310. doi: 10.1016/j.brat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 66.Modinos G, Ormel J, Aleman A. Individual differences in dispositional mindfulness and brain activity involved in reappraisal of emotion. Social cognitive and affective neuroscience. 2010;5:369–377. doi: 10.1093/scan/nsq006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Desrosiers A, Donalds R, Anderson M, Itzoe M, Britton W. School based mindfulness training may offer clinical benefits. Boston, MA: World Congress of Behavioral and Cognitive Therapy; 2010. [Google Scholar]
- 68.Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Waltz T, Zettle RD. Preliminary psychometric properties of the acceptance and action questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy. 2011;42:676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]