Abstract
Background:
Smoke-free air laws have effectively reduced cigarette consumption at the population level; however, the influence of these policies on smoking among those with mental illness is unclear. We examined whether associations between statewide restaurant/bar smoking bans and cigarette smoking varied by psychiatric diagnoses and gender.
Methods:
We analyzed data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC, Wave 1: 2001–2002; Wave 2: 2004–2005; n = 7,317 smokers). All analyses were stratified by gender. We examined whether tobacco cessation was associated with the interaction between ban implementation and Wave 1 psychiatric diagnoses (alcohol use disorder [AUD], anxiety disorder [AD], or mood disorder), adjusting for relevant covariates. Among those who continued to use tobacco at Wave 2, we examined associations between Wave 2 cigarettes per day (CPD) and the diagnoses × ban interactions, controlling for Wave 1 CPD and other relevant covariates.
Results:
Among men with an AUD and women with an AD, ban implementation was associated with 6% and 10% greater probability of tobacco cessation at Wave 2, respectively. Among men in the overall sample, ban implementation was associated with smoking 0.8 fewer CPD at Wave 2. Associations with CPD were nonsignificant among women. Interactions between ban implementation and psychiatric diagnoses were also nonsignificant when examining CPD, suggesting consistent reductions in CPD among men but not among women.
Conclusions:
This study provided the first evidence that statewide restaurant/bar smoking bans may be associated with reduced smoking among those with select psychiatric conditions.
INTRODUCTION
A growing body of research has documented large disparities in cigarette smoking and nicotine dependence based on mental health status. Those with mental illness are more likely to smoke, smoke more heavily, are more dependent on nicotine, have more severe withdrawal, and have more difficulty quitting than those without mental illness (Center for Behavioral Health Statistics and Quality, 2013; Centers for Disease Control and Prevention, 2013; Grant, Hasin, Chou, Stinson, & Dawson, 2004; Lasser et al., 2000; Lawrence, Mitrou, & Zubrick, 2009; Smith, Homish, Giovino, & Kozlowski, 2014; Weinberger, Desai, & McKee, 2010). A recent report from the Substance Abuse and Mental Health Services Administration found that the prevalence of smoking in the United States declined from 1997 to 2011 among those without, but not with, mental illness (Center for Behavioral Health Statistics and Quality, 2013). Further, persons with serious mental illness are at increased risk for tobacco-related illnesses and die, on average, 25 years prematurely (Colton & Manderscheid, 2006). This issue is particularly relevant from a tobacco control perspective, given evidence that one third to one half of cigarette smokers have a comorbid diagnosis (Grant, Hasin, et al., 2004; Lasser et al., 2000). It has been speculated that continued reductions in smoking in the general U.S. population will require stronger tobacco control efforts that reach smokers with mental illness (Williams & Ziedonis, 2004; Ziedonis et al., 2008).
Tobacco control policies, such as smoke-free air laws, have been demonstrated to effectively reduce smoking rates in the general population (see Cummings, Fong, & Borland, 2009, for a review). To date, 28 states have implemented statewide smoke-free air laws in restaurants and bars (American NonSmokers’ Rights Foundation, 2013b). Not only do these policies reduce second-hand exposure to smoke (Akhtar, Currie, Currie, & Haw, 2007; Travers et al., 2004), they are also associated with reductions in cigarette consumption (Tauras, 2006; Wasserman, Manning, Newhouse, & Winkler, 1991) and greater likelihood of making quit attempts (Hackshaw, McEwen, West, & Bauld, 2010).
Despite this evidence for the effectiveness of smoke-free air laws among the general population, there has been virtually no research on whether smoking bans are associated with reduced smoking among subgroups of individuals with mental illness (Ziedonis et al., 2008). Given that smokers with mental illness have more difficulty quitting, as well as evidence that prevalence of smoking has not been reduced among those with mental illness, one might suspect that smoke-free air policies have less of an impact on cigarette consumption among this vulnerable population (Williams & Ziedonis, 2004). However, this may not be the case across all psychiatric diagnoses. Young-Wolff et al. (2013) found that smoking bans in restaurants and bars were associated with remission of alcohol use disorders (AUD), particularly among smokers and among men. Given strong links between smoking and alcohol use, particularly among men (Westmaas & Langsam, 2005), one might anticipate reductions in smoking to accompany reductions in AUD.
The aim of the current investigation was to examine whether the implementation of smoking bans in restaurants and bars would be differentially associated with tobacco cessation and reductions in cigarette smoking by psychiatric diagnoses and gender. To achieve this aim, we analyzed nationally representative data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Wave 1: 2001–2002, Wave 2: 2004–2005). Between the two waves of data collection, eight states implemented statewide smoking bans in bars and restaurants. We examined whether smokers who lived in states that implemented bans were more likely to stop using tobacco than those who lived in states with no bans, and whether associations varied by mental illness. Among Wave 1 smokers who reported continued tobacco use at Wave 2, we examined whether those who lived in states that implemented smoking bans had greater reductions in cigarettes per day than those in states without bans, and again whether this varied by mental illness. Our analyses were conducted separately for AUD, mood disorders (MD), and anxiety disorders (AD) and were stratified by gender. These specific disorders were chosen for multiple reasons. For one, these disorders were prevalent enough to have adequately powered analyses. Second, these disorders cover both the internalizing and externalizing spectrum of disorders (Krueger, 1999; Krueger, Caspi, Moffitt, & Silva, 1998; Krueger et al., 2002). Third, as noted, AUD may be particularly relevant when examining the influence of bans at bars and restaurants.
We hypothesized that the implementation of smoking bans would be less strongly associated with reductions in smoking among those with mental illness than those without. Smokers with mental illness are more dependent on nicotine and have more difficulty quitting and thus may be less influenced by policy-level tobacco control efforts. However, we also anticipated greater reductions in smoking among those with AUD than other diagnoses and expected that this association would be stronger among men than women with AUD, following the findings from Young-Wolff et al. (2013).
METHODS
Participants
A detailed account of the NESARC methodology can be found elsewhere (Grant & Kaplan, 2005; Grant, Kaplan, Shepard, & Moore, 2003; Grant, Stinson, et al., 2004; Grant et al., 2009). Briefly, the Wave 1 NESARC data were collected during 2001 and 2002 and Wave 2 during 2004 and 2005. The response rate for Wave 1 was 81%, and the sample of 43,093 represented the civilian, noninstitutionalized adult population in the United States. Wave 2 included 34,653 (80%) of the original respondents. For both waves, surveys were administered face to face, using computer-assisted personal interviews. African Americans, Hispanics, and young adults were oversampled, and the data were weighted to adjust for nonresponse at the household and person levels. Based on the 2000 Census, the data were adjusted on sociodemographic variables to ensure an accurate representation of the U.S. population. For the current study, we selected the 7,317 smokers at Wave 1 (>100 cigarettes in their lifetime and smoked during the past year), who completed both waves of data collection, and resided in states that did not have comprehensive statewide smoking bans in restaurants and bars at Wave 1.
Measures
Mental Illness
Axis I and Axis II mental illness diagnoses were measured at Wave 1 using the Alcohol Use Disorder and Associated Disabilities Interview Schedule, DSM-IV version (AUDADIS-IV) (Grant & Dawson, 2000; Grant, Dawson, et al., 2003). Our study included past-year diagnoses for MD, AD, and AUD. MD included major depression, dysthymia, mania, and hypomania. AD included generalized anxiety disorder, panic disorder, social phobia, specific phobia, and agoraphobia. AUD included alcohol abuse and dependence.
Tobacco Cessation and Cigarettes per Day
We defined cessation as long-term (at least 1 year) abstinence from all forms of tobacco (North American Quitline Consortium, 2009). Using this definition, we identified quitters as those who were smokers at Wave 1 and who did not use tobacco during the past year at Wave 2. Cigarettes per day were assessed at both Wave 1 and Wave 2 with the following prompt: “In the days that you smoked in the past year, about how many cigarettes did you usually smoke?”
Smoking Bans in Restaurants and Bars
Eight states were identified as having implemented smoking bans in restaurants and bars between the Wave 1 and Wave 2 NESARC data collection. These states were Delaware, New York, Connecticut, Maine, Massachusetts, Rhode Island, Vermont, and Washington (American NonSmokers’ Rights Foundation, 2012). California implemented comprehensive smoke-free policies in restaurants and bars prior to Wave 1, and the 589 smokers from California were excluded. Residence data were only available at the state level and not at the municipality level; thus, we were unable to examine residence in substate geographical locations that had implemented bans. However, only 19 municipalities (approximately 1% of the population) located in states without statewide bans implemented smoke-free policy in restaurants, bars, and workplaces between 2001 and 2004 (American NonSmokers’ Rights Foundation, 2013a).
Covariates
We included several covariates in our models that could potentially influence differences in cessation and cigarettes per day between those residing in states that implemented bans, those with and without mental illness, and by gender. Wave 1 covariates included nicotine dependence levels, cigarettes per day, smokeless tobacco use, household income, education, age, race/ethnicity, state-level cigarette excise tax rates (2002), and frequency of drinking in public. Wave 2 covariates included whether states had implemented work-site smoking bans during the NESARC data collection, smokeless tobacco use, and cigarette tax increases (2002–2004). When examining Wave 2 cigarettes per day as our outcome, we also included Wave 2 use of smokeless tobacco products when selecting for male smokers. There were insufficient numbers of females using smokeless tobacco to include as a covariate when selecting for women who smoked.
Our measure of nicotine dependence was based on a count of DSM-IV nicotine dependence symptoms. Past-year household income was divided into 21 categories, ranging from “Less than $5,000” to “$200,000 or more,” and was entered as a continuous variable using the category numbers. Education was measured as highest grade or year of school completed, ranging from 1 = no formal schooling to 14 = Completed graduate or professional degree (master’s degree or higher). This was also entered as a continuous variable. Race/ethnicity categories were as follows: (a) White/Caucasian, not Hispanic or Latino; (b) Black/African American, not Hispanic or Latino; (c) American Indian/Alaska Native, not Hispanic or Latino; (d) Asian/Native Hawaiian/Pacific Islander, Not Hispanic or Latino; (e) Hispanic or Latino. There were 6 states that implemented smoke-free work legislation, 4 of which also implemented restaurant/bar bans (Delaware, New York, and Massachusetts) (American NonSmokers’ Rights Foundation, 2012). To control for cigarette taxation, we included state-level excise tax information from 2002, as well as a variable for change in state-level excise taxes between 2002 and 2004 (Campaign for Tobacco-Free Kids, 2013; Federation of Tax Administrators, 2013). We also included a variable for frequency of drinking in public at Wave 1, which was measured from 0 to 10 (never to every day). This variable was important to include as a covariate, in order to account for associations with all three variables of interest (state ban implementation, psychiatric diagnosis, and smoking outcomes; Young-Wolff et al., 2013). Finally, our variable for smokeless tobacco was based on any use of snuff or chewing tobacco during the past year.
Analyses
All analyses were conducted using Stata Statistical Software, Release 13.0 (StataCorp, 2013) and accounted for the NESARC survey design. We first examined bivariate associations between ban-state residence and the following variables: Wave 1 and Wave 2 cigarettes per day, Wave 1 nicotine dependence, Wave 1 and Wave 2 smokeless tobacco use, tobacco cessation rates, and Wave 1 frequency of drinking in public. All of these bivariate associations were examined by gender and psychiatric diagnoses. We calculated significance using chi-square tests of independence and t tests.
We stratified all models by gender. In our first series of multivariable models, we used logistic regression to examine odds of tobacco cessation by interactions between residence in states that implemented bans and the following psychiatric diagnosis categories, each in a separate model: (a) AUD, (b) MD, and (c) AD. We first examined a main effects–only model and then tested the interaction between ban, gender, and psychiatric diagnosis. For all models, our mental illness comparison group was composed of those with no lifetime history of mental illness. For example, when examining the interaction between smoking ban and alcohol use disorder, we only included those who had either a past year AUD or no history of mental illness. This comparison group was selected so that our analyses compared those with mental illness to those without, rather than those with one mental illness to those who potentially had other mental illnesses. Significant interactions were further examined using simple slopes analyses. We followed the same general procedure when examining cigarettes per day at follow-up as the outcome, first examining a main effects–only model and then testing interactions between ban implementation and mental illness diagnoses. We used linear regression rather than logistic regression for this outcome.
RESULTS
Bivariate Associations
Among male smokers, 41.7% had a past-year psychiatric diagnosis at Wave 1. The prevalence of AUD was 21.7%, of AD was 10.7%, and of MD was 12.2%. Table 1 displays comparisons between those residing in states that implemented restaurant/bar smoking bans and those residing in states without statewide restaurant/bar smoke-free policy. Comparisons were made for tobacco use outcomes and frequency of drinking in public and were categorized by gender and psychiatric diagnosis. Those residing in states that implemented bans generally smoked fewer cigarettes per day at Wave 1 and Wave 2 and had fewer nicotine dependence symptoms, regardless of psychiatric diagnosis. Differences in quit rates were only found for men with no diagnosis or men with an AUD. Those residing in states with bans were more likely to stop using tobacco in both of these groups. Men living in states that implemented bans reported more frequent public drinking at Wave 1, if they had no diagnosis, any mental illness, or an AUD.
Table 1.
Bivariate Associations Between Ban-State, Cigarette Outcomes, and Frequency of Drinking in Public Among Cigarette Smokers (n = 9,913), by Gender and Mental Illness
| No mental illness (n = 5,935) | Alcohol use disorder (n = 1,630) | Mood disorder (n = 1,654) | Anxiety disorder (n = 1,576) | |||||
|---|---|---|---|---|---|---|---|---|
| No ban | Ban | No ban | Ban | No ban | Ban | No ban | Ban | |
| Men | ||||||||
| Frequency (among all male smokers) | 51.7 | 6.6 | 19.3 | 3.4 | 11.1 | 1.5 | 1.4 | 10.1 |
| W1 CPD | 16.4 (10.8) | 14.0*** (9.8) | 16.5 (11.4) | 14.4*** (11.6) | 17.7 (11.8) | 17.0 (13.3) | 19.8 (11.7) | 18.3** (12.2) |
| W2 CPD | 18.8 (10.9) | 16.5*** (10.3) | 17.9 (11.2) | 14.9*** (8.9) | 19.2 (11.8) | 17.2** (11.3) | 20.5 (12.3) | 17.4*** (9.8) |
| W1 nicotine dependencea | 3.1 (2.6) | 3.2 (2.7) | 5.0 (3.3) | 4.2*** (2.9) | 5.8 (3.3) | 6.4*** (3.9) | 5.6 (3.2) | 5.1** (3.4) |
| W1 smokeless tobacco use | 7.4 | 1.4*** | 17.7 | 15.5 | 13.6 | 5.1*** | 11.0 | 13.1 |
| W2 smokeless tobacco use | 5.0 | 0.4*** | 13.5 | 9.3 | 7.2 | 3.1 | 6.7 | 11.7 |
| Percent quit by W2b | 20.4 | 22.3* | 15.2 | 25.2*** | 14.8 | 13.5 | 10.5 | 11.3 |
| W1 frequency of drinking in publicc | 1.6 (2.2) | 2.1*** (2.6) | 3.8 (2.8) | 4.3** (2.4) | 2.2 (2.5) | 2.2 (2.6) | 2.2 (2.5) | 2.1 (2.8) |
| Women | ||||||||
| Frequency (among all female smokers) | 49.7 | 8.3 | 10.6 | 1.4 | 18.6 | 2.8 | 19.3 | 3.0 |
| W1 CPD | 14.1 (9.2) | 13.2*** (10.5) | 13.3 (9.3) | 10.8*** (8.0) | 16.1 (10.9) | 15.1 (13.5) | 16.7 (10.7) | 15.5* (11.6) |
| W2 CPD | 15.0 (9.2) | 14.1** (9.1) | 13.6 (8.7) | 12.3*** (9.7) | 16.3 (10.6) | 14.8 (10.5) | 17.3 (10.1) | 15.1** (11.6) |
| W1 nicotine dependencea | 3.4 (2.7) | 3.1*** (2.7) | 5.2 (3.2) | 5.3 (3.2) | 5.7 (3.3) | 5.9* (3.1) | 5.6 (3.1) | 5.6 (2.9) |
| W1 smokeless tobacco use | — | — | — | — | — | — | — | — |
| W2 smokeless tobacco use | — | — | — | — | — | — | — | — |
| Percent quit by W2b | 21.3 | 21.7 | 18.1 | 17.3 | 16.4 | 18.3 | 17.8 | 26.0*** |
| W1 frequency of drinking in publicc | 1.43 (2.01) | 1.53* (2.01) | 3.7 (2.6) | 4.1*** (2.4) | 1.7 (2.2) | 2.2*** (2.8) | 1.7 (2.2) | 1.9 (2.3)* |
Note. Figures are mean (SD) or percentages. Estimates accounted for the NESARC survey design. Significance calculated using chi-square tests of independence and t tests.
aCount of DSM-IV nicotine dependence symptoms, range = 0–14.
bQuitting defined as past-year abstinence from all forms of tobacco.
cRange = 0–10 (never to every day).
*p < .05, **p < .01, ***p < .001 (ban versus no ban).
Among female smokers, 42% had a past-year psychiatric diagnosis. The prevalence of AUD among female smokers in this population was 11.4%. The prevalence of AD and MD were 20.8% and 21.0%, respectively. With the exception of women with MD, those residing in states that implemented bans smoked fewer cigarettes per day at both Waves of data collection. Among women with no psychiatric diagnosis, those living in states that implemented bans had fewer nicotine dependence symptoms, whereas women with a MD reported a greater number of symptoms. Ban implementation was associated with greater likelihood of quitting only among women with an AD. Similar to men, women who lived in states that implemented bans tended to drink in public more frequently at Wave 1; however, women with no mental illness or an AUD living in states that implemented bans reduced their frequency of drinking in public by follow-up, relative to women residing in states with no bans.
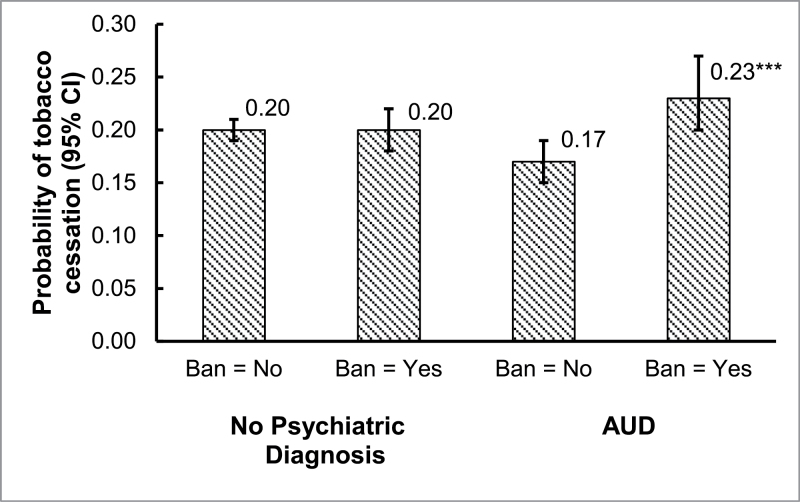
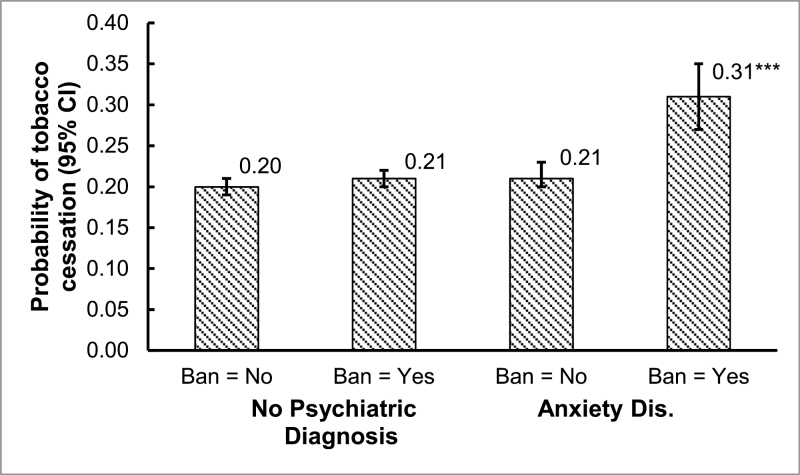
Tobacco Cessation
We first examined whether residence in a state that implemented bans (referred to as “ban” throughout the rest of the results) was associated with tobacco cessation, stratified by gender (Table 2). In these main effects–only models, the associations between ban and cessation were nonsignificant among both men and women (p > .05). We then examined interactions between ban and each of the three mental illness diagnosis variables. The interaction between AUD and ban was significant among men (p < .05; Figure 1), and the interaction between AD and ban was significant among women (p < .05; Figure 2). Simple slope analyses revealed that among men with an AUD, ban was associated with 1.55 times greater odds of tobacco cessation (95% CI = 1.18, 2.05). The association was nonsignificant among men with no mental illness. Among women with an AD, ban was associated with 1.73 times greater odds of tobacco cessation, whereas the association among women with no mental illness was nonsignificant.
Table 2.
Adjusted Associations Between Residence in States That Implemented Bans and Tobacco Cessation/Cigarettes per Day at Follow-up
| Model 1: Tobacco cessation, OR (95% CI) | Model 2: Wave 2 cigarettes per day, β (95% CI) | |||
|---|---|---|---|---|
| Women | Men | Women | Men | |
| Ban | 1.08 (0.94, 1.22) | 0.98 (0.85, 1.12) | −0.52 (−1.16, 0.12) | −0.82 (−1.45, −0.19)* |
| Alcohol use disordera | 0.78 (0.68, 0.90)** | 0.88 (0.77, 0.99)* | −0.58 (−1.03, −0.12)* | −1.15 (−1.80, −0.51)** |
| Anxiety disordera | 1.34 (1.18, 1.53)*** | 0.66 (0.52, 0.83)** | 0.60 (0.10, 1.10)* | −0.13 (−1.00, 0.74) |
| Mood disordera | 0.91 (0.76, 1.08) | 1.00 (0.76, 1.32) | −0.47 (−0.88, −0.06)* | −1.27 (−2.18, −0.35)** |
| Nicotine dependence (W1) | 0.88 (0.86, 0.90)*** | 0.90 (0.87, 0.93)*** | 0.35 (0.29, 0.42)*** | 0.46 (0.36, 0.56)*** |
| Cigarettes per day (W1) | 0.95 (0.94, 0.96)*** | 0.95 (0.93, 0.96)*** | 0.49 (0.46, 0.52)*** | 0.55 (0.42, 0.59)*** |
| Smokeless tobacco use (W1)b | — | 0.83 (0.65, 1.08) | — | — |
| Smokeless tobacco use (W2)b | — | — | — | −5.28 (−6.21, −4.35)*** |
| State cigarette excise tax (W1; 2002) | 0.98 (0.87, 1.10) | 1.10 (0.97, 1.24) | −0.37 (−0.83, 0.09) | −0.87 (−1.53, −0.21)* |
| Increases in state cigarette excise tax (W1–W2; 2002–2004) | 0.97 (0.85, 1.11) | 0.89 (0.72, 1.09) | 0.74 (−0.13, 1.62) | 0.35 (−0.39, 1.09) |
| Frequency of drinking in public (W1) | 1.04 (1.01, 1.06)** | 1.03 (1.00, 1.06)* | −0.20 (−0.29, −0.12)*** | −0.17 (−0.29, −0.06)** |
| Implementation of statewide work-site smoking ban | 0.86 (0.74, 1.00)* | 0.88 (0.78, 0.99)* | 0.35 (−0.18, 0.89) | 1.26 (0.63, 1.89)*** |
| Race/ethnicity | ||||
| White/Caucasian, non-Hispanic | Ref. | Ref. | Ref. | Ref. |
| Black/African American, non-Hispanic | 0.89 (0.78, 1.02) | 0.85 (0.73, 1.00)* | −2.67 (−3.01, −2.33)*** | −3.00 (−3.59, −2.41)*** |
| Other, non-Hispanic | 0.72 (1.52, 1.94)*** | 1.46 (1.21, 1.76)*** | −3.00 (−3.51, −2.49)*** | −3.67 (−4.25, −3.08)*** |
| Hispanic | 0.71 (0.55, 0.90)** | 1.54 (1.31, 1.82)*** | −2.34 (−3.30, −1.37)*** | −2.32 (−3.32, −1.32)*** |
| Income | 1.01 (0.96, 1.06) | 1.04 (0.97, 1.11) | 0.01 (−0.18, 0.20) | 0.04 (−0.16, 0.24) |
| Education | 1.11 (1.04, 1.17)** | 1.10 (1.03, 1.19)** | −0.54 (−0.72, −0.35)*** | −0.67 (−0.94, −0.39)*** |
| Age | 1.00 (0.99, 1.00) | 1.00 (1.00, 1.01) | 0.04 (0.02, 0.05)*** | 0.01 (−0.01, 0.03) |
Note. OR = odds ratio; CI = confidence interval. All estimates accounted for the Survey Design. Model 1 estimates were calculated using logistic regression; Model 2 estimates were calculated using linear regression.
aThe reference category for each psychiatric diagnosis was smokers with no lifetime diagnosis.
bSmokeless tobacco use was not included as a covariate when selecting for women due to insufficient numbers of users.
*p < .05, **p < .01, ***p < .001.
Figure 1.
Among men: tobacco cessation associated with the interaction between alcohol use disorder and residence in a state that implemented restaurant/bar smoking bans. All estimates accounted for the survey design. Estimates were calculated using logistic regression. The following covariates were included in the model: Wave 1 cigarettes per day, Wave 1 nicotine dependence, Wave 1 smokeless tobacco use, 2002 state cigarette excise taxes, change in excise taxes 2002–2004, Wave 1 frequency of drinking in public, annual household income, highest level of education attained, race/ethnicity, age, and whether respondents lived in a state that had implemented a work-site smoking ban during the NESARC study.
***p < .001 for difference between ban = no vs. yes.
Figure 2.
Among women: tobacco cessation associated with the interaction between anxiety disorder and residence in a state that implemented restaurant/bar smoking bans. All estimates accounted for the survey design. Estimates were calculated using logistic regression. The following covariates were included in the model: Wave 1 cigarettes per day, Wave 1 nicotine dependence, Wave 1 non-cigarette tobacco use, 2002 state cigarette excise taxes, change in excise taxes 2002–2004, Wave 1 frequency of drinking in public, annual household income, highest level of education attained, race/ethnicity, age, and whether respondents lived in a state that had implemented a work-site smoking ban during the NESARC study.
***p < .001 for difference between ban = no versus yes.
Cigarettes per Day
We first examined the main effect association between ban and Wave 2 cigarettes per day, stratified by gender. In this model, we selected for Wave 1 smokers who continued to use tobacco at Wave 2 and adjusted for Wave 1 cigarettes per day, Wave 2 smokeless tobacco use, and other relevant covariates. Among men, ban was associated with 0.82 fewer cigarettes per day (95% CI = −1.45, −0.19). The association was nonsignificant among women. None of the interactions between ban and mental illness diagnoses were significant for men nor for women.
DISCUSSION
This study extended previous research by examining whether residence in states that implemented restaurant/bar smoking bans was associated with greater probability of tobacco cessation and reductions in cigarette consumption, and whether these associations varied by mental illness diagnoses. Contrary to our hypotheses, we did not find differential reductions in cigarette consumption (i.e., cigarettes per day) between those with and without psychiatric diagnoses. Ban implementation was associated with fewer cigarettes per day among men, regardless of mental illness diagnoses. Potential interpretations of this finding are discussed below. In support of our hypotheses, we found evidence that the implementation of statewide smoking bans in bars and restaurants was associated with greater probability of tobacco cessation among men with AUD than those with no history of psychiatric illness. We also found this association for women with AD.
Our findings for the overall sample were consistent with previous research. For example, Tauras (2006) found that smoke-free air laws were associated with reduced average smoking by adult smokers but were not associated with reduced prevalence of smoking. However, the current study’s results suggest these findings may not apply broadly to all smokers. For one, we only found significant associations with fewer cigarettes per day among men although the average effect was small (<1 cigarette). We also found significant associations between ban implementation and tobacco cessation among men with AUD: those living in states that implemented bans were approximately 6% more likely to stop using tobacco than those residing in states without bans. Our explanation for this finding revolves around social contexts for smoking and barriers to cessation. Alcohol consumption has previously been shown to be strongly related to increased risk of smoking relapse among quitters who are heavy drinkers (Kahler, Spillane, & Metrik, 2010; McKee, Krishnan-Sarin, Shi, Mase, & O’Malley, 2006), and this may be particularly true for men (Westmaas & Langsam, 2005). Further, heavier, more problematic drinkers are substantially more likely to drink in bars than those who consume less alcohol and drink less problematically (Single & Wortley, 1993), and smoking often accompanies this drinking. Thus, drinking in bars may present a particularly strong barrier to smoking cessation for men with AUD. Smoke-free air laws may help remove this barrier by dramatically increasing the inconvenience of smoking cigarettes in bars and restaurants.
It is also important to mention that previous findings suggest AUD remittance was more likely among male smokers residing in states that implemented restaurant/bar smoking bans (Young-Wolff et al., 2013). Further, Young-Wolff et al. (2013) and McKee et al. (2009) found greater reductions in public drinking following the implementation of the bans, among heavier drinkers or men with AUD. These reductions in drinking may mediate the pathway to reduced smoking, as tobacco and alcohol use tend to operate as complements. However, we found significant associations after adjusting for frequency of drinking in public, suggesting a possible synergistic interaction between reductions in drinking and tobacco cessation. It is important to note that female smokers with AUD did not reduce their frequency of drinking in public, perhaps partially explaining the gender difference in this finding. Future research exploring these speculated mechanisms will help elucidate the influence of smoking bans on both drinking and smoking among those with AUD and drinkers in general.
Among women with AD, we found that ban implementation was associated with approximately 10% greater probability of tobacco cessation. This finding may be driven by a paradigm that is similar to that for men with AUD. Negative affect and stress have been found to be a stronger barrier to smoking cessation for women than men (McKee, Maciejewski, Falba, & Mazure, 2003; Westmaas & Langsam, 2005). Westsmaas and Langsam (2005) specifically found that trait anxiety was a stronger predictor of failed quit attempts among women. Further, previous research has demonstrated that both smoking and alcohol use are common coping mechanisms for those with AUD, particularly those with social anxiety (Buckner, Eggleston, & Schmidt, 2006; Kushner, Sher, Wood, & Wood, 1994; Zvolensky et al., 2006). Restaurant/bar smoking bans may limit opportunities to utilize smoking as an anxiety-reducing mechanism in some social situations for women with AD, aiding in attempts to stop or reduce cigarette use.
We did not find differential effects for tobacco cessation among respondents with or without a MD. In contrast to individuals with AUD and AD, those with MD may be more socially isolated and less motivated to smoke in public settings, such as restaurants and bars. For example, Thornton et al. (2012) found that only 9% of those with depression reported social motives for smoking (Thornton et al., 2012). We also did not find significant interactions with psychiatric disorders when examining cigarette consumption, among those who continued to use tobacco. For men, this may have been the result of smokeless tobacco use. Rates of smokeless tobacco use at Wave 2 were substantially higher for men with an AUD or AD compared with men with no disorder. To explore this mechanism, we removed smokeless tobacco use as a covariate from these models and found that ban was associated with fewer cigarettes per day among both men with AUD and AD. This suggests that men with these disorders who continue to use tobacco may substitute smokeless tobacco for cigarettes. It is less clear why we did not find differential associations among women, particularly among those with AD. It may be the case that, because women with AD were more likely to stop using tobacco, those who continued to use tobacco were more dependent relative to women without disorders and thus less likely to reduce their cigarette consumption. We conducted post hoc exploratory analyses to examine this explanation and indeed found greater levels of nicotine dependence among women with AD who continued to smoke compared with women with AD who had quit and women without AD who continued to smoke.
Our interpretations of these findings are speculative, due to the lack of research on the impact of smoking bans among individuals with mental illness. Further, there are important limitations of this investigation to note. Smoking status was based on past-year tobacco use. This makes it possible that those defined as smokers at Wave 1 may have actually quit smoking within the year prior to the survey and were actually former smokers, and those defined as smoking at Wave 2 may also have quit within the year prior to the interview resulting in misclassications of continued smoking versus quitting. This misclassification could present bias if there were differential misclassification between states based on smoking ban implementation. It is impossible to test this bias or the direction of bias; however, the proportion of the sample to whom this applies is likely minimal. We were unable to assess the influence of relocation on study findings. However, if smoking bans did influence smoking, those who were identified as residing in states that implemented bans and moved to states without statewide bans would have been less likely to quit and thus biased results toward the null. Those who resided in states with no statewide bans may have resided in localities that did implement bans. This would also likely have biased results toward the null. However, between 2001 and 2004, only 19 municipalities in states without statewide bans implemented bans in bars, restaurants, and work-sites (approximately 1% of the population), suggesting this effect was minimal (American NonSmokers’ Rights Foundation, 2013a). We were unable to control for some potentially confounding variables. For example, states that implemented smoking bans may have had more widespread use of nicotine replacement therapy. Cigarette price can have a relatively strong influence on smoking behavior, and although we controlled for excise tax rates and increases, these are relatively crude measures of tobacco pricing.
There are also limitations to the generalizability of these findings. The NESARC sample was composed of adults, and we were thus unable to examine associations between smoking bans and tobacco use for adolescents and teens. The findings from this investigation may not extend to these age groups. Further, it will be important to investigate associations between smoking bans and tobacco use among younger samples with and without mental illness. The NESARC sample was also limited to noninstitutionalized adults, which is particularly relevant when considering the number of individuals with psychiatric illness who are institutionalized in mental health or correctional facilities. These individuals are likely exposed to restaurants and bars less frequently or not at all, and as a result, this study’s findings may not apply to these individuals. Studies of smoking bans in psychiatric residencies may be more applicable to this population (see Lawn & Pols, 2005, for a review). Lastly, we were unable to examine the influence of smoking bans on those with serious versus less serious mental illness. It may be the case that our findings were driven by those with less serious mental illness, and bans may not have as strong of an effect on those with more serious mental illness.
Our findings provide evidence that smoking-ban policies may be associated with reduced smoking among those with select psychiatric diagnoses. Currently, 30 states have statewide bans of smoking in restaurants and bars (American NonSmokers’ Rights Foundation, 2013b). Continued implementation of these policies may potentially reduce disparities in smoking for those with select mental disorders. Further, these findings support the need to continue investigating the influence of tobacco control policy on those with mental illness, particularly policies with direct implications for those with psychiatric disorders. For example, it is unclear whether increased tobacco taxes help individuals with psychiatric illness quit or reduce smoking. Further research is needed on smoking bans in psychiatric facilities because these policies have been demonstrated to reduce smoking among inpatients but have had limited success in achieving long-term abstinence (Lawn & Pols, 2005). The expansion of Medicaid to cover smoking cessation therapies may have allowed more of those with psychiatric diagnoses to access these treatments, but there has been limited research on the extent to which these services are being utilized. Continued research on these topics will be vital to reducing smoking among those with mental illness and assisting those who want to quit smoking to do so.
FUNDING
This research was funded by the National Institute on Drug Abuse (P50-DA033945-02, PI: S. McKee) and the National Institute of Mental Health (T32-MH014235-39, PI: H. Zhang).
DECLARATION OF INTERESTS
None declared.
REFERENCES
- Akhtar P. C., Currie D. B., Currie C. E., Haw S. J. (2007). Changes in child exposure to environmental tobacco smoke (CHETS) study after implementation of smoke-free legislation in Scotland: National cross sectional survey. British Medical Journal, 335, 545. 10.1136/bmj.39311.550197.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- American NonSmokers’ Rights Foundation. (2012). Percent of U.S. state populations covered by 100% smoke-free air law Retrieved July 23, 2013, from www.no-smoke.org/pdf/SummaryUSPopList.pdf
- American NonSmokers’ Rights Foundation. (2013a). Local 100% smokefree laws in all workplaces, restaurants, and bars: Effective by year Retrieved July 30, 2013, from www.no-smoke.org/pdf/current_smokefree_ordinances_by_year.pdf
- American NonSmokers’ Rights Foundation. (2013b). U.S. 100% smokefree laws in non-hospitality workplaces and restaurants and bars Retrieved August 7, 2013, from www.no-smoke.org/pdf/current_smokefree_ordinances_by_year.pdf
- Buckner J. D., Eggleston A. M., Schmidt N. B. (2006). Social anxiety and problematic alcohol consumption: The mediating role of drinking motives and situations. Behavior Therapy, 37, 381–391. 10.1016/j.beth.2006.02.007 [DOI] [PubMed] [Google Scholar]
- Campaign for Tobacco-Free Kids. (2013). Cigarette tax increases by state per year Retrieved July 30, 2013, from www.tobaccofreekids.org/research/factsheets/pdf/0275.pdf
- Center for Behavioral Health Statistics and Quality. (2013). Smoking rate among adults with serious psychological distress remains high. The CBHSQ Report. Substance Abuse and Mental Health Services Administration Retrieved from www.samhsa.gov/data/spotlight/spot120-smokingSPD.pdf
- Centers for Disease Control and Prevention. (2013). Vital signs: Current cigarette smoking among adults aged >= 18 years with mental illness: United States, 2009–2011. Morbidity and Mortality Weekly, 62, 81–87 Retrieved from www.cdc.gov/mmwr/ [PMC free article] [PubMed] [Google Scholar]
- Colton C. W., Manderscheid R. W. (2006). Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Preventing Chronic Disease, 3, A42 Retrieved from www.ncbi.nlm.nih.gov/pmc/articles/PMC1563985/ [PMC free article] [PubMed] [Google Scholar]
- Cummings K. M., Fong G. T., Borland R. (2009). Environmental influences on tobacco use: Evidence from societal and community influences on tobacco use and dependence. Annual Review of Clinical Psychology, 5, 433–458. 10.1146/annurev.clinpsy.032408.153607 [DOI] [PubMed] [Google Scholar]
- Federation of Tax Administrators. (2013). Cigarette tax increases 2000–2013 Retrieved July 30, 2013, from www.taxadmin.org/fta/rate/cig_inc02.html
- Grant B. F., Dawson D. A. (2000). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism [Google Scholar]
- Grant B. F., Dawson D. A., Stinson F. S., Chou P. S., Kay W., Pickering R. (2003). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence, 71, 7–16. 10.1016/s0376-8716(03)00070-x [DOI] [PubMed] [Google Scholar]
- Grant B. F., Goldstein R. B., Chou S. P., Huang B., Stinson F. S., Dawson D. A, … Compton W. M. (2009). Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry, 14, 1051–1066. 10.1038/mp.2008.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F., Hasin D. S., Chou S. P., Stinson F. S., Dawson D. A. (2004). Nicotine dependence and psychiatric disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry, 61, 1107–1115. 10.1001/archpsyc.61.11.1107 [DOI] [PubMed] [Google Scholar]
- Grant B. F., Kaplan K. (2005). Source and accuracy statement for wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism [Google Scholar]
- Grant B. F., Kaplan K., Shepard J., Moore T. (2003). Source and accuracy statement for wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism [Google Scholar]
- Grant B. F., Stinson F. S., Dawson D. A., Chou S. P., Dufour M. C., Compton W, … Kaplan K. (2004). Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 61, 807–816. 10.1001/archpsyc.61.8.807 [DOI] [PubMed] [Google Scholar]
- Hackshaw L., McEwen A., West R., Bauld L. (2010). Quit attempts in response to smoke-free legislation in England. Tobacco control, 19, 160–164. 10.1136/tc.2009.032656 [DOI] [PubMed] [Google Scholar]
- Kahler C. W., Spillane N. S., Metrik J. (2010). Alcohol use and initial smoking lapses among heavy drinkers in smoking cessation treatment. Nicotine & Tobacco Research, 12, 781–785. 10.1093/ntr/ntq083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger R. F. (1999). The structure of common mental disorders. Archives of General Psychiatry, 56, 921–926. 10.1001/archpsyc.56.10.921 [DOI] [PubMed] [Google Scholar]
- Krueger R. F., Caspi A., Moffitt T. E., Silva P. A. (1998). The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology, 107, 216–227. 10.1037/0021-843X.107.2.216 [DOI] [PubMed] [Google Scholar]
- Krueger R. F., Hicks B. M., Patrick C. J., Carlson S. R., Iacono W. G., McGue M. (2002). Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology, 111, 411–424. 10.1037/0021-843x.111.3.411 [PubMed] [Google Scholar]
- Kushner M. G., Sher K. J., Wood M. D., Wood P. K. (1994). Anxiety and drinking behavior: Moderating effects of tension-reduction alcohol outcome expectancies. Alcoholism: Clinical and Experimental Research, 18, 852–860. 10.1111/j.1530-0277.1994.tb00050.x [DOI] [PubMed] [Google Scholar]
- Lasser K., Boyd J. W., Woolhandler S., Himmelstein D. U., McCormick D., Bor D. H. (2000). Smoking and mental illness. The Journal of the American Medical Association, 284, 2606–2610. 10.1001/jama.284.20.2606 [DOI] [PubMed] [Google Scholar]
- Lawn S., Pols R. (2005). Smoking bans in psychiatric inpatient settings? A review of the research. Australian & New Zealand Journal of Psychiatry, 39, 866–885 Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=2009346098&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Lawrence D., Mitrou F., Zubrick S. R. (2009). Smoking and mental illness: Results from population surveys in Australia and the United States. BioMed Central Public Health, 9, 285. 10.1186/1471-2458-9-285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee S. A., Higbee C., O’Malley S., Hassan L., Borland R., Cummings K. M, … Hyland A. (2009). Longitudinal evaluation of smoke-free Scotland on pub and home drinking behavior: Findings from the International Tobacco Control Policy Evaluation Project. Nicotine & Tobacco Research, 11, 619–626. 10.1093/ntr/ntp020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee S. A., Krishnan-Sarin S., Shi J., Mase T., O’Malley S. S. (2006). Modeling the effect of alcohol on smoking lapse behavior. Psychopharmacology, 189, 201–210. 10.1007/s00213-006-0551-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee S. A., Maciejewski P. K., Falba T., Mazure C. M. (2003). Sex differences in the effects of stressful life events on changes in smoking status. Addiction (Abingdon, England), 98, 847–855. 10.1046/j.1360-0443.2003.00408.x [DOI] [PubMed] [Google Scholar]
- North American Quitline Consortium. (2009). Measuring quit rates. Quality improvement initiative. In An L., Betzner A., Luxenberg M. L., Rainey J., Capesius T., Subialka E. (Eds.). Phoenix, AZ: Author [Google Scholar]
- Single E., Wortley S. (1993). Drinking in various settings as it relates to demographic variables and level of consumption: Findings from a national survey in Canada. Journal of Studies on Alcohol and Drugs, 54, 590 Retrieved from www.jsad.com/jsad/article/Drinking_in_Various_Settings_As_It_Relates_to_Demographic_Variables_and_Lev/1949.html [DOI] [PubMed] [Google Scholar]
- Smith P. H., Homish G. G., Giovino G. A., Kozlowski L. T. (2014). Cigarette smoking and mental illness: A study of nicotine withdrawal. American Journal of Public Health, 104, e127–e133. 10.2105/AJPH.2013.301502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2013). Stata Statistical Software: Release 13.0. College Station, TX: StataCorp LP [Google Scholar]
- Tauras J. A. (2006). Smoke-free air laws, cigarette prices, and adult cigarette demand. Economic Inquiry, 44, 333–342. 10.1093/ei/cbj028 [Google Scholar]
- Thornton L. K., Baker A. L., Lewin T. J., Kay-Lambkin F. J., Kavanagh D., Richmond R, … Johnson M. P. (2012). Reasons for substance use among people with mental disorders. Addictive Behaviors, 37, 427–434. 10.1016/j.addbeh.2011.11.039 [DOI] [PubMed] [Google Scholar]
- Travers M. J., Cummings K. M., Hyland A., Repace J., Babb S., Pechacek T., Caraballo R. (2004). Indoor air quality in hospitality venues before and after implementation of a clean indoor air law-Western New York, 2003. Morbidity and Mortality Weekly Report, 53, 1038–1041 Retrieved from www.cdc.gov/mmwr/ [PubMed] [Google Scholar]
- Wasserman J., Manning W. G., Newhouse J. P., Winkler J. D. (1991). The effects of excise taxes and regulations on cigarette smoking. Journal of Health Economics, 10, 43–64. 10.1016/0167-6296(91)90016-G [DOI] [PubMed] [Google Scholar]
- Weinberger A. H., Desai R. A., McKee S. A. (2010). Nicotine withdrawal in US smokers with current mood, anxiety, alcohol use, and substance use disorders. Drug and Alcohol Dependence, 108, 7–12. 10.1016/j.drugalcdep.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westmaas J. L., Langsam K. (2005). Unaided smoking cessation and predictors of failure to quit in a community sample: Effects of gender. Addictive Behaviors, 30, 1405–1424. 10.1016/j.addbeh.2005.03.001 [DOI] [PubMed] [Google Scholar]
- Williams J. M., Ziedonis D. (2004). Addressing tobacco among individuals with a mental illness or an addiction. Addictive Behaviors, 29, 1067–1083. 10.1016/j.addbeh.2004.03.009 [DOI] [PubMed] [Google Scholar]
- Young-Wolff K. C., Hyland A., Desai R. A., Sindelar J., Pilver C. E., McKee S. A. (2013). Smoke-free policies in drinking venues predict transitions in alcohol use disorders in a longitudinal U.S. sample. Drug and Alcohol Dependence, 128, 214–221. 10.1016/j.drugalcdep.2012.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziedonis D., Hitsman B., Beckham J. C., Zvolensky M., Adler L. E., Audrain-McGovern J, … Riley W. T. (2008). Tobacco use and cessation in psychiatric disorders: National Institute of Mental Halth report. Nicotine & Tobacco Research, 10, 1691–1715. 10.1080/14622200802443569 [DOI] [PubMed] [Google Scholar]
- Zvolensky M. J., Bonn-Miller M. O., Feldner M. T., Leen-Feldner E., McLeish A. C., Gregor K. (2006). Anxiety sensitivity: Concurrent associations with negative affect smoking motives and abstinence self-confidence among young adult smokers. Addictive Behaviors, 31, 429–439. 10.1016/j.addbeh.2005.05.027 [DOI] [PubMed] [Google Scholar]