Abstract
Purpose
Asian Americans have consistently reported poorer communication with physicians compared with non-Hispanic Whites (NHW). This qualitative study sought to elucidate the similarities and differences in communication with physicians between Chinese and NHW breast cancer survivors.
Methods
Forty-four Chinese and 28 NHW women with early-stage breast cancer (stage 0-IIa) from the Greater Bay Area Cancer Registry participated in focus group discussions or individual interviews. We oversampled Chinese women because little is known about their cancer care experiences. In both interview formats, questions explored patients’ experiences and feelings when communicating with physicians about their diagnosis, treatment, and follow-up care.
Results
Physician empathy at the time of diagnosis was important to both ethnic groups; however, during treatment and follow-up care, physicians’ ability to treat cancer and alleviate physical symptoms was a higher priority. NHW and US-born Chinese survivors were more likely to assert their needs, whereas Chinese immigrants accepted physician advice even when it did not alleviate physical problems (e.g., pain). Patients viewed all physicians as the primary source for information about cancer care. Many Chinese immigrants sought additional information from primary care physicians and stressed optimal communication over language concordance.
Conclusions
Physician empathy and precise information were important for cancer patients. Cultural differences such as the Western emphasis on individual autonomy vs. Chinese emphasis on respect and hierarchy can be the basis for the varied approaches to physician communication we observed. Interventions based on cultural understanding can foster more effective communication between immigrant patients and physicians ultimately improving patient outcomes.
Keywords: Patient-Physician communication, Chinese Americans, Culture, Breast Cancer
INTRODUCTION
Effective patient-physician communication, where both parties share the same understanding of a conversation [1], is key to helping cancer patients cope with the physical and emotional challenges they face during diagnosis, treatment, and survivorship [2–5]. Kornblith (1998) delineated a vulnerability model of psychosocial adaption of cancer survivors, stressing that patients’ communication and relationships with physicians influence their management of late effects of treatment and psychosocial rehabilitation [6]. Patient-centered communication (i.e., communication during which the physician listens to patients, spends sufficient time answering questions, and provides relevant information) is valued as a mean to promote quality care and patient outcomes regardless of an individual’s background [7;8].
Minority patients are likely to experience poor communication with physicians as well as increased levels of stress during medical encounters [9–11]. For example, compared to Whites, Asian American women have reported less satisfaction during medical encounters due to perceptions that their doctors either did not listen to them or failed to demonstrate an understanding of their cultural backgrounds [9]. Recent research also indicated that Asian American cancer survivors had the poorest quality communication with their physicians [12;13]. This may, in part, be related to cultural differences in communication style.
Compared with Western Euro-Americans, Asian culture is known to be more collectivist, emphasizing harmonious relationships with others and conformity to authority over individual autonomy [14]. Since physicians represent the authority of medical knowledge, respect and deference to them is valued in Chinese culture [15;16]. Thus, Asian patients may have higher regard for their physicians’ recommendations than for their own preferences. This is distinct from the Western cultural value of individual patient rights and personal responsibility for one’s health; autonomy is encouraged and respected [17]. Such cultural differences may affect patient-physician communication processes and patient outcomes [18]. Chinese Americans consistently report poorer communication with their clinical providers compared with Whites [10;12;13]. Chinese American breast cancer survivors also report more unresolved physical problems compared to Non-Hispanic White (NHW) survivors [13;19]. In this paper, we report our qualitative investigation of similarities and differences between Chinese American and NHW patients’ perceptions and expectations of communication with physicians along the continuum of breast cancer care (i.e., diagnosis, treatment, and follow-up care). The significance of such a comparative research study is underscored by the fact that Chinese Americans are the largest Asian American subgroup and the fastest growing immigrant population [20].
METHODS
This analysis is part of a larger study that used qualitative and quantitative approaches to explore the impact of culture on breast cancer survivorship. This study was approved by the Institutional Review Boards at Georgetown University Medical Center, the California Health and Human Services Agency, and the Cancer Prevention Institution of California (CPIC) that operates the Greater Bay Area Cancer Registry (GBACR), the SEER registry for the San Francisco Bay Area.
Study Population and Setting
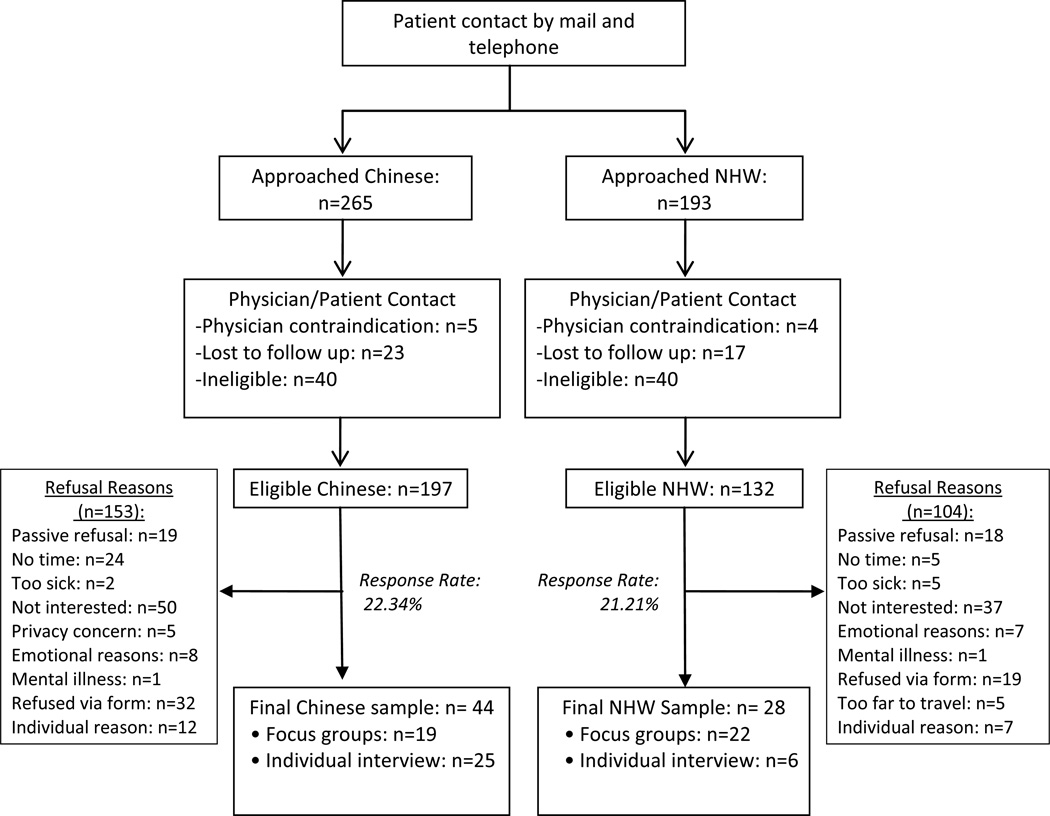
Chinese American (herein refers to US-born Chinese and foreign-born Chinese; the latter is also referred to as Chinese immigrants) and NHW women were recruited from the 2006–2008 GBACR. Eligible women were over 21 years old; had been diagnosed with stage 0-IIa breast cancer; had completed primary treatment (surgery, radiation, chemotherapy) within the past 1–5 years; and had no recurrence or other cancers. Breast cancer cases were randomly selected and invitation letters were mailed to women along with an opt-out form. Patients who did not return the opt-out form were called to solicit their interest and to screen for eligibility. Patients who had physician contraindications, who reported mental problems, or who were unable to clearly communicate with our field staff in Chinese or English were not invited to participate. Figure 1 describes our recruitment procedures and patients’ refusal reasons. A total of 44 Chinese American and 28 NHW women participated in this study. The sample size was estimated based on prior qualitative reports on breast cancer survivorship [21–23]. Actual study enrollment ended when we reached the data saturation point. We oversampled Chinese survivors because little is known about this group relative to NHWs.
Figure 1.
Flow Chart of Patient Enrollment
Qualitative Data Collection
In order to gather information on women’s survivorship experiences, semi-structured interview guides were developed and used for both focus group and individual telephone interviews--two common qualitative approaches in behavioral and social science [24;25]. Individual interviews were conducted to elicit narratives from women who felt uncomfortable sharing their experiences in a group setting. This methodology provided the research team with a more comprehensive understanding of survivorship experiences since focus groups tend to identify group norms while individual interviews explore the range of perceptions [26].
Theoretical framework
The entire interview guide was developed by adapting three theories: 1) Kornblith’s Vulnerability Model with an emphasize on patient-physician communication [6], 2) Transactional Model of Stress and Coping illustrating relationships among individual stress, coping, and quality of life [27], and 3) Social Network Theory pertinent to social support and sources [28], in order to explore the full range of sociocultural influences on breast cancer survivors’ adaptation to breast cancer and quality of life after treatment. In particular, the patient-physician communication questions guided by the Vulnerability Model inquired about patients’ experiences in obtaining oncology care after cancer diagnosis and treatment, expectations of communication and relationship with physicians, and attitudes toward patient-physician interactions (see specific questions in Table 1). Interview guides were written in English and Chinese languages. Chinese guides were back-translated to English to confirm semantic equivalence.
Table 1.
Interview Questions regarding Patient-Physician Communication
| Interview questions |
|---|
| 1. Now, I would like to talk about your medical care. How has your communication been with the doctor that you have seen most often since breast cancer diagnosis? |
| 2. Have you told your doctors about your aforementioned concerns and what you need from them? If not, Why not? |
| 3. Has your doctor spent enough time with you to answer your questions or to understand any problems? |
| 4. Has your doctor recommended any regular check-ups or exams? |
| 5. What would you like to change about your relationship or communication with your doctor? |
| 6. Have you experienced any difficulties with getting medical care since your breast cancer diagnosis? |
| 7. Do you think that you would have experienced these difficulties with getting medical care if you were living in your home country? [Why or Why not?] (Chinese immigrant group only). |
Qualitative interviews
We conducted four Chinese immigrant (n=19) and four NHW (n=22) focus groups, and individually interviewed 31 survivors (6 NHW, 7 US-born Chinese, 18 Chinese immigrants). Focus groups were conducted at CPIC and community centers in San Francisco’s Chinatown. Two of the Chinese focus groups were conducted in Mandarin and two in Cantonese. All of the US-born Chinese were individually interviewed in English. The first two authors conducted most of the qualitative interviews. A total of six Cantonese interviews were conducted by an experienced, trained Cantonese speaker. All interviewers were trained to follow the moderator guide to minimize variations in data collection. Participants received $35 compensation for a 1.5–2-hour interview. Interviews were audio-recorded and transcribed. Chinese language interviews were translated into English for analysis.
Data Analysis
Patient-physician communication was one of the dominant themes in this cross-cultural investigation. In this paper, we analyzed data on women’s discussion of their communication with physicians across the cancer care continuum, and the ways in which this communication helped them deal with their physical and emotional states. Based on the transcripts, we created a codebook taxonomy that consisted of broad thematic categories and specific codes within the categories. Two trained coders independently coded all interviews in order to make possible an unconstrained analysis of the data [29;30]. Data analyses followed established qualitative methods of content analysis [31]. Initial intercoder reliability was 86.1%; however, all text was discussed and ultimately coded to consensus.
RESULTS
Sample Characteristics
The average age of our Chinese and NHW survivors was 57.7 years old. All participants except one Chinese immigrant were insured. As displayed in Table 2, most of the Chinese American survivors were married (~80%) and able to speak English and Chinese languages (~64%). Approximately 86% of NHW and 100% of US-born survivors had college degrees compared to 49% of Chinese immigrant survivors. Chinese immigrant survivors had a higher percentage (32.4%) of annual household incomes below $30,000 compared to US-born Chinese and NHW survivors.
Table 2.
Sample Characteristics
| Non-Hispanic
White (N=28) |
Chinese Americans
(N=44) |
P value | ||
|---|---|---|---|---|
| US-Born (N=7) | Immigrant (N=37) | |||
| Average years in the US (S.D.) | * | - | 22.22 (14.67) | - |
| Average age (S.D.) | 58.5 (9.83) | 58.57 (6.5) | 56.9 (9.19) | - |
| Spoken language | <.0001 | |||
| Chinese only | 0 | 0 | 13 (36.11%) | |
| English and Chinese | 1 (3.57%) | 4 (57.14%) | 23 (63.89%) | |
| English only | 27 (96.43%) | 3(42.86%) | 0 | |
| Marital status | .0037 | |||
| Married | 13 (46.43%) | 6 (85.71%) | 29 (78.38%) | |
| Single | 15 (53.57%) | 1 (14.29%) | 8 (21.62%) | |
| Education | .0104 | |||
| ≤ High school | 4 (14.29%) | 0 | 19 (51.35%) | |
| > High school | 24 (85.71%) | 7 (100%) | 18 (48.65%) | |
| Employment status | .4822 | |||
| Employed | 17 (60.71%) | 1 (14.29%) | 22 (59.46%) | |
| Unemployed | 11 (39.29%) | 6 (85.71%) | 15 (40.54%) | |
| Annual household income | .0016 | |||
| < 30k | 0 | 0 | 12 (32.43%) | |
| 30k–69k | 6 (21.43%) | 2 (28.57%) | 11 (29.73%) | |
| 70k+ | 18 (64.29%) | 4 (57.14%) | 9 (24.32%) | |
| Unknown | 4 (14.29%) | 1 (14.29%) | 5 (13.51%) | |
| Health insurance | .0023 | |||
| Private | 25 (89%) | 6 (86%) | 21 (57%) | |
| Government | 3 (11%) | 1 (14%) | 15 (41%) | |
| No insurance | 0 | 0 | 1 (2%) | |
| †Stage of cancer | .7104 | |||
| 0 | 16 (57.14%) | 4 (57.14%) | 23 (62.16%) | |
| I | 9 (32.14%) | 3 (42.86%) | 7 (18.92%) | |
| II | 1 (3.57%) | 0 | 1 (2.7%) | |
| Don’t Know | 2 (7.14%) | 0 | 6 (16.22%) | |
| †Type of treatment | ||||
| Mastectomy | 6 (21.43%) | 2 (28.57%) | 16 (43.24%) | .1061 |
| Lumpectomy | 23 (82.14%) | 6 (85.71%) | 19 (51.35%) | .0132 |
| Chemotherapy | 1 (3.57%) | 0 | 1 (2.7%) | .7235 |
| Radiation | 13 (46.43%) | 5 (71.43%) | 15 (40.54%) | .8252 |
| †Survival months | .6476 | |||
| 0–12 months | 7 (25%) | 3 (42.86%) | 9 (24.32%) | |
| 13–24 months | 11 (39.29%) | 3 (42.86%) | 16 (43.24%) | |
| 25–36 months | 3 (10.71%) | 1 (14.29%) | 6 (16.22%) | |
| 36–45 months | 7 (25%) | 0 | 6 (16.22%) | |
Note. S.D. = Standard Deviation.
Stage of cancer, type of treatment, and survival months all were based on patient self-reported data.
Only one NHW participant was born in South Africa.
P-values were based on chi-square tests comparing the ethnic groups between NHW and Chinese Americans.
Patient-Provider Communication
When asked to talk about communication with physicians, women spoke about their surgeons, oncologists, radiation oncologists, and primary care physicians across the periods of diagnosis, treatment, and follow-up care. A number of similarities and differences were revealed among Chinese and NHW survivors with regard to perceptions, expectations, and reactions to physicians’ communication styles. In the following, we describe common themes across ethnic groups and then ethnic and cultural differences in communication with physicians. The narrative below is elaborated by quotes in Table 3.
Table 3.
Results of Thematic Analysis and Corresponding Quotes
| Themes | Original Quotes |
|---|---|
| Ethnic Similarities | |
| Empathetic communication at time of diagnosis | I only spoke with him (the medical oncologist) and it was early on, before the surgeries,…I think he was the first one to reassure me that this is not life-threatening; it's breast-threatening. (NHW, age 49, some college, income >$100k)† |
| The doctor said, “You seem to have a positive outlook so I think you’re going to be fine.” And I believed her. (US-born Chinese, age 53, some college, $60–70k) | |
| The doctor was very different from what I expected; I found that he took really good care of me during our interaction, so I gained a lot of confidence in him…I think doctors have to treat patients as humans,…so when the doctors tell patients news, first is the mammogram, then ultrasound, and biopsy. During the process, I think that doctors need to be very patient, to guide the patients and not just say do this or that, or just tell them the results. For patients, their heart sank and they feel very worried. (Chinese immigrant, age 58, some college, 33 yrs in US, $90–99k)* | |
| When I was diagnosed, I was very surprised. I would get very emotional, but my doctor told me I only had very little cancer in my body and I became calm after that. (Chinese immigrant, age 71, bachelor’s degree, 3 yrs in US, $30–40k)*# | |
| Factual communication during treatment phases | I have the best doctor in the world. He would call, “How’s everything? Good. Okay. Goodbye. I’ll talk to you later.” That’s the relationship I prefer. I don’t need any coddling. I did my part. He did his part. (NHW, age 54, some college, >$100k) |
| [My oncologist] was a bit of a pollyanna. I would have preferred someone more direct.(NHW, age 71, master level, $90–99k) | |
| Both surgeons were excellent, very supportive. When I did ask questions, they answered them…[The oncologist] gave me facts. She didn't mince words or anything…They were all very good. (US-born Chinese, age 59, college grad., $50–60k)# | |
| Interviewer: Are you satisfied with his communication? Patient: I'm satisfied with his medical knowledge. (Chinese immigrant, age 48, High school, 19 yrs in US, $30–40k)*# | |
| Let me tell you about my surgeon…She's very demanding and has very high standards for herself… my colleagues said, "She has a bad temper and I don't like her, but go to her."…So, this is the turning point. I viewed it from this angle, how she cared for me….I don’t know if she really has "sympathy", but she has high standards… When I looked in the mirror [at the wound], I saw a very neat line and I don't feel sad. (Chinese immigrant, age 58, some college, 33 yrs in US, $90–99k)* | |
| Seeking information for cancer care | I was always told if you have any further questions, please call. And, I would get a response… oh, within an hour or so, from either the general surgeon or the oncologist. And, that was really important. (NHW, age 54, college grad, >$100k) |
| My doctor told me it's normal to have pain after surgery. The cells in my body had not yet recovered, so I would feel pain. After my doctor explained why I still felt pain after several months, I felt better. (Chinese immigrant, age 45, some college, 34 yrs in US, <$10k)* | |
| I listened to the doctors and did whatever they told me. (Chinese immigrant, age 66, 25 yrs in US, $30–40k)*# | |
| Ethnic Differences | |
| Attitudes toward communication post treatment | There is a surprising lack of any kind of willingness or knowledge to support you as you go through this. (NHW, age 57, bachelor’s degree, $80–90k) |
| You know…I try to ask lots of questions. And, things that I don't understand, I ask for explanations. (US-born Chinese, age 59, bachelor degree, $50–60k)# | |
| The doctor’s time is very precious… [Previously], I would go to the doctor and then, Aiya! I forgot to ask him that question. So, the next time, I wrote down a list of things to ask him. Then, we discuss these things… I would change myself. You do not need to change the doctor. (Chinese immigrant, age 48, high school, 28 yrs in US, $50–60k)* | |
| I didn't ask the doctor; I don't know how many lymphs there are. I don't understand it… There is no metastasis in the lymph. None, but now my body is half numb…. The doctors are very busy. They don’t have a lot of time. They only answer what you ask them… The doctors are very good, each one of them… The problem is, they can't satisfy your answers… (Chinese immigrant, age 73, high school, 14 yrs in US, <$10k)*# | |
| Managing expectation | I think that they don’t wanna scare people from the treatment that they need. They just want people to be positive and go through it…So, they say, “You may experience slight discomfort.” They should say, “This is gonna hurt like heck and you’re going to be sore for at least two weeks, maybe five.”…There has to be clear communication about what sort of pain and duration of pain or level of pain, realistically, I could expect. (NHW, age 56, bachelor degree, >$100k) |
| I found that I had a red circle under my eyes…My face was swollen,…completely out of shape; it was horrible… But the doctor I met told me repeatedly that they he has never seen such symptoms. Then, there's nothing else I can do. (Chinese immigrant, age 61, master level, 38 yrs in US,> $100k)* | |
| (has pain from side effects but just deals with it because according to her): "The doctor will say, ‘It’s normal to have pain after surgery.' So, what can you do?" (Chinese immigrants, age 51, high school, 4 yrs in US, <$10k)* | |
| Difference in information seeking | I talked to my radiology oncologist and she assured me that it (a bruised feeling) is normal. There's nothing she and I can do about it. Now, I've read--I've done research online--and have looked into what you can do with scarred tissue, [like] can you massage it to reduce scarred tissue and pain and stuff like that. I just found out that my oncologist is leaving… I'll be seeing someone new, so maybe I'll get some new information from a new doctor. (NHW, age 49, some college, >$100k) |
| [In order to improve communication], I should read more magazines about seeing the doctor and know what I should ask. (Chinese immigrant, age 48, high school, 19 yrs in US, $30–40k)*# | |
| -Chinese and Primary care physicians: | |
| Some friends told me that right now you only have breast cancer, but the cancer cells might move to other parts of the body… That's why I'm nervous. I didn't feel right about my entire body, so I told my family doctor to take me to do screening. I told him about my concerns about being afraid that cancer would move to other places. (Chinese immigrant, age 45, some college, 34 yrs in US, <$10k)* | |
| [The oncologist] didn't even look at my wound, just talked to me…Well, I just went to the gynecologist the day before, and she checked my breast. (Chinese immigrant, age 61, master level, 38 yrs in US, >$100k)* | |
| Since mine was detected at the early stage, I asked my own family doctor for her opinion. My family doctor said I could decide for myself. With my own doctor having said that, along with the information I had collected about the sickness and my own understanding of it, I felt that I did not need to do it. If, however, my own doctor told me I should, I would have done it (had a mastectomy). (Chinese immigrant, age 52, high school, 3 yrs in US, $10–20k)*# | |
| -Language and communication: | |
| It's not a big problem in San Fran because there are Chinese interpreters. After surgery, the doctor is willing to show me my medical record, so it's not a [language] problem either. (Chinese immigrant, age 48, high school, 19 yrs in US, $30–40k)*# | |
| I speak both English and Chinese, so [language is] not a big problem… I prefer American doctors because their attitude is better and they really take good care of me. When they talk to me, I feel very comfortable. (Chinese immigrant, age 45, some college, 34 yrs in US, <$10k)* | |
| When you don't know how to "communicate," actually, if you have a language barrier, this is not the most important--it can be overcome. The problem is the communication channel; that is, whether the doctor is willing to listen or talk, whether the patient is willing to ask or learn. This needs to be built up in the beginning… I think communication is the most difficult, not the language. (Chinese immigrant, age 58, some college, 33 yrs in US, $90–99k)* | |
Inside the parenthesis, ethnicity, age, educational level, years of stay in the US, and annual household income level are sequentially listed.
Indicated that patient interview was conducted in Chinese languages (including Mandarin and Cantonese)
Indicated that patients were insured by a government plan.
Ethnic similarities
Overall, Chinese and NHW women reported comparable levels of satisfaction with physician communication at the time of diagnosis and treatment. They also expressed similar attitudes with regard to empathy at time of diagnosis and factual communication during the treatment phase. In addition, Chinese immigrant participants were certain that the care they received from physicians in the US was better than that which they would have received in Asia.
Empathic communication at time of diagnosis
Physician empathy was most important at the time of diagnosis among all ethnic groups. Sensitive responses along with reassurances that modern treatment is very effective and that the prognosis for survival was good assuaged women’s fears. For example, a team of physician-researchers was treating one of the US-born Chinese women. The team gave her prognostic “percentages for everything.” She was grateful for this information, but expressed even more appreciation for the physician’s reassurance that she would survive this disease. Empathy, on the other hand, was an attribute that women appreciated, but did not necessarily expect from physicians during the treatment period.
Factual communication during the treatment phase
Women reported that emotionally-charged discussions were rare during the treatment period. With a few of exceptions, NHW and Chinese women stated that they did not need or expect emotional support from physicians during this phase. Instead, encounters during this period focused more on facts regarding medical care and other information sharing. Women expected physicians to be knowledgeable about early stage cancer, and to provide evidence-based treatment options. Women wanted to know as much as possible about their prognosis, and they were willing to sacrifice bedside manner for more direct communication and a more skillful physician. For example, a NHW participant was warned that her physician did not have good bedside manner; however, she appreciated the doctor’s forthright attitude. One of the Chinese immigrant participants worked at a hospital. She was referred to a physician at that hospital who was criticized for her attitude, but lauded for her surgical skills. She went on to say that the physician had “very high standards for herself” and stitched her wound with amazing care and precision.
Information seeking for cancer care
All women stated that physicians were their primary source for information about treatment options, follow-up care, and physical distress. Many of the Chinese and NHW women complained about the unexpected and persistent side effects associated with radiation and hormonal treatment. Both NHW and Chinese participants expected medical interventions that would relieve some of their discomfort, or at least clear explanations for why side effects persisted.
Ethnic differences
The results showed that Chinese and NHW survivors’ perceptions of, and attitudes toward, medical communication diverged from each other in a few ways. Cultural differences in communication between the two groups were mostly related to post treatment follow-up.
Attitudes toward communication post treatment
While women in all groups thought that post-treatment follow-up was the point at which the quality of physician communication declined, responses to this decline varied by ethnic group. NHW and US-born Chinese women were more likely to compel doctors to respond to their concerns (i.e., physical symptoms and side effects) until they were satisfied and to engage in shared-decision making. In contrast, Chinese immigrant participants were more passive, accepting whatever physicians said in response to their concerns. For example, one Chinese immigrant survivor who was still experiencing numbness, simultaneously praised the doctors and disclosed that she had unresolved questions and problems (see the quote in Table 3). Highly acculturated Chinese immigrant women—those with greater English proficiency, higher incomes and education levels—were more likely to challenge physicians, in the same manner as NHW and US-born Chinese women. Moreover, relative to NHW women, highly acculturated and US-born Chinese women reported having to invest more time in conversation (via phone or face-to-face contact) with physicians in order to get referrals or relief from side effects. A US-born Chinese survivor suffered with serious pain which was not alleviated by the pain medication that her doctor prescribed. After doing research to identify resources that may be available to her, she returned to the physician and requested a referral to a physical therapist.
Managing expectations
In the context of post-treatment communication, some women noted that physicians did not warn them about side effects prior to prescribing treatments. More NHW and US-born Chinese women were outspoken about this deficiency relative to Chinese immigrants. For example, NHW women felt that doctors deliberately withheld information, and that they should have been more forthright about the pain and discomfort associated with cancer treatment. NHW women said that physicians did not mentally prepare them for the emotional distress associated with changes to their physical appearance (e.g., scars, weight gain, radiation tattoos). Still, NHW commented that they understood that physicians were most concerned about removing the cancer and preventing recurrence.
In contrast, Chinese immigrant women spoke favorably about physicians even if their post-treatment experiences were not congruent with their expectations. Contrary to NHW women and US-born Chinese, none of Chinese immigrants said that they were ill-prepared to manage their physical distress; that there was any inconsistency between what physicians told them prior to treatment and what they were experienced post treatment; or that physicians failed to help them anticipate the emotional distress associated with changes in physical appearance. Furthermore, Chinese immigrants tended to be considerate of physicians’ time restraints. In one example, a Chinese immigrant participant stated that she felt rushed, but added, “The doctor’s time is very precious.” When asked if there was anything that she would change about her communication with her doctor, she said, “I would change myself” (quote continued in Table 3).
Difference in information seeking
Chinese immigrant participants were more likely to state that they left their physician’s office with unanswered questions and unresolved issues. In other words, they were less likely to request the additional information that they needed. For example, one of the Chinese participant’s whose arm was still numb from surgery, but said that her communication with her physician was superb. Results indicated that Chinese immigrants were more likely to discuss their physical problems with, and obtain information from their primary care physicians (PCPs) in addition to their cancer specialists. This was true regardless of income or educational status. While it is probable that all of the women had relationships with their PCPs that predated cancer, Chinese immigrant women were more likely than other groups to perceive their PCPs as central to their cancer care. For example, one Chinese immigrant had two surgeries and experienced severe side effects. She was dissatisfied with the feedback she received from her surgeon and the lack of personal attention. She stated that it was her gynecologist (whom she saw for primary care) who checked her wound. She added that she is able to contact her gynecologist via e-mail and she typically receives a response within 24 hours. In another example, a Chinese immigrant participant was satisfied with her surgeon and described him as being thorough; however, she had known her family doctor for approximately 15 years and communicated with him throughout her treatment experience.
Chinese immigrant women’s narratives indicated that anticipated challenges resulting from patient-provider language discordance were minimal because many Bay Area medical facilities have resources for the Chinese population. The conditions that facilitated communication were: translators in the healthcare system, friends or family members who translated for them, Chinese physicians, and their own English proficiency. Five Chinese women explicitly stated that they faced language barriers, but none of them questioned the quality of the care they received. The most dominant sentiment among immigrant Chinese women was that “communication” is more important than “language.” These Chinese immigrant survivors said that language discordance is not always the greatest barrier and they were willing to deal with the language barriers if they believed that they were receiving high quality cancer care.
DISCUSSION
In this study, regardless of ethnicity or birthplace, communication with physicians was essential for patients to handle their breast cancer diagnosis, treatment, and post-treatment care. Our results indicate that breast cancer patients not only need an empathetic physician who understands their illness experiences, but also a competent physician who provides a cure for their cancer and helps to alleviate symptoms associated with their cancer treatment. Thus, physicians’ ability to communicate helpful advice and complete information was key to patients’ comfort regarding prognosis and treatment. For cancer patients, unresolved physical problems often prompt emotional uncertainty about prognosis, [19;32;33]. Our findings support prior survivor-physician research [34;35] showing that survivors perceived optimal quality of care when they experienced satisfactory patient-centered communication with physicians. Empirical research has also shown that patient-centered communication has short-term and long-term impacts on cancer patients’ mental health [5;36–38].
Our qualitative results might explain epidemiological findings that Chinese Americans are more likely to have poorer quality physician communication and more unmet needs for survivorship care than other ethnic groups [12;13;39]. This ethnic difference is likely related to cultural respect for physicians and the expectation of limited information-sharing related to this respect. In Asian cultures, patients defer to physicians, respecting the physicians’ authority and trusting the physician to do what is in the best interest of the patient [16]. Traditional Chinese values do not emphasize patient autonomy and shared decision-making in medical encounters [40]. Therefore, our Chinese immigrant patients appeared to be less proactive and assertive in expressing their unmet cancer care needs to physicians compared to NHW and US-born Chinese survivors. Unfortunately, failure to obtain information from and question physicians, regardless of the cause, can adversely affect patients’ satisfaction with care. Research has shown that Chinese American cancer patients reported more unresolved physical symptoms than their NHW counterparts [13]. It is a typical notion that language discordance between immigrant patients and physicians can impede quality communication [41]. However, our Chinese immigrant survivors said that language concordance does not ensure optimal communication. Empirical research indicates that the quality of patient-physician communication is more important than English ability in explaining ethnic disparities in physical and emotional distress between Spanish-speaking Latino and Whites breast cancer patients [3].
Ethnic variations in the accessibility of cancer care information may also contribute to Chinese immigrants’ disadvantages in communication with physicians. Many of our Chinese immigrants had lived in the US for over 20 years, but they could not be interviewed in English. Plus, our Chinese immigrants had lower socioeconomic status (i.e., education and income) than their NHW and US-born counterparts. It is likely that the former have less access to scientific based, linguistically appropriate materials about cancer treatments and survivorship care than the other groups. Previous studies indicate that NHW, and more educated patients are more likely to have satisfactory communication with their physicians and get their physical problems resolved [3;19;42;43]. Given the qualitative nature of this study, our current findings could not explain to what extent acculturation and sociodemographics compound the dynamics of patient-physician communication. Empirical investigation of ethnic differences in cancer care communication will need to take these sociocultural factors into account.
These language and cultural factors might have caused Chinese immigrant survivors to seek care from their primary care physicians more than specialists. Chinese immigrant patients probably feel more comfortable asking their primary care physician questions, especially when there is mutual trust built over a long-term relationship and when they share the same language and cultural background. Our data showed that visits to the primary care physician were beneficial for immigrant survivors to receive supplemental information and care. Further investigation of the role of primary care physicians in cancer care continuum among minority immigrants is needed.
This study has several limitations. First, our findings are limited to retrospective patient narratives. Prospective observation of actual patient-physician encounters throughout the cancer care continuum would strengthen this research. Second, our Chinese and NHW samples were early-stage breast cancer survivors. The results of our study may not be generalized to women diagnosed at later stages, with other cancer types, or from different racial groups, as they may have different experiences. Third, our Chinese patients were sampled from the Greater San Francisco Bay area where resources (e.g., Chinese cancer support groups, interpreter services, and media) for Chinese are more abundant than in most areas in the US. Consequently, research such as this should be conducted in communities where fewer resources are available.
In conclusion, while patients who are oriented in different cultural philosophies and values have common needs for cancer care, they are likely to have different communication styles with physicians [11;44]. Surbone (2008) emphasized that oncologists should be sensitive to cancer patients’ cultural backgrounds in order to effectively communicate with them and deliver optimal care [1]. The results of this study underscore the importance of culture in patient-physician communication. At the same time, the findings provide direction for further research on interventions that may improve communication between Chinese immigrant patients and their physicians through linguistically appropriate educational programs and culturally competent oncology care.
Acknowledgements
This research was supported by a Lance Armstrong Foundation Young Investigator Award and the National Cancer Institute R21 Grant# CA139408. This research was also supported by the National Cancer Institute's Surveillance, Epidemiology and End Results Program under contract HHSN261201000040C awarded to the Cancer Prevention Institute of California. The collection of cancer incidence data used in this study was supported by the California Department of Health Services as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute's Surveillance, Epidemiology, and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under agreement #1U58 DP000807-01 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the authors, and endorsement by the State of California, the California Department of Health Services, the National Cancer Institute, or the Centers for Disease Control and Prevention or their contractors and subcontractors is not intended nor should be inferred.
We appreciate field staff at CPIC, Pagan Morris, Mei-chin Kuo, Kathie Lau, and Daisy Lubag for their efforts in participant enrollment and preparation for focus groups. We sincerely thank Dr. Frances M. Lewis for her constructive comments on the interview guides to enhance our qualitative data collection.
Footnotes
Conflict of Interest
None of the authors of this article have any conflicts of interest, as they have no financial affiliations with the organizations that sponsored the research to affect the ethical conduct of this study and authorship. The first author has full control of all primary data and agrees to allow the journal to review the data if requested.
Reference List
- 1.Surbone A. Cultural aspects of communication in cancer care. Support Care Cancer. 2008;16:235–240. doi: 10.1007/s00520-007-0366-0. [DOI] [PubMed] [Google Scholar]
- 2.Neumann M, Wirtz M, Bollschweiler E, Mercer SW, Warm M, Wolf J, Pfaff H. Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. Patient Educ Couns. 2007;69:63–75. doi: 10.1016/j.pec.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Maly RC, Liu Y, Leake B, Thind A, Diamant AL. Treatment-related symptoms among underserved women with breast cancer: the impact of physician-patient communication. Breast Cancer Res Treat. 2010;119:707–716. doi: 10.1007/s10549-009-0418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zachariae R, Pedersen CG, Jensen AB, Ehrnrooth E, Rossen PB, von der MH. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br J Cancer. 2003;88:658–665. doi: 10.1038/sj.bjc.6600798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mager WM, Andrykowski MA. Communication in the cancer 'bad news' consultation: patient perceptions and psychological adjustment. Psychooncology. 2002;11:35–46. doi: 10.1002/pon.563. [DOI] [PubMed] [Google Scholar]
- 6.Kornblith A. Holland J, Breitbart W, Jacobsen P, Lederberg M, Loscalzo M, Massie M, McCorkle R, editors. Psychological Adaptation to Cancer. Psycho-Oncology. 1998:223–241. [Google Scholar]
- 7.Epstein RM, Street RL., Jr . National Cancer Institute, NIH Publication No. 07-6225. Bethesda, MD: 2007. Patient-centered communication in cancer care: promoting healing and reducing suffering. [Google Scholar]
- 8.Roter DL, Hall JA, Katz NR. Relations between physicians' behaviors and analogue patients' satisfaction, recall, and impressions. Med Care. 1987;25:437–451. doi: 10.1097/00005650-198705000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Ngo-Metzger Q, Legedza AT, Phillips RS. Asian Americans' reports of their health care experiences. Results of a national survey. J Gen Intern Med. 2004;19:111–119. doi: 10.1111/j.1525-1497.2004.30143.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang JH, Sheppard VB, Schwartz MD, Liang W, Mandelblatt J. Disparaties in cervical cancer screening between Asian and non-Hispanic White women. Cancer Epidemiol Biomarkers Prev. 2008;17:1968–1973. doi: 10.1158/1055-9965.EPI-08-0078. [DOI] [PubMed] [Google Scholar]
- 11.Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. J Gen Intern Med. 2004;19:101–110. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ayanian JZ, Zaslavsky AM, Arora NK, Kahn KL, Malin JL, Ganz PA, van RM, Hornbrook MC, Kiefe CI, He Y, Urmie JM, Weeks JC, Harrington DP. Patients' experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2010;28:4154–4161. doi: 10.1200/JCO.2009.27.3268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palmer NRA, Arora NK, Kent E, Forsythe L, Rowland JH, Aiz N, Weaver KE. Racial-ethnic disparities in patient-provider communication and overall perceptions of follow-up care quality among adult cancer survivors; The fifth AACR conference in the Science of Cancer Health Disparities; San Diego, California. 2012. [Google Scholar]
- 14.Dhooper SS. Health care needs of foreign-born Asian Americans: an overview. Health Soc Work. 2003;28:63–73. doi: 10.1093/hsw/28.1.63. [DOI] [PubMed] [Google Scholar]
- 15.Wang JH, Liang W, Schwartz MD, Lee MM, Kreling B, Mandelblatt JS. Development and evaluation of a culturally tailored educational video: changing breast cancer-related behaviors in Chinese women. Health Educ Behav. 2008;35:806–820. doi: 10.1177/1090198106296768. [DOI] [PubMed] [Google Scholar]
- 16.Hsu WC, Yoon HH. Building cultural competency for improved diabetes care: Asian Americans and diabetes. J Fam Pract. 2007;56:S15–S21. [PubMed] [Google Scholar]
- 17.Kagawa-Singer M, Blackhall LJ. Negotiating cross-cultural issues at the end of life: "You got to go where he lives". JAMA. 2001;286:2993–3001. doi: 10.1001/jama.286.23.2993. [DOI] [PubMed] [Google Scholar]
- 18.Kreuter MW, McClure SM. The role of culture in health communication. Annu Rev Public Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- 19.Wang JH, Adams I, Huang E, Ashing-Giwa K, Gomez SL, Allen L. Physical distress and cancer care experiences among Chinese-American and non-Hispanic White breast cancer survivors. Gynecol Oncol. 2012;124:383–388. doi: 10.1016/j.ygyno.2011.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pew Reseach Center. [Accessed 18 March 2013];The Rise of Asian Americans. 2012 http://www.pewsocialtrends.org/files/2012/06/SDT-The-Rise-of-Asian-Americans-Full-Report.pdf.
- 21.Killoran M, Moyer A. Surgical treatment preferences in Chinese-American women with early-stage breast cancer. Psychooncology. 2006;15:969–984. doi: 10.1002/pon.1032. [DOI] [PubMed] [Google Scholar]
- 22.Ashing-Giwa KT, Padilla G, Tejero J, Kraemer J, Wright K, Coscarelli A, Clayton S, Williams I, Hills D. Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psychooncology. 2004;13:408–428. doi: 10.1002/pon.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quach T, Nuru-Jeter A, Morris P, Allen L, Shema SJ, Winters JK, Le GM, Gomez SL. Experiences and perceptions of medical discrimination among a multiethnic sample of breast cancer patients in the Greater San Francisco Bay Area, California. Am J Public Health. 2012;102:1027–1034. doi: 10.2105/AJPH.2011.300554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kvale S, Brinkmann S. Interviews: Learning the Craft of Qualitative Research Interviewing. Los Angeles, CA: Sage; 2009. [Google Scholar]
- 25.Krueger RA, Casey MA. A Practical Guide for Applied Research. ed 4. Los Angeles, CA: Sage; 2009. Focus Groups. [Google Scholar]
- 26.Bernard HR. Research Methods in Anthropology Qualitative And Quantitative Methods. United Kingdom: Plymouth, AltaMira Press; 2002. [Google Scholar]
- 27.Glanz K, Schwartz M. Stress, coping, and health behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education Theory, Research and Practice. San Francisco, CA: Jossey-Bass; 2008. pp. 212–236. [Google Scholar]
- 28.Heaney C, Israel B. Social networks and social support. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education Theory, Research and Practice. San Francisco, CA: Jossey-Bass; 2008. pp. 189–210. [Google Scholar]
- 29.Saldana J. The coding manual for qualitative researchers. Thousand Oaks, CA: Sage Publication; 2009. [Google Scholar]
- 30.Fossey E, Harvey C, McDermott F, Davidson L. Understanding and evaluating qualitative research. Aust N Z J Psychiatry. 2002;36:717–732. doi: 10.1046/j.1440-1614.2002.01100.x. [DOI] [PubMed] [Google Scholar]
- 31.LeCompte MD, Schensul JJ. Analyzing and interpreting ethnographic data. In: Schensul JJ, LeCompte MD, editors. Ethnographer's Toolkit. Baltimore MD, USA: Altamira Press; 1999. [Google Scholar]
- 32.Clayton MF, Dudley WN, Musters A. Communication with breast cancer survivors. Health Commun. 2008;23:207–221. doi: 10.1080/10410230701808376. [DOI] [PubMed] [Google Scholar]
- 33.Miller LE. Sources of uncertainty in cancer survivorship. J Cancer Surviv. 2012;6(4):431–40. doi: 10.1007/s11764-012-0229-7. [DOI] [PubMed] [Google Scholar]
- 34.Lawler S, Spathonis K, Masters J, Adams J, Eakin E. Follow-up care after breast cancer treatment: experiences and perceptions of service provision and provider interactions in rural Australian women. Support Care Cancer. 2011;19:1975–1982. doi: 10.1007/s00520-010-1041-4. [DOI] [PubMed] [Google Scholar]
- 35.Arora NK, Reeve BB, Hays RD, Clauser SB, Oakley-Girvan I. Assessment of Quality of Cancer-Related Follow-Up Care From the Cancer Survivor's Perspective. J Clin Oncol. 2011;29:1280–1289. doi: 10.1200/JCO.2010.32.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Institute of Medicine. Cancer Care for the Whole Patient: Meeting psychosocial health needs. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 37.Silliman RA, Dukes KA, Sullivan LM, Kaplan SH. Breast cancer care in older women: sources of information, social support, and emotional health outcomes. Cancer. 1998;83:706–711. [PubMed] [Google Scholar]
- 38.Butow P, Bell M, Goldstein D, Sze M, Aldridge L, Abdo S, Mikhail M, Dong S, Iedema R, Ashgari R, Hui R, Eisenbruch M. Grappling with cultural differences; communication between oncologists and immigrant cancer patients with and without interpreters. Patient Educ Couns. 2011;84:398–405. doi: 10.1016/j.pec.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 39.Blendon RJ, Buhr T, Cassidy EF, Perez DJ, Sussman T, Benson JM, Herrmann MJ. Disparities in physician care: experiences and perceptions of a multi-ethnic America. Health Affairs. 2008;27:507–517. doi: 10.1377/hlthaff.27.2.507. [DOI] [PubMed] [Google Scholar]
- 40.Tom LASH. Health and health care for Chinese American Elder. [Accessed March 19, 2013];University of Hawaii. 2001 http://www.stanford.edu/group/ethnoger/chinese.html.
- 41.Green AR, Ngo-Metzger Q, Legedza AT, Massagli MP, Phillips RS, Iezzoni LI. Interpreter services, language concordance, and health care quality. Experiences of Asian Americans with limited English proficiency. J Gen Intern Med. 2005;20:1050–1056. doi: 10.1111/j.1525-1497.2005.0223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cooper Lisa A, Debra L Roter: Unequal Treatment. Confronting Racial and Ethnic Disparities in Health Care (full printed version) The National Academies Press; 2003. [PubMed] [Google Scholar]
- 44.Ngo-Metzger Q, Massagli MP, Clarridge BR, Manocchia M, Davis RB, Lezzoni LI, Philips RS. Linguistic and cultural barriers to care: perspectives of Chinese and Vietnamese immigrants. J Gen Intern Med. 2003;18:44–52. doi: 10.1046/j.1525-1497.2003.20205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]