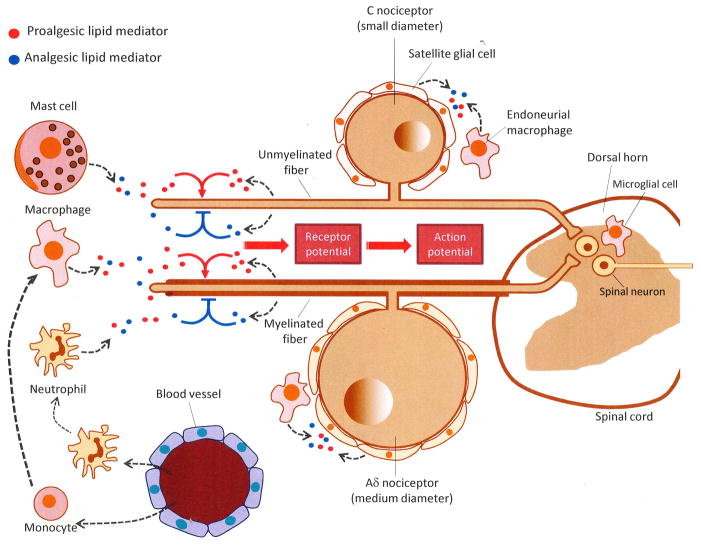
Figure 1. Peripheral gating of nociceptive signals by endogenous lipid mediators.
From the dorsal root ganglia (DRG), where the cell bodies of C and Aδ sensory neurons are located, nociceptive fibers travel both peripherally (to innervate skin, bone, viscera and other internal organs) and centrally (to form synapses with neurons in the dorsal horn of the spinal cord). Peripheral nociceptor terminals respond to acute injury directly, through cell-surface receptors specialized in detecting harmful physical and chemical stimuli, as well as indirectly, through receptors that sense proalgesic (pain-inducing) factors released by cell damage, inflammation, neuropathy or tumor growth (e.g., nucleotides, peptides and various lipid mediators). These sensitizing effects may be modulated by analgesic lipid-derived mediators generated at different stages of the tissue response to damage and under the control of neural and hormonal signals (e.g., autonomic nervous system, circulating corticosteroids). Some of these compounds may be released from the sensory nerve endings themselves, while others may derive from local host-defense cells, such as resident mast cells and macrophages, epidermal keratinocytes and blood-borne leukocytes recruited to the injury site. Nociceptive nerve endings integrate the inputs provided by proalgesic (excitatory) and analgesic (inhibitory) signals, converting them into graded receptor potentials and, eventually, all-or-none action potentials. Alterations in the production of analgesic lipid mediators may occur not only at the nerve endings of primary afferents, but also within the DRG and dorsal horn of the spinal cord, with neurons and other cells (e.g., satellite cells, endoneurial macrophages, microglia) likely contributing to this response.