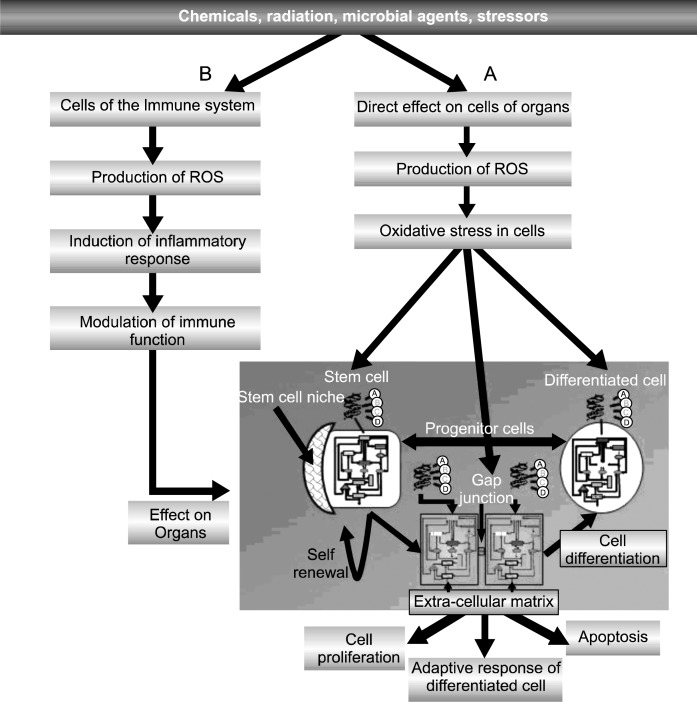
Fig. 3.
The diagram tries to incorporate a “systems” aspect of how a physical, chemical or biological agent could affect a multi-cellular organism. At non-cytotoxic concentrations or doses, an agent could simultaneously trigger oxidative stress in both the cells of the immune tissues and the epithelial/ endothelial/ stromal cells in various organs. Upon induction of reactive oxygen species (ROS) and of oxidative stress induction of intra-cellular signaling in various cell types of the complex immune system, various cytokines would interact on tissues, containing the three fundamental cell types (adult stem cells, progenitor and terminally-differentiated cells). Given that these cells would have been exposed to the toxic agent and that they, also, would have reacted to the agent differentially because of their different physiological/phenotypic state, the interaction of all three types could be very different (e.g., the normal stem cells might be induced to proliferate asymmetrically; any initiated pre-cancerous stem cell might proliferate symmetrically; the progenitor cells might be induced to proliferate symmetrically and to migrate, as in wound healing; and the terminally differentiated cell might adaptively respond or to apoptose) in response to the inflammatory signal. In summary, each cell type of the immune system and of the various organ tissues, with their different expressed genes and cellular physiology, will respond differently to sub-lethal exposure to agents inducing oxidative stress triggered intra-cellular signaling and epigenetic alterations. The interaction of inflammatory agents on pre-exposed organ epithelial cells could be an additive effect, a synergistic response or possibly, even an antagonistic effect. This could explain the wide range of diseases in which the inflammatory process seems to play a prominent role.