Abstract
Background and Purpose:
Today no method of topical anesthesia for intravitreal injection administration has been proven to make the patient comfortable yet. We compared the efficacy of topical levobupivacaine 0.75% and proparacaine 0.5% in patients undergoing intravitreal injections.
Materials and Methods:
A prospective, randomized study comparing two agents for topical anesthesia in intravitreal injections. Ninety-six consecutive patients were enrolled into two groups to receive either topical levobupivacaine 0.75% (n=48) or proparacaine 0.5% (n=48). Patients were asked to score their pain using a visual analog scale (VAS) immediately following the injection. The average of these scores was used as the primary outcome. The surgeon performing the procedure scored his perception of the patients’ pain using the Wong-Baker FACES scale.
Results:
Mean VAS pain scores for two groups were found to be 44.77 ± 16.42 and 34.18 ± 14.83, respectively. Mean VAS pain score in the proparacaine group was significantly lower than that in the levobupivacaine group (P= 0.003). Mean Wong-Baker FACES scores for the two groups were 1.08 ± 0.49 and 1.10 ± 0.30, respectively. There was no statistically significant difference between levobupivacaine and proparacaine groups (P=0.824).
Conclusions:
Topical proparacaine 0.5% was more effective in preventing pain during intravitreal injections.
Keywords: Anesthetic effectiveness, topical levobupivacaine, topical proparacaine, intravitreal injections
INTRODUCTION
Intravitreal injection is a preferred route of delivering various therapeutic agents to the posterior segment of the eye. However, it may be associated with significant patient anxiety and discomfort and carries risk of complications such as endophthalmitis, vitreous hemorrhage, retinal detachment, and traumatic cataract.[1,2] As the number of intravitreal pharmacologic agents with sustained delivery systems increase, many patients will require ongoing treatments with monthly or near-monthly injections. Therefore, an ocular anesthesia that will minimize patient discomfort and risk of complication is important to consider when using intravitreally administered drugs.
Numerous methods of local anesthesia for intravitreal injection have been compared including peribulbar and subconjunctival anesthetic injections as well as the use of anesthetic eye drops, gels, and anesthetic-soaked pledgets.[3,4,5,6,7,8,9] Today, no method of topical anesthesia for intravitreal injection administration has been proven to make the patient comfortable yet. Levobupivacaine is the isomer of bupivacaine and it is routinely used to provide regional anesthesia. In the current literature, there is no study evaluating the anesthetic effectiveness of topical levobupivacaine for intravitreal injections.
In this study, we evaluated and compared the efficacy of topical application of levobupivacaine 0.75% and proparacaine 0.5% in patients undergoing intravitreal drug administration.
MATERIALS AND METHODS
This prospective and randomized study compared the anesthetic effectiveness of Group 1: levobupivacaine 0.75% and Group 2: proparacaine 0.5% for intravitreal injections. The study was carried out at Kirikkale University Hospital. The research was reviewed and approved by Institutional Review Board. All participants gave written informed consent prior to their participation. The study was done in adherence to the tenets of the Declaration of Helsinki.
All patients who were scheduled to receive intravitreal ranibizumab (Lucentis; Genentech, Inc.) or triamcinolone acetonide (Kenacort; Bristol, MS) for one eye were evaluated for inclusion into the study. Patients were excluded if they had a history of past ocular surgery or intravitreal injection, a history of thromboembolic events, or a previously known allergic response to the topical anesthetics to be used.
Patients approved for the study were randomized to one of the two treatment groups. The anesthetic was administered by one of two nurses both having been trained in and experienced with the technique. Two drops of topical anesthetic were applied each time. All intravitreal injections were performed in the supine position under sterile conditions. The eye and the skin around it were washed three times by 4% povidone — iodine solution and then dried with sterile gauze. A sterile ophthalmic drape was then used to move the eyelashes away from the ocular surface. A sterile speculum was used to make sure the eyelids remain open. Four percent of povidone — iodine was again applied to the conjunctiva. Calipers were used to measure the injection site at 4 mm from the limbus, where ranibizumab or triamcinolone acetonide were injected intravitreally. Each time, the same ophthalmic surgeon (KÖ) was invited into the treatment room, with the anesthetic concealed, and performed the intravitreal injection. All injections were performed using a straight injection technique with a 30-gauge needle. Mild pressure was applied with a swabstick over the injection site to reduce vitreal reflux and subconjunctival hemorrhage. Three drops of antibiotic was applied at the end of the procedure.
Immediately following the injection, a study coordinator explained the 100-mm visual analog scale (VAS) for pain [Figure 1] and asked the subject the level of pain he or she experienced during the injection. The VAS scale is commonly used for the evaluation of ocular pain severity and relief. Those who could not adequately visualize the scale were prompted to vocalize a number from 0 to 100. A separate pain scale was employed to record physician-perceived pain. The Wong-Baker FACES scale [Figure 2] was chosen primarily for its ease of use. It has been studied as an observer scale and has prior use in ophthalmic analgesia. The specialist recorded his perception of the subjects’ pain experience shortly after the procedure.
Figure 1.
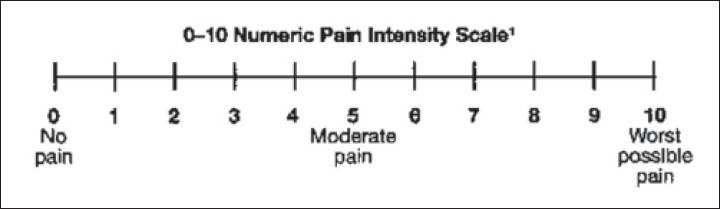
Visual analog scale for pain
Figure 2.
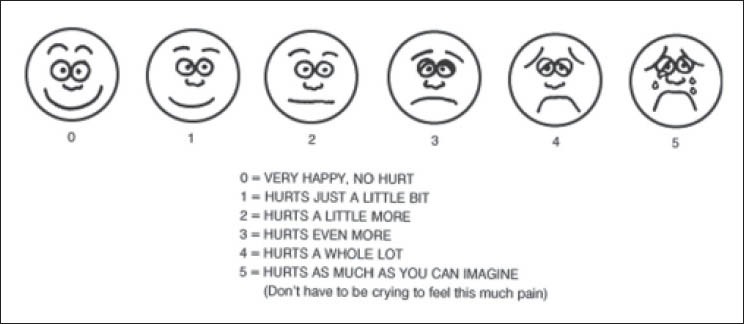
Wong-Baker FACES pain rating scale
Demographic and procedural characteristics between groups were compared using descriptive statistics and univariate analysis as appropriate. One-way analysis of variance was used to compare the outcomes. All statistical analyses were performed using the SPSS software system, version 18.0 (SPSS Inc., Chicago, Illinois, USA).
RESULTS
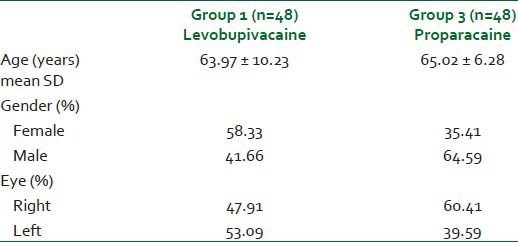
Each injection group contained 48 eyes of 48 patients. Table 1 shows the demographic data of two study groups. There was no statistically significant difference between the groups with respect to age, gender, or treated eye. The mean age was 63.97 ± 10.23 years (range 44-83 years) for Group 1, and 65.02 ± 6.28 years (range 51-82 years) for Group 2. The percentage of patients who were female was 58.33% for Group 1 and 35.41% for Group 2. The percentage of patients who had the right eye treated was 47.91% for Group 1 and 60.41% for Group 2.
Table 1.
Demographic data of two study groups
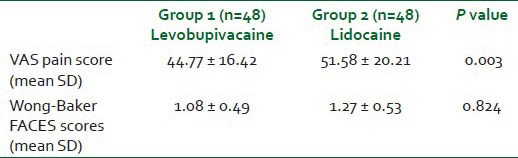
Mean VAS pain scores for two groups were found to be 44.77 ± 16.42 and 34.18 ± 14.83, respectively. Mean VAS pain score in the proparacaine group was significantly lower than that in the levobupivacaine group (P= 0.003). Mean Wong-Baker FACES scores for the two groups were 1.08 ± 0.49 and 1.10 ± 0.30, respectively [Table 2]. There was no statistically significant difference between levobupivacaine and proparacaine groups (P = 0.824).
Table 2.
VAS and Wong-Baker FACES scores in both groups
The rate and severity of intraoperative complications were similar between the two groups. No complications were encountered in the levobupivacaine and proparacaine groups.
DISCUSSION
In the recent years, there has been increasing use of intravitreal medications, such as steroids and anti-vascular endothelial growth factors worldwide to treat macular diseases like macular edema and age-related macular degeneration. Currently, no method of topical anesthesia prior to intravitreal injection administration has been proven to eliminate pain completely. In PubMed-based search of the current literature, although the efficacy of topical proparacaine has been well documented to date, we were unable to find any studies on the use of levobupivacaine as a topical anesthetic in intravitreal injection procedures.
In this study, we aimed to determine the efficacy of two topical anesthetic agents used in intravitreal injection by comparing the patients’ subjective pain evaluations and surgeon-perceived pain scores. Both topical levobupivacaine and proparacaine provided satisfactory analgesia during the procedure. The mean VAS pain score in the proparacaine group was significantly lower than that in the levobupivacaine group. However, there was no statistically significant difference between levobupivacaine and proparacaine groups for mean Wong-Baker FACES scores.
Davis et al. have determined that the use of topical proparacaine drops, compared to 4% lidocaine solution or 3.5% lidocaine gel, provided a very effective and cost-effective anesthesia during office-based intravitreal injections.[8] In a study by Blaha et al., proparacaine drops had the lowest average combined pain score associated with the intravitreal injection.[9] Cintra et al. also compared topical proparacaine drops, 2% xylocaine subconjunctival injection, and peribulbar injection of 2% xylocaine for anesthesia before intravitreal injection in 60 patients. They reported no significant difference in pain scores between topical drops and subconjunctival injection for both the injection-related pain scores and the entire procedure pain scores.[7]
Levobupivacaine has been introduced into clinical practice within the last few years. As a result of its lower cardiac and neurotoxicity compared to racemic bupivacaine, anesthetists feel safer working with levobupivacaine, than with bupivacaine. In this study, we found that although both anesthetics are effective, pain reported by patients during the injection was less in the proparacaine group. Surgeon-perceived pain scores were similar between the two groups. There were also no differences between the two groups in postoperative corneal epithelial defects, indicating a similar iatrogenic effect of both drugs.
According to the results of our study, we may conclude that topical proparacaine 0.5% was more effective than topical levobupivacaine in preventing pain during intravitreal injections. No difference was observed in corneal epithelial toxicity between the groups during the study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Veritti D, Di Giulio A, Sarao V, Lanzetta P. Drug safety evaluation of intravitreal triamcinolone acetonide. Expert Opin Drug Saf. 2012;11:331–40. doi: 10.1517/14740338.2012.635141. [DOI] [PubMed] [Google Scholar]
- 2.Day S, Acquah K, Mruthyunjaya P, Grossman DS, Lee PP, Sloan FA. Ocular complications after anti-vascular endothelial growth factor therapy in Medicare patients with age-related macular degeneration. Am J Ophthalmol. 2011;152:266–72. doi: 10.1016/j.ajo.2011.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kozak I, Cheng L, Freeman WR. Lidocaine gel anesthesia for intravitreal drug administration. Retina. 2005;25:994–8. doi: 10.1097/00006982-200512000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Kaderli B, Avci R. Comparison of topical and subconjunctival anesthesia in intravitreal injection administrations. Eur J Ophthalmol. 2006;16:718–21. doi: 10.1177/112067210601600509. [DOI] [PubMed] [Google Scholar]
- 5.Friedman SM, Margo CE. Topical gel vs subconjunctival lidocaine for intravitreous injection: A randomized clinical trial. Am J Ophthalmol. 2006;142:887–8. doi: 10.1016/j.ajo.2006.06.033. [DOI] [PubMed] [Google Scholar]
- 6.Yau GL, Jackman CS, Hooper PL, Sheidow TG. Intravitreal injection anesthesia-comparison of different topical agents: A prospective randomized controlled trial. Am J Ophthalmol. 2011;151:333–7. doi: 10.1016/j.ajo.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 7.Cintra LP, Lucena LR, Da Silva JA, Costa RA, Scott IU, Jorge R. Comparative study of analgesic effectiveness using three different anesthetic techniques for intravitreal injection of bevacizumab. Ophthalmic Surg Lasers Imaging. 2009;40:13–8. doi: 10.3928/15428877-20090101-05. [DOI] [PubMed] [Google Scholar]
- 8.Davis MJ, Pollack JS, Shott S. Comparison of topical anesthetics for intravitreal injections: A randomized clinical trial. Retina. 2012;32:701–5. doi: 10.1097/IAE.0b013e31822f27ca. [DOI] [PubMed] [Google Scholar]
- 9.Blaha GR, Tilton EP, Barouch FC, Marx JL. Randomized trial of anesthetic methods for intravitreal injections. Retina. 2010;10:1–5. doi: 10.1097/IAE.0b013e3181eac724. [DOI] [PubMed] [Google Scholar]


