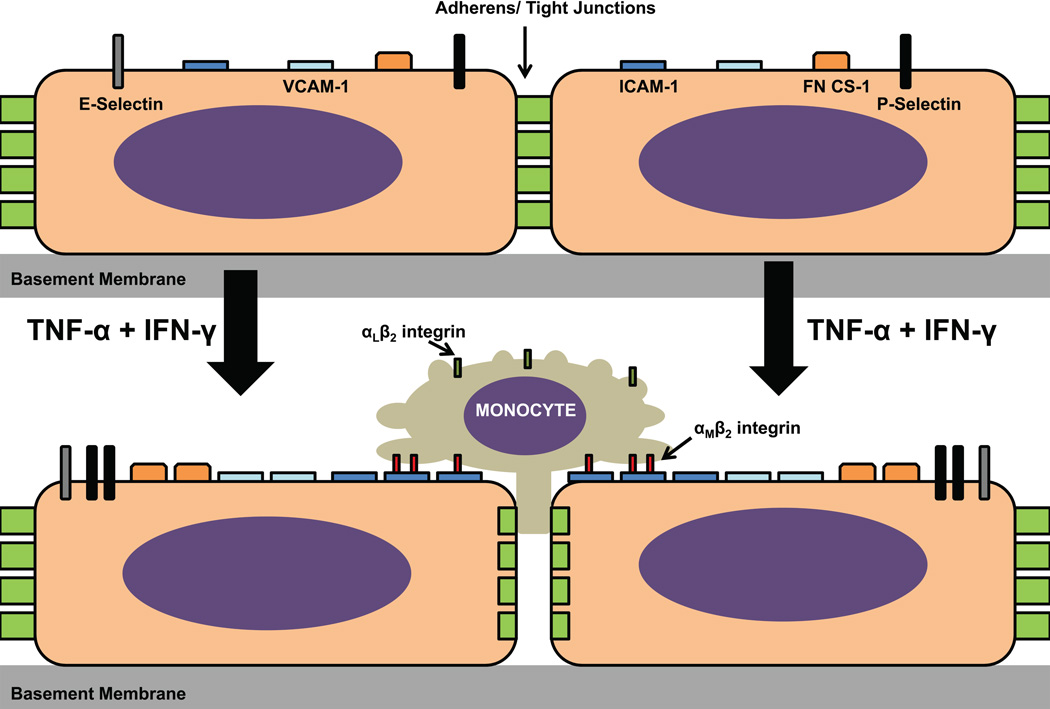
Figure 4. Hunan endoneurial endothelial cell adhesion molecules and effect of proinflammatory cytokines.
The constitutive expression of CAMs by the human BNB in vitro is depicted in the upper image, with a time-dependent increase in cytoplasmic protein expression observed following exogenous treatment of confluent cultures with 10 U/mL TNF-α and 20 U/mL IFN-γ over 48 hours. CD31 and CD34 expression have been described, but the effect of cytokine treatment on their expression has not been evaluated. Cytoplasmic JAM-A expression by pHEndECs has been described in vitro, but its expression was not regulated by proinflammatory cytokine treatment (not shown in figure). Using a flow-dependent in vitro BNB-leukocyte trafficking model, ICAM-1 significantly contributed to pathogenic peripheral blood mononuclear cell adhesion and transmigration, dependent on interactions with αMβ2 integrin, rather than its more ubiquitously expressed counterligand, αLβ2 integrin. Video microscopy shows that these mononuclear cells firmly arrest and congregate at contact sites between confluent endothelial cells, with a subset of leukocytes slowly migrating across the BNB via the paracellular route without significant retraction of neighboring endothelial cells from each other during the course of a 30-minute assay with estimated in vivo capillary flow rates based on red blood cell velocities (refer to published supplementary data for reference [61] for videos). Further studies are needed to determine whether transcellular trafficking occurs at the human BNB in vitro and in vivo, as observed in other microvascular transmigration model systems.