Abstract
Background
Patient benefits from natural orifice transluminal endoscopic surgery (NOTES) are of interest in acute-care surgery. This review provides an overview of the historical development of NOTES procedures, and addresses their current uses and limitations for intra-abdominal emergency conditions.
Methods
A PubMed search was carried out for articles describing NOTES approaches for appendicectomy, percutaneous gastrostomy, hollow viscus perforation and pancreatic necrosectomy. Pertinent articles were reviewed and data on available outcomes synthesized.
Results
Emergency conditions in surgery tax the patient’s cardiovascular and respiratory systems, and fluid and electrolyte balance. The operative intervention itself leads to an inflammatory response and blood loss, thus adding to the physiological stress. NOTES provides a minimally invasive alternative access to the peritoneal cavity, avoiding abdominal wall incisions. A clear advantage to the patient is evident with the implementation of an endoscopic approach to deal with inadvertently displaced percutaneous endoscopic gastrostomy tubes and perforated gastroduodenal ulcer. The NOTES approach appears less invasive for patients with infected pancreatic necrosis, in whom it allows surgical debridement and avoidance of open necrosectomy. Transvaginal appendicectomy is the second most frequently performed NOTES procedure after cholecystectomy. The NOTES concept has provided a change in perspective for intramural and transmural endoscopic approaches to iatrogenic perforations during endoscopy.
Conclusion
NOTES approaches have been implemented in clinical practice over the past decade. Selected techniques offer reduced invasiveness for patients with intra-abdominal emergencies, and may improve outcomes. Steady future development and adoption of NOTES are likely to follow as technology improves and surgeons become comfortable with the approaches.
Introduction
Intra-abdominal emergency conditions usually arise as a result of disruption to the blood supply (bleeding, ischaemia) or the normal gastrointestinal tract (obstruction, perforation or leak), which often leads to infection. The surgical therapy for such conditions has been emergency laparotomy with direct access to the site of interest. Emergency laparotomy is still required for acute conditions resulting in severe haemodynamic distress when there is no time for accurate diagnosis. However, when the patient’s condition allows enough time for a preoperative diagnosis, use of minimally invasive techniques to solve the problem may provide potential advantages. Emergency conditions in surgery tax the patient’s cardiovascular and respiratory systems, and fluid and electrolyte balance. The operative intervention itself leads to an inflammatory response and blood loss, thus adding to the physiological stress. In particular, a large incision in the abdominal wall contributes to the stress of a ‘second hit’.
At the juncture of endoscopy, laparoscopy and catheter-based techniques, the concept of natural orifice transluminal endoscopic surgery (NOTES) has developed. Surgeons and gastroenterologists are collaborating to advance flexible endoscopy-based techniques with the aim of further decreasing the invasiveness of intervention. The principle of the NOTES concept is the traversal of an endoscope through natural orifices (gastrointestinal tract rectally or orally, or through the vagina in women) to accomplish an intervention in the abdominal cavity.
Emergency surgical conditions, however, may often cause quite considerable patient suffering. The disease process and its treatment not infrequently have fatal consequences, especially in the frail and the immuno-compromised. The minimally invasive techniques currently applicable to emergencies due to ischaemia or bleeding and requiring more than intraluminal endoscopy are most frequently endovascular. Conditions involving disruption or infection of gastrointestinal organs are a possible target for NOTES procedures.
This review describes the current uses of NOTES for intra-abdominal surgical emergencies. Specific consideration is given to NOTES as applicable to acute appendicitis, percutaneous endoscopic gastrostomy (PEG) rescue, the treatment of peptic ulcer perforations and pancreatic necrosectomy. The limitations of NOTES are also discussed.
Methods
PubMed/MEDLINE was searched for English and German articles using the medical subject heading (MeSH) terms ‘natural orifice endoscopic surgery’, ‘appendicectomy’, ‘appendicitis’, ‘necrosectomy’, ‘acute pancreatitis’, ‘perforated ulcer’ and ‘perforated diverticulitis’. Relevant articles from clinical trials and case reports since 2005 were included as well as background articles relevant to the disease processes of interest.
Brief history of the development of NOTES
The first patient to undergo a NOTES procedure had an appendicectomy, one of the most frequently performed emergency procedures in Western countries. The endoscope was brought in through the stomach and exited the through anterior gastric wall, following which endoscopic tools were used to divide the appendiceal mesentery and ligate the base of the appendix. Anecdotally, the patient suffered from a severely scarred abdominal wall owing to burns, so transabdominal access was significantly restricted. NOTES captured the imagination of many people such that a transgastric appendicectomy was soon featured in an American television series.
It was thought that the NOTES technique would replace laparoscopy for routine procedures, which would have allowed significant additional technological development1. Given the limited patient suffering after basic laparoscopy (such as cholecystectomy), the new technique was not disruptive enough to replace laparoscopy. However, modifications of the laparoscopic technique have been investigated. Single-port laparoscopy and minilaparoscopy have been further developed for common procedures as a consequence of NOTES. In addition, intraluminal procedures have evolved with use of endoscopic suturing tools and large clips.
NOTES appendicectomy
Acute appendicitis is the most common abdominal emergency. The advent of minimally invasive technology has radically transformed the landscape of surgical management of appendicitis. Over the past decade, appendicectomy has gone from an open to a minimally invasive approach, most often three-port laparoscopy. Despite the universal acceptance of the minimally invasive approach, the ideal technique is still heavily debated and undergoing modifications, including single-port appendicectomy and NOTES. The first incidental transvaginal appendicectomy was reported in 1949 by Bueno2, and the first pure transvaginal NOTES appendicectomy in 2008 by Palanivelu and colleagues3. Appendicectomy is currently the second most frequently performed NOTES procedure after cholecystectomy. In contrast to other NOTES procedures for emergency conditions, appendicectomy can be performed through a variety of natural orifices.
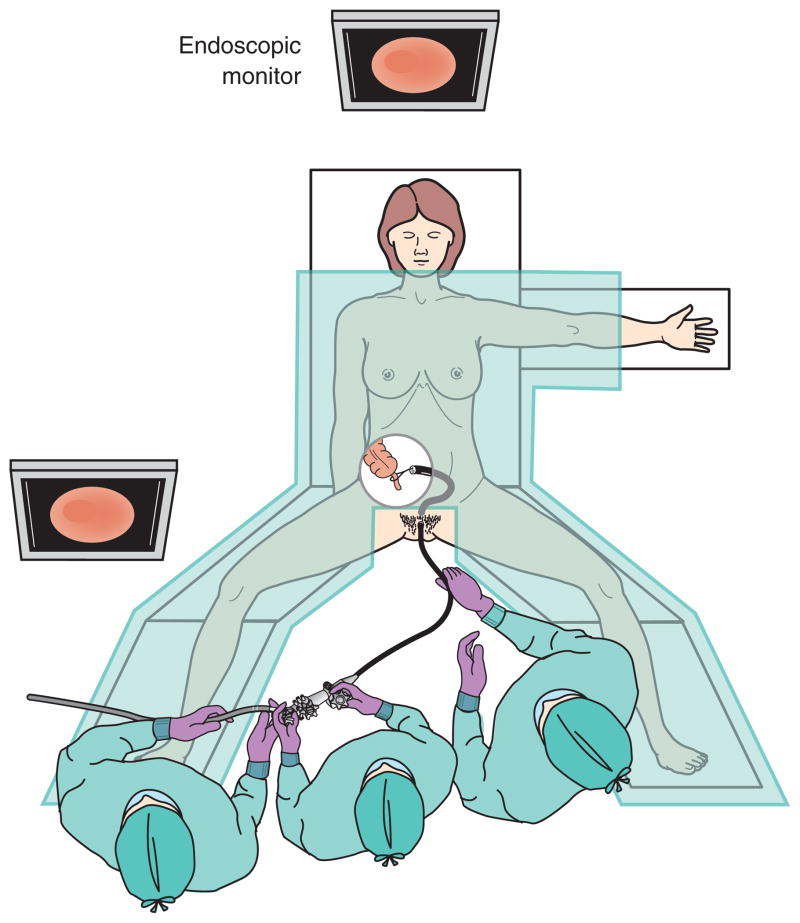
The choice of orifice and the procedure performed varies from patient to patient, and is at the discretion of the surgeon. To date, several successful endoscopic approaches have been developed for appendicectomy, including the transgastric, transcolonic, transvaginal and transvesical routes4 – 7. Any of the approaches can be performed as a pure NOTES procedure without any percutaneous assistance, or as hybrid NOTES with addition of laparoscopy. Hybrid NOTES utilizes laparoscopic visualization or an assistance port. NOTES procedures (especially transvaginal or transrectal procedures) are further divided to FLEX-notes, performed by flexible endoscopy, or RIG-NOTES, assisted by rigid instruments. A purely transvaginal NOTES procedure can be carried out by the same number of team members as a traditional laparoscopic or open appendicectomy (Fig. 1). If a hybrid procedure is performed, an additional assistant is needed for the second operative field.
Fig. 1.
Set up for transvaginal appendectomy using flexible endoscopic instrumentation
The following aspects often determine the route for NOTES appendicectomy: access and secure closure of the transluminal site, risk of infectious complications, and ease of specimen extraction through the entry site. The transvaginal approach offers the advantages of a well known entry site into the peritoneum through a posterior colpotomy, and the use of traditional laparoscopic equipment and rigid instruments. In contrast to transvaginal appendicectomy, transgastric and transcolonic approaches require application of more flexible and longer instruments. As NOTES is still evolving, proper instrumentation still represents a challenge that affects the efficiency and length of operation. The transvaginal route provides direct access for closure of the vaginal stump using conventional instruments under direct vision. It also allows retrieval of large specimens, which can present a significant challenge through the transgastric route. However, the transgastric approach provides better control of the bacterial load than the other routes, although closure of the gastrotomy may be challenging. Over-the-scope clip closure is relatively reliable, although the need for further laparoscopic suturing has been reported8. Overall, the transgastric approach requires a longer learning curve owing to the need for more complicated flexible endoscopy skills, and the technical difficulties associated with instrument advancement and specimen retrieval through the narrow lumen of the oesophagus. Despite the ease of access with the trans-vaginal route, a hostile pelvis owing to previous infections and surgical interventions is more common than a hostile upper abdomen. A study in the UK and Germany that compared the transgastric with the trans-sigmoidal technique for appendicectomy in the ELITE simulator (endoscopic–laparoscopic interdisciplinary training entity, based on the synthetic training manikin ELITE; CLA, Coburg, Germany)9 found that surgeons had better control of the instrumentation in the trans-sigmoidal procedure. There was no difference in mean performance time between the two approaches. It has been reported that use of the incisionless Operating Platform™ (USGI Medical, San Clemente, California, USA), a multifunctional and flexible surgical platform, improves accessibility and manoeuvrability during NOTES procedures, although it requires a longer learning curve10,11; surgeons successfully completed a small series of transgastric appendicectomies without the need for conversion. The transcolonic approach offers advantages over the transgastric approach in terms of closure using the transanal endoscopic micro-surgery technique. It serves as a safe alternative to the transvaginal approach for male patients.
Sexual function after transvaginal appendicectomy
A study of 42 patients who underwent either laparoscopic or transvaginal appendicectomy showed no effect of transvaginal access on sexual function scores at approximately 3 months after the procedure12. There were no changes in sexual function (compared with preoperative baseline) reported after either transvaginal or laparoscopic appendicectomy13. No complaints of dyspareunia were reported in a case series of ten women who underwent a transvaginal NOTES procedure, two of whom had a transvaginal appendicectomy14. Unfortunately, the Euro-NOTES clinical registry for natural orifice transluminal endoscopic surgery, one of the biggest on NOTES appendicectomies, has no information on dyspareunia. Nevertheless, these conclusions are in line with previous findings reported by gynaecologists on the outcomes of hysterectomy performed transvaginally. Although there is no long-term effect on sexual function, sexual abstinence for 2–6 weeks is currently recommended after a transvaginal procedure. It is too early to make definite conclusions regarding sexual function after transvaginal appendicectomy. Larger and longer-term studies are needed to provide more solid evidence concerning not only the sexual sequelae but also the mandatory period of abstinence following the transvaginal approach.
Infectious complications, accessibility and conversion rate
Complications of NOTES appendicectomy vary between different approaches. The rate of intraoperative complications ranges from 0 to 6·1 per cent. Zorron and colleagues15 reported intraoperative bleeding from the appendiceal vessels in four of 51 patients; this was controlled by laparoscopic clips. The overall postoperative complication rate ranges from 0 to 11·9 per cent, with a higher incidence after transvaginal appendicectomy. In one study14 no postoperative complications were observed over a median follow-up of 10·6 months. The most common complications reported after a transvaginal procedure are intra-abdominal abscess and urinary retention12,13,16. Urinary tract infections, postoperative prolonged ileus, wound infection and vaginal cuff granulation have also been documented16. These complications were also described as the most common after both single-incision and conventional three-incision laparoscopic appendicectomy17.
NOTES for gastrostomy tube replacement
One of the first emergency NOTES procedures described in the USA was the replacement of a PEG tube that had been removed inadvertently soon after placement18. Traditionally, this was dealt with by emergency laparotomy or laparoscopy to irrigate the abdomen, close the gastrostomy and place a new tube. In this instance, the NOTES procedure was performed in a sedated patient in the intensive care unit. The endoscope exited the anterior gastric wall at the existing gastrotomy site. The peritoneal cavity was surveyed and free fluid aspirated. A wire was placed through the abdominal wall, retrieved from the peritoneal cavity and withdrawn back into the stomach. The bumper tube was replaced inside the lumen, and the patient was spared general anaesthesia and laparoscopy18. Others19 have used similar approaches, showing a clear advantage to the patient.
NOTES for perforated gastroduodenal ulcer
A recent study20 found the mean age of patients with perforated ulcer to be 68 years, and the mean American Society of Anesthesiologists grade to be III, representing a population with limited physiological reserve21. A nationwide Danish prospective cohort study22 in 2003–2009 reported a mortality rate as high as 26·5 per cent after perforated peptic ulcer.
Complications after open operative intervention for perforated peptic ulcer contribute to mortality23. A recent systematic review24 suggested that the laparoscopic approach may be beneficial; however, there have not been enough randomized trials to determine whether the difference is significant. Furthermore, laparoscopic suturing is an advanced technical skill and may not always be available when caring for a patient with peptic ulcer perforation20. Thus, a different minimally invasive technique may help decrease the ‘second hit’.
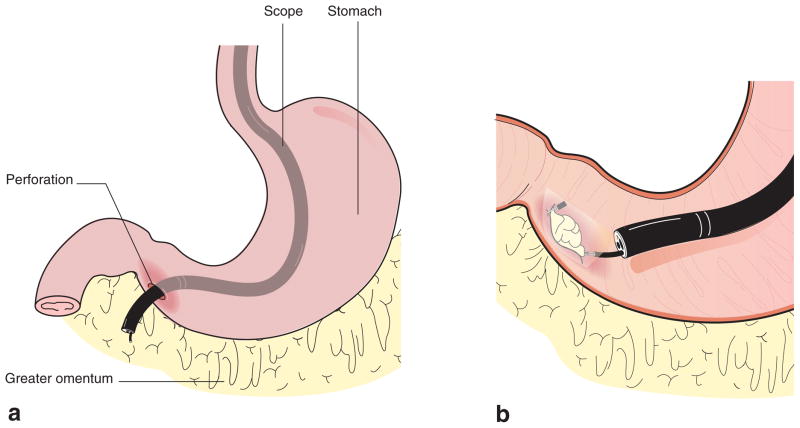
Ulcer closure by NOTES uses the same concept as open and laparoscopic surgery: to bring a well vascularized pedicle of omentum or falciform ligament to the perforation site and fasten it in place (Fig. 2). Using carbon dioxide insufflation, the endoscope exits the existing perforation site, the abdominal cavity is irrigated and the omentum is pulled inside the stomach or duodenal lumen. It is then clipped in place and a leak test can be performed by insufflating the lumen25. In a retrospective review20 of 100 operative reports, the procedure was deemed possible in about 50 per cent. The technique was developed and studied extensively in an animal model25,26, and a pilot trial27 was performed in humans to demonstrate feasibility. Haemodynamically stable patients with a suspected perforated ulcer were potentially eligible for a NOTES procedure. Patients who had undergone previous omentectomy or upper gastrointestinal surgery that had altered the anatomy, or were found to have giant perforated ulcers, were excluded. Resuscitation proceeded in a standard fashion with intravenous fluid and antibiotics, to avoid delaying the operative procedure. Trial procedures were performed under laparoscopic guidance to assure patient safety (Fig. 3). If the ulcer itself was too small to permit exit of the entire endoscope, laparoscopic assistance was used. A surgeon or gastroenterologist used the endoscope with a technical assistant, and one surgeon used the laparoscope with an assistant. A contrast swallow was performed to exclude any leak before resumption of oral intake. The postoperative hospital stay was 3–4 days. Patients who were offered the new procedure were amenable to having a different approach, unlike those who were offered a transvaginal cholecystectomy28. It is estimated that the endoscopic skill required to perform the procedure is similar to that for PEG placement or for application of a haemostatic endoscopic clip to control gastric haemorrhage. The NOTES approach demonstrated that an oesophagogastroduodenoscopy is not necessarily absolutely contraindicated in a patient with presumed ulcer perforation. The oesophagogastroduodenoscopy added additional diagnostic information in some patients (kissing ulcer, invasion of large perforation into pancreas, diagnosis of perforation site in a patient with cirrhosis undergoing primary open ulcer repair). Teaching courses have been offered at national meetings to facilitate diffusion.
Fig. 2.
Schematic of transluminal omental patch repair for perforated ulcer. a Peritoneal access through the perforation site; b transluminal omental patch for perforated ulcer
Fig. 3.
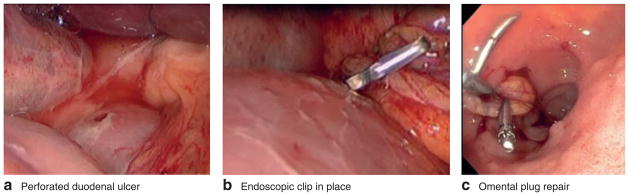
Perforated ulcer repair. a Laparoscopic view of perforated duodenal ulcer, b laparoscopic view of endoscopic clip grasping falciform ligament pedicle and c endoscopic view of omental plug after clipping and leak testing
NOTES for pancreatic necrosectomy
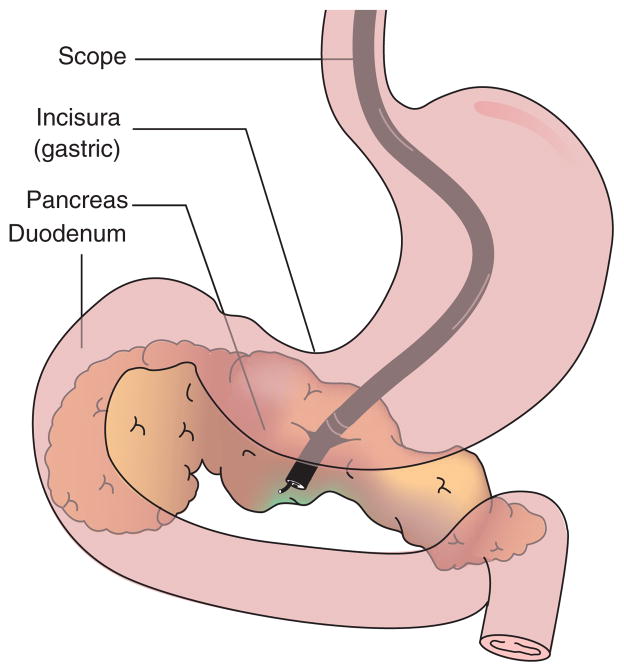
Until recently, open surgical intervention was the standard procedure for infected pancreatic necrosis29,30. Endoscopic drainage of symptomatic and infected pseudocysts slowly replaced some surgical interventions, starting in 198331. Infected necrosis was initially addressed endoscopically in 2000 and gained more momentum as a NOTES concept. When endoscopic ultrasonography became available, ‘seeing beyond the lumen’ and understanding the vascular anatomy became possible. In laboratory studies an exit just proximal to the incisura was found to be most helpful for gaining access to the pancreas (Fig. 4)32. Several teams33,34 have now embarked on removing infected necrotic tissue from the lesser sac by endoscopic means.
Fig. 4.
Transgastric access to pancreatic necrosis
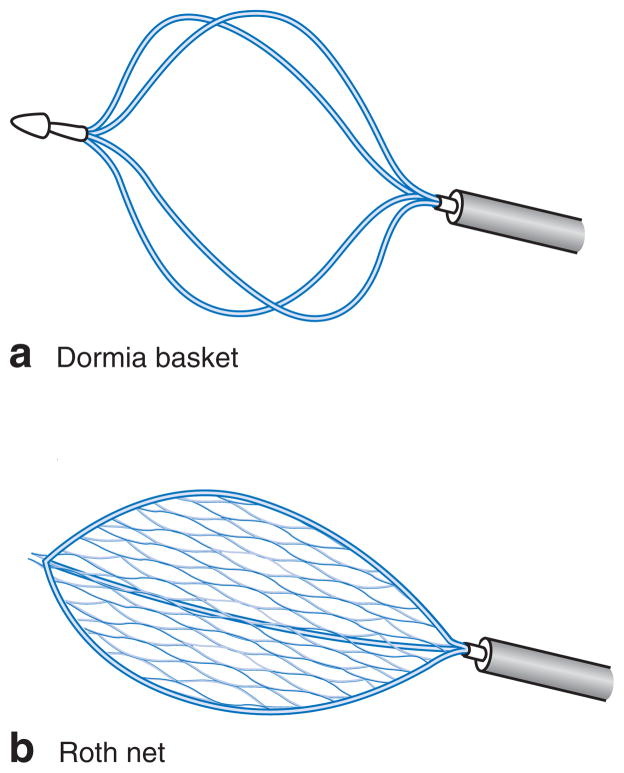
Traditionally, a well formed pseudocyst was drained using a cyst wall puncture and a small-lumen stent placed to drain the fluid. Any necrotic tissue stayed in place and continued to be a source of sepsis. Now endoscopists consider intervention when an infected necrosis becomes life-threatening. A large gastrotomy (more than 1 cm) is created in the posterior wall of the stomach to allow access to the lesser sac. Initially the posterior wall is opened with a needle knife, followed by a sphincterotome or balloon. A larger-bore metallic stent can be placed to maintain patency of the gastrotomy for repeated access and irrigation. The large gastrotomy allows entry of the endoscope into the lesser sac to visualize the necrosis. Under direct vision, the endoscopist can debride the tissue, with the aid of one technical assistant, while sedation or anaesthesia is monitored by a dedicated provider. Irrigation, Dormia baskets, Roth nets and biopsy forceps have been used (Fig. 5)33.
Fig. 5.
a Dormia basket and b Roth net
Even though endoscopic debridement is a slow process, it closely mirrors surgical debridement while maintaining an intact abdominal wall in a patient without compartment syndrome. After completion of the initial debridement, transnasal drainage catheters can be brought in to permit irrigation. To access dependent portions of large necrotic cavities, a rendezvous procedure under image guidance can also be performed. As with open or laparoscopic surgical debridement, repeated procedures are necessary. Bleeding is a major risk during any debridement of infected pancreatic necrosis. The advantage of transluminal access into the lesser sac compared with a drainage-only procedure is the extent of debridement possible under vision, and the ability to visualize blood vessels and friable tissue to prevent injury.
The recent PENGUIN trial34 of endoscopic versus surgical necrosectomy for infected pancreatitis suggested that the main benefit of the endoscopic approach is that it is less invasive. A criticism of the study has been the high mortality rate in the open necrosectomy group, which may have led to bias towards the endoscopic group.
NOTES for iatrogenic perforations and postoperative leaks
Iatrogenic perforations during colonoscopy and oesophagogastroduodenoscopy are rare (1 in 1000 to 1 in 4000 procedures). Over a 25-year period at a tertiary referral centre, 180 iatrogenic colonic perforations were treated (incidence 0·07 per cent), 165 by an emergency laparotomy35. Eighty per cent presented within 24 h and had minimal peritoneal contamination.
As a consequence of NOTES techniques, pneumoperitoneum alone found at endoscopic intervention is no longer a reason to proceed expeditiously to the operating theatre for exploration. Endoscopists have become more comfortable with ‘venting’ an abdominal cavity using a Veress needle or angiocatheter. Endoscopic clips and suturing techniques allow a first attempt at endoscopic repair, certainly if the perforation is visualized immediately. As a result, the same centre has now instituted a pathway calling first for an endoscopic attempt at closure, followed by surgical consultation for laparoscopic closure if this is unsuccessful.
A similar situation applies to the stenting of anastomotic leaks (for example after oesophageal or low anterior colorectal resections). Although the primary approach to stenting is endoluminal, at times extraluminal debridement is possible. NOTES has provided a change in perspective for all intramural and transmural endoscopic approaches, following the demonstration that it is feasible, haemodynamically safe with appropriate precautions, and with no higher risk of infection than with gastrointestinal surgery alone.
NOTES for perforated diverticulitis
Another frequent source of perforation, inflammation and infection is diverticular disease. NOTES procedures have had no impact in this situation up to now. Endoscopic closure of intestinal perforation in the upper gastrointestinal tract is more feasible than such closure of colonic perforation sites. Experimental data on colonic closure by means of clips or suturing are not yet convincing. In addition, a severely distorted colonic lumen during the acute inflammatory phase of diverticulitis increases the procedural difficulty and risk.
Discussion
Pure and hybrid NOTES approaches have been developed and brought into clinical use over the past decade. NOTES has not replaced traditional basic laparoscopy. For patients with conditions requiring urgent intervention, such as ulcer perforation and infected pancreatic necrosis, the value of NOTES is emerging. This is especially true for procedures with high mortality and procedure-related morbidity rates. As a consequence of the research into NOTES, it has been possible to allay concerns about endoscopic examinations being contraindicated in the setting of a perforation.
With the advent of a new technique, the operating time is frequently longer than that for the standard approach. The time taken for successful repair of ulcer perforations by a NOTES approach is similar to historical data for open or laparoscopic omental patch closure27. Procedure duration is easiest to compare for NOTES appendicectomy as a number of studies have reported duration of operation for traditional laparoscopy, single-port laparoscopy, and the transvaginal and transgastric approach to NOTES appendicectomy. The only case–control study12,13 to compare directly conventional laparoscopic three-port with pure transvaginal appendicectomy reported similar operating times (mean(s.d.) 44·4(4·5) versus 39·8(2·6) min). In a study8 based on data from the European registry supported by the Euro-NOTES Foundation, reporting 28 hybrid transgastric and five hybrid transvaginal appendicectomies using either a flexible endoscope or rigid laparoscope, the mean duration of surgery was significantly shorter in the transvaginal group (59 versus 99·8 min; P = 0·002). An international multicentre trial15 among nine countries reported 37 transvaginal and 14 transgastric appendicectomies over 3 years (2007–2009); again, the mean(s.d.) operating time was shorter for transvaginal than for transgastric appendicectomy (60·5(31·3) versus 135·5(9·3) min). In general, the operating times for transvaginal techniques are comparable with those reported in a meta-analysis of single-incision and conventional laparoscopic appendicectomy36. The transgastric approach takes longer than conventional and single-incision procedures. It has been demonstrated in some studies8,9 that previous experience of the operating surgeon with single-incision laparoscopic surgery helps achieve a rapid learning curve for NOTES.
Introducing a new technique in the clinical environment can be difficult, and conversion to a traditional procedure may be necessary. In an initial experience of three transgastric appendicectomies, only one was successful, with conversion in the other two37 (Table 1). The Euro-NOTES registry43 reported a conversion rate of 7 per cent, similar to that in earlier series of conventional laparoscopic appendicectomies. Conversion was prompted by injuries to the caecal serosa owing to difficulties with tissue manipulation by the transgastric route8. The issue was overcome by using additional transabdominal trocars in transvaginal appendicectomy procedures, obviating the need for conversion. It may be possible to decrease the conversion rate in transvaginal appendicectomy by using commercially available single-incision ports through the colpotomy.
Table 1.
Characteristics of all currently available studies on natural orifice transluminal endoscopic appendicectomy
| Reference | Year | Approach | No. of patients | NOTES procedure | Conversion |
|---|---|---|---|---|---|
| Tsin et al.38 | 2007 | Transvaginal | 3 | Laparoscopically assisted | 0 |
| Palanivelu et al.3 | 2008 | Transvaginal | 1 | Hybrid | 0 |
| Bernhardt et al.39 | 2008 | Transvaginal | 1 | Pure | 0 |
| Rao et al.5 | 2008 | Transgastric | 8 | Pure | 0 |
| Tabutsadze and Kipshidze40 | 2009 | Transvaginal | 2 | Pure | 0 |
| Park and Bergstrom37 | 2010 | Transgastric | 3 | Hybrid | 2 of 3 |
| Shin et al.41 | 2010 | Transvaginal | 1 | Hybrid | 0 |
| Noguera et al.14 | 2011 | Transvaginal | 4 | Hybrid | 0 |
| Horgan et al.10 | 2011 | Transgastric | 2 | Pure | 0 |
| Roberts et al.13 | 2012 | Transvaginal | 18 | Pure | 1 of 18 |
| Panait et al.42 | 2013 | Transvaginal | 1 | Pure | 0 |
| Kaehler et al.7 | 2013 | Transgastric | 15 | Hybrid | 1 of 15 |
NOTES, natural orifice transluminal endoscopic surgery.
Although a postoperative stay ranging from 1 to 4 days has been reported after NOTES appendicectomy, similar to that for conventional and single-incision laparoscopic approaches36, a relatively longer hospital stay after NOTES appendicectomy has commonly been described by surgeons as a precautionary measure owing to the novelty of the technique.
The aim of NOTES is for the procedure to be less invasive by avoiding the abdominal wall. The invasiveness of the procedure can be measured in terms of pain and return to regular activities. Roberts and colleagues13, using a purely transvaginal access in 18 patients, showed that those who underwent transvaginal appendicectomy required less pain medication in the first 12 h than patients who had a laparoscopic three-port appendicectomy (mean(s.d.) morphine administered using patient-controlled analgesia: 8·7(2·1) versus 23·0(3·4) mg). It also allowed more rapid return to normal activity (6·4 days) and return to work (5·3 days). Almost one-quarter of patients in the international registry (12 of 51) had no requirement for any analgesia in the postoperative period15. These data indicate that avoiding the abdominal wall as entry site to the peritoneal cavity can indeed translate into direct patient benefit. Knowledge of this potential benefit, however, is not represented uniformly in public opinion and patients’ preferences. In a study of patient preferences44, younger patients (aged 20–29 years) were more willing to try the newer technique than those aged 50–59 years, and women were more likely to do so than men (24 versus 16 per cent). However, none of the patients offered the new approach for emergency ulcer repair or pancreatic necrosectomy declined.
Intra-abdominal emergency conditions and the procedures necessary to alleviate them continue to cause significant suffering. As the population of elderly patients increases, minimally invasive techniques will be necessary to improve outcomes for those with decreased physiological reserve. Surgeons and endoscopists are slowly becoming familiar with the endoscopic view of the extramural environment, and the availability and acceptance of data on the safety of NOTES is increasing. Endoscopic, laparoscopic and robotic technology continues to develop, for both visualization (such as narrow band imaging and autofluorescence, confocal microscopy, computed tomography-based augmented reality45) and instrumentation (single-port robotics, improved suction and instrumentation channels in endoscopes, cautery-enabled endoscopic scissors). Thus, steady progress is being made towards minimally invasive procedures for emergency conditions. Collaboration between different physician teams and openness to new technology in adjacent areas of practice are needed for continued improvement in patient care.
Supplementary Material
Acknowledgments
Research reported in this article was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (award no. K23DK93553-01A1). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Rattner D, Kalloo A ASGE/SAGES Working Group. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery October 2005. Surg Endosc. 2006;20:329–333. doi: 10.1007/s00464-005-3006-0. [DOI] [PubMed] [Google Scholar]
- 2.Bueno B. Primer caso de apendicectomia por via vaginal. Tokoginecol Pract. 1949;8:152–158. [PubMed] [Google Scholar]
- 3.Palanivelu C, Rajan PS, Rangarajan M, Parthasarathi R, Senthilnathan P, Prasad M. Transvaginal endoscopic appendectomy in humans: a unique approach to NOTES – world’s first report. Surg Endosc. 2008;22:1343–1347. doi: 10.1007/s00464-008-9811-5. [DOI] [PubMed] [Google Scholar]
- 4.Horgan S, Cullen JP, Talamini MA, Mintz Y, Ferreres A, Jacobsen GR, et al. P.Natural orifice surgery: initial clinical experience. Surg Endosc. 2009;23:1512–1518. doi: 10.1007/s00464-009-0428-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rao GV, Reddy DN, Banerjee R. NOTES: human experience. Gastrointest Endosc Clin N Am. 2008;18:361–370. doi: 10.1016/j.giec.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Jeong CW, Lee S, Oh JJ, Lee SB, Jeong SJ, Hong SK, et al. Pure transvesical NOTES appendectomy using a 5-mm rigid laparoscope: a feasibility and survival study with porcine models. Surg Endosc. 2013;27:2992–2999. doi: 10.1007/s00464-013-2825-7. [DOI] [PubMed] [Google Scholar]
- 7.Kaehler G, Schoenberg MB, Kienle P, Post S, Magdeburg R. Transgastric appendicectomy. Br J Surg. 2013;100:911–915. doi: 10.1002/bjs.9115. [DOI] [PubMed] [Google Scholar]
- 8.Arezzo A, Zornig C, Mofid H, Fuchs KH, Breithaupt W, Noguera J, et al. The EURO-NOTES clinical registry for natural orifice transluminal endoscopic surgery: a 2-year activity report. Surg Endosc. 2013;27:3073–3084. doi: 10.1007/s00464-013-2908-5. [DOI] [PubMed] [Google Scholar]
- 9.Clark J, Gillen S, James DR, Fiolka A, Karimyan V, Sodergren M, et al. Transgastric or trans-sigmoidal? The impact of the choice of access on task performance in target natural orifice translumenal endoscopic surgery procedures. J Laparoendosc Adv Surg Tech A. 2011;21:237–242. doi: 10.1089/lap.2010.0360. [DOI] [PubMed] [Google Scholar]
- 10.Horgan S, Thompson K, Talamini M, Ferreres A, Jacobsen G, Spaun G, et al. Clinical experience with a multifunctional, flexible surgery system for endolumenal, single-port, and NOTES procedures. Surg Endosc. 2011;25:586–592. doi: 10.1007/s00464-010-1225-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaikh SN, Thompson CC. Natural orifice translumenal surgery: flexible platform review. World J Gastrointest Surg. 2010;2:210–216. doi: 10.4240/wjgs.v2.i6.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roberts KE, Silasi DA, Bell RL, Duffy AJ. Pure transvaginal laparoscopic appendectomy. Surg Endosc. 2012;26:3316. doi: 10.1007/s00464-012-2319-z. [DOI] [PubMed] [Google Scholar]
- 13.Roberts KE, Solomon D, Mirensky T, Silasi DA, Duffy AJ, Rutherford T, et al. Pure transvaginal appendectomy versus traditional laparoscopic appendectomy for acute appendicitis: a prospective cohort study. Ann Surg. 2012;255:266–269. doi: 10.1097/SLA.0b013e31823b2748. [DOI] [PubMed] [Google Scholar]
- 14.Noguera JF, Cuadrado A, Sánchez-Margallo FM, Dolz C, Asencio JM, Olea JM, et al. Emergency transvaginal hybrid natural orifice transluminal endoscopic surgery. Endoscopy. 2011;43:442–444. doi: 10.1055/s-0030-1256042. [DOI] [PubMed] [Google Scholar]
- 15.Zorron R, Palanivelu C, Galvão Neto MP, Ramos A, Salinas G, Burghardt J, et al. International multicenter trial on clinical natural orifice surgery – NOTES IMTN study: preliminary results of 362 patients. Surg Innov. 2010;17:142–158. doi: 10.1177/1553350610370968. [DOI] [PubMed] [Google Scholar]
- 16.Wood SG, Panait L, Duffy AJ, Bell RL, Roberts KE. Complications of transvaginal natural orifice transluminal endoscopic surgery: a series of 102 patients. Ann Surg. 2013 doi: 10.1097/SLA.0b013e3182916138. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 17.Ahmed K, Wang TT, Patel VM, Nagpal K, Clark J, Ali M, et al. The role of single-incision laparoscopic surgery in abdominal and pelvic surgery: a systematic review. Surg Endosc. 2011;25:378–396. doi: 10.1007/s00464-010-1208-6. [DOI] [PubMed] [Google Scholar]
- 18.Marks JM, Ponsky JL, Pearl JP, McGee MF. PEG ‘rescue’: a practical NOTES technique. Surg Endosc. 2007;21:816–819. doi: 10.1007/s00464-007-9361-2. [DOI] [PubMed] [Google Scholar]
- 19.Sweetser S, Kashyap P, Baron TH. Percutaneous endoscopic gastrostomy tract salvage using natural orifice transluminal endoscopic surgery technique (with video) Gastrointest Endosc. 2011;73:839–840. doi: 10.1016/j.gie.2010.08.044. [DOI] [PubMed] [Google Scholar]
- 20.Bonin EA, Moran E, Gostout CJ, McConico AL, Zielinski M, Bingener J. Natural orifice transluminal endoscopic surgery for patients with perforated peptic ulcer. Surg Endosc. 2012;26:1534–1538. doi: 10.1007/s00464-011-2063-9. [DOI] [PubMed] [Google Scholar]
- 21.Thorsen K, Søreide JA, Kvaløy JT, Glomsaker T, Søreide K. Epidemiology of perforated peptic ulcer: age- and gender-adjusted analysis of incidence and mortality. World J Gastroenterol. 2013;19:347–354. doi: 10.3748/wjg.v19.i3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buck DL, Vester-Andersen M, Moller MH. Surgical delay is a critical determinant of survival in perforated peptic ulcer. Br J Surg. 2013;100:1045–1049. doi: 10.1002/bjs.9175. [DOI] [PubMed] [Google Scholar]
- 23.Imhof M, Epstein S, Ohmann C, Röher HD. Duration of survival after peptic ulcer perforation. World J Surg. 2008;32:408–412. doi: 10.1007/s00268-007-9370-2. [DOI] [PubMed] [Google Scholar]
- 24.Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev. 2013;(2):CD004778. doi: 10.1002/14651858.CD004778.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moran EA, Gostout CJ, McConico AL, Bingener J. Natural orifice translumenal endoscopic surgery used for perforated viscus repair is feasible using lower peritoneal pressures than laparoscopy in a porcine model. J Am Coll Surg. 2010;210:474–479. doi: 10.1016/j.jamcollsurg.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Moran EA, Gostout CJ, McConico AL, Michalek J, Huebner M, Bingener J. Assessing the invasiveness of NOTES perforated viscus repair: a comparative study of NOTES and laparoscopy. Surg Endosc. 2012;26:103–109. doi: 10.1007/s00464-011-1834-7. [DOI] [PubMed] [Google Scholar]
- 27.Bingener J, Loomis EA, Gostout CJ, Zielinski MD, Buttar NS, Song LM, et al. Feasibility of NOTES omental plug repair of perforated peptic ulcers: results from a clinical pilot trial. Surg Endosc. 2013;27:2201– 2208. doi: 10.1007/s00464-012-2740-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bingener J, Sloan JA, Ghosh K, McConico A, Mariani A. Qualitative and quantitative analysis of women’s perceptions of transvaginal surgery. Surg Endosc. 2012;26:998–1004. doi: 10.1007/s00464-011-1984-7. [DOI] [PubMed] [Google Scholar]
- 29.Vasiliadis K, Papavasiliou C, Al Nimer A, Lamprou N, Makridis C. The role of open necrosectomy in the current management of acute necrotizing pancreatitis: a review article. ISRN Surg. 2013;2013:579435. doi: 10.1155/2013/579435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cirocchi R, Trastulli S, Desiderio J, Boselli C, Parisi A, Noya G, et al. Minimally invasive necrosectomy versus conventional surgery in the treatment of infected pancreatic necrosis: a systematic review and a meta-analysis of comparative studies. Surg Laparosc Endosc Percutan Tech. 2013;23:8–20. doi: 10.1097/SLE.0b013e3182754bca. [DOI] [PubMed] [Google Scholar]
- 31.Baron TH, Kozarek RA. Endotherapy for organized pancreatic necrosis: perspectives after 20 years. Clin Gastroenterol Hepatol. 2012;10:1202–1207. doi: 10.1016/j.cgh.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 32.Moran EA, Bingener J, Murad F, Levy MJ, Gostout CJ. The challenges with NOTES retroperitoneal access in humans. Surg Endosc. 2011;25:1096–1100. doi: 10.1007/s00464-010-1323-4. [DOI] [PubMed] [Google Scholar]
- 33.Gardner TB, Chahal P, Papachristou GI, Vege SS, Petersen BT, Gostout CJ, et al. A comparison of direct endoscopic necrosectomy with transmural endoscopic drainage for the treatment of walled-off pancreatic necrosis. Gastrointest Endosc. 2009;69:1085–1094. doi: 10.1016/j.gie.2008.06.061. [DOI] [PubMed] [Google Scholar]
- 34.Bakker OJ, van Santvoort HC, van Brunschot S, Geskus RB, Besselink MG, Bollen TL, et al. Dutch Pancreatitis Study Group. Endoscopic transgastric vs surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA. 2012;307:1053–1061. doi: 10.1001/jama.2012.276. [DOI] [PubMed] [Google Scholar]
- 35.Iqbal CW, Cullinane DC, Schiller HJ, Sawyer MD, Zietlow SP, Farley DR. Surgical management and outcomes of 165 colonoscopic perforations from a single institution. Arch Surg. 2008;143:701–706. doi: 10.1001/archsurg.143.7.701. [DOI] [PubMed] [Google Scholar]
- 36.Gill RS, Shi X, Al-Adra DP, Birch DW, Karmali S. Single-incision appendectomy is comparable to conventional laparoscopic appendectomy: a systematic review and pooled analysis. Surg Laparosc Endosc Percutan Tech. 2012;22:319–327. doi: 10.1097/SLE.0b013e31824f2cf8. [DOI] [PubMed] [Google Scholar]
- 37.Park PO, Bergstrom M. Transgastric peritoneoscopy and appendectomy: thoughts on our first experience in humans. Endoscopy. 2010;42:81–84. doi: 10.1055/s-0029-1243795. [DOI] [PubMed] [Google Scholar]
- 38.Tsin DA, Colombero LT, Lambeck J, Manolas P. Minilaparoscopy-assisted natural orifice surgery. JSLS. 2007;11:24–29. [PMC free article] [PubMed] [Google Scholar]
- 39.Bernhardt J, Gerber B, Schober HC, Kähler G, Ludwig K. NOTES – case report of a unidirectional flexible appendectomy. Int J Colorectal Dis. 2008;23:547–550. doi: 10.1007/s00384-007-0427-3. [DOI] [PubMed] [Google Scholar]
- 40.Tabutsadze T, Kipshidze N. New trend in endoscopic surgery: transvaginal appendectomy NOTES (Natural Orifice Transluminal Endoscopic Surgery) Georgian Med News. 2009;(168):7–10. [PubMed] [Google Scholar]
- 41.Shin EJ, Jeong GA, Jung JC, Cho GS, Lim CW, Kim HC, et al. Transvaginal endoscopic appendectomy. J Korean Soc Coloproctol. 2010;26:429–432. doi: 10.3393/jksc.2010.26.6.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Panait L, Wood SG, Bell RL, Duffy AJ, Roberts KE. Transvaginal natural orifice transluminal endoscopic surgery in the morbidly obese. Surg Endosc. 2013;27:2625–2629. doi: 10.1007/s00464-012-2775-5. [DOI] [PubMed] [Google Scholar]
- 43.Li X, Zhang J, Sang L, Zhang W, Chu Z, Liu Y. Laparoscopic versus conventional appendectomy – a meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010;10:129. doi: 10.1186/1471-230X-10-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chow A, Purkayastha S, Dosanjh D, Sarvanandan R, Ahmed I, Paraskeva P. Patient reported outcomes and their importance in the development of novel surgical techniques. Surg Innov. 2012;19:327–334. doi: 10.1177/1553350611426011. [DOI] [PubMed] [Google Scholar]
- 45.Azagury DE, Ryou M, Shaikh SN, San José Estépar R, Lengyel BI, Jagadeesan J, et al. Real-time computed tomography-based augmented reality for natural orifice transluminal endoscopic surgery navigation. Br J Surg. 2012;99:1246–1253. doi: 10.1002/bjs.8838. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.