Abstract
Purpose
This research aimed to explain sexual orientation disparities in BMI by examining child abuse history, weight-related behaviors, and sociodemographics.
Methods
We used data from 7960 females and 5992 males from the prospective Growing Up Today Study over nine waves between 1996 (ages 12–14 years) and 2007 (ages 20–25 years). Using repeated measures of BMI (kg/m2) as a continuous outcome, gender-stratified latent quadratic growth models adjusted for child abuse history, weight-related behaviors, and sociodemographics. BMI at age 17 years (intercept) and one-year change in BMI (slope) are reported.
Results
Bisexual females had higher BMI at age 17 years (β = 1.59, 95% CI = 1.00, 2.18) and displayed greater one-year increases in BMI (β = .09, 95% CI = .03, .14), compared to completely heterosexual females. Gay males displayed smaller one-year increases in BMI (β = − .19, 95% CI = −.25, −.12), compared to completely heterosexual males. No sexual orientation differences in BMI at age 17 years were observed for males, but gay males’ BMI at age 25 was less than completely heterosexual males by 2 units. Among females, sexual orientation differences remained but were slightly attenuated after controlling for child abuse history, weight-related behaviors, and sociodemographics. Among males, the addition of child abuse and weight-related behaviors did not change the estimated difference in one-year BMI increases.
Conclusions
Sexual orientation differences in BMI were partly explained by child abuse and weight-related behaviors in females. More research is needed to explore additional drivers of these disparities among both females and males.
Keywords: obesity, child abuse, adolescence, gender differences, sexual orientation, lesbian, gay, bisexual
Obesity is a key public health issue for U.S. adolescents and young adults, [1, 2] that confers numerous health risks, such as heart disease and diabetes.[1] Previous research has found sexual orientation health disparities in body mass index (BMI) that are modified by gender.[3, 4] Specifically, sexual minority female adults have higher BMI and sexual minority male adults (especially gay males) have lower BMI, compared to their heterosexual counterparts.[5–7] A similar pattern has been found among adolescents in the Growing Up Today Study (GUTS), a U.S. national cohort of youth; among females, sexual minorities had higher BMI compared to heterosexuals, whereas among males, heterosexuals displayed steeper increases in BMI through adolescence and into young adulthood compared to sexual minorities, especially gay males.[3] Although sexual orientation patterns in BMI have been established, the basis for these disparities remains to be explained.
Sexual Minority Stress Theory proposes that sexual minorities experience stressors related to the stigmatization of non-heterosexuality and these stressors produce negative health outcomes[8] via a psychological stress response pathway.[9] For example, previous research has found that sexual minorities are more likely than heterosexuals to experience stressors such as victimization[10] and child abuse.[11, 12] In addition, sexual minority youth have worse health outcomes compared to their heterosexual counterparts, including more depressive symptoms[8, 13], PTSD[14], and eating disorder symptoms.[15, 16] Independent of sexual orientation, sexual orientation mobility (also termed sexual fluidity) refers to changes in sexual identity over time.[17] Although some change in sexual identity is normative during adolescence, multiple changes might indicate stress related to identifying as a sexual minority. The potential stressful effects of sexual orientation mobility appear to be modified by gender; greater mobility was related to greater substance use among females and to a lesser extent among males in GUTS.[18] More research is needed to understand why experiencing stressors may lead to sexual orientation health disparities. The current study included sexual orientation mobility as a covariate, conceptualized as a potential stressor, to explain sexual orientation disparities in BMI.
One possible contributor to sexual orientation disparities in BMI is increased exposure among sexual minorities to stressors, such as child abuse. In a study of adult women, childhood sexual abuse partially explained disparities in obesity between lesbians and heterosexuals.[6] Exposure to violence in the home during childhood is related to greater likelihood of being overweight among adolescent females and males, [19] which may account for sexual orientation disparities in BMI among females. However, it remains unclear whether child abuse explains sexual orientation disparities in BMI among males. The link between child abuse and sexual orientation disparities in BMI may be explained by the association between child abuse and negative mental health outcomes among sexual minorities. In the GUTS cohort, greater risk of PTSD – an indicator of extreme stress – observed among sexual minority compared to heterosexual youth was partially accounted for by child abuse.[20] Unhealthy weight-related behaviors, which may have obesogenic or leptogenic effects, may contribute to sexual orientation disparities in BMI as part of a gender-modified stress pathway. In the GUTS cohort, sexual minority women and men were more likely to report binge eating and purging, compared to their heterosexual counterparts.[15] Sexual minorities may use unhealthy weight-related behaviors – for example, fast food consumption or calorie restriction – as a way of coping with stressors, such as child abuse, leading to elevated or reduced BMI, relative to heterosexuals. Female and male sexual minorities may use different weight-related behaviors in response to stressors, leading to differential patterns in BMI disparities. To our knowledge, no previous study has examined child abuse history and weight-related behaviors to explain gendered sexual orientation disparities in BMI among adolescents.
The current study examined child abuse as a moderator in a gender-modified stress pathway to sexual orientation disparities in BMI among youth, using 11 years of data from GUTS. Previous research with the GUTS cohort has found that sexual minority females have higher BMI and sexual minority males have lower BMI, compared to same-gender heterosexuals; and that sexual minority females display greater one-year increases in BMI, and sexual minority males display smaller one-year increases, compared to same-gender heterosexual youth.[3] We use these findings as a starting point and further hypothesize that: 1) unhealthy weight-related behaviors will partially account for elevated BMI in sexual minority females and reduced BMI in sexual minority males, compared with same-gender heterosexuals; 2) sexual orientation mobility will be positively associated with BMI in females, but not in males; and 3) child abuse will partially account for elevated BMI in sexual minority females.
Methods
Study Sample
The original sample size for the current analyses was 16,882 (9039 females, 7843 males) from the GUTS cohort. After exclusion criteria (described below) were applied, the final sample size was 13,952 (7960 females, 5992 males), 86.2% of the original cohort. GUTS is a prospective cohort of children of women participating in the Nurses’ Health Study II.[21] Recruitment information for GUTS is detailed elsewhere.[22] Youth ages 9 to 14 years were originally enrolled in 1996 and followed annually or biennially. For the current study, data were used from assessments collected from participants across nine waves from 1996 (age 12 to 14 years) to 2007 (age 20 to 25 years). The racial/ethnic breakdown of the sample is 93.3% white and 6.7% other race/ethnicities.
Participants were excluded if they were missing data or reported “not sure” for sexual orientation at all waves (971 females, 10.7%; 1791 males, 22.8%); if they were missing BMI at all waves (2 females, <1%; 4 males, <1%); and if they indicated any of the following health conditions that could interfere with growth (106 females, 1.3%; 56 males, <1%): diabetes, juvenile rheumatoid arthritis, inflammatory bowel disease, cerebral palsy, Down syndrome, acute lymphocytic leukemia, and other selected conditions and congenital anomalies. This study was approved by the Brigham and Women’s Hospital Institutional Review Board.
Measures – Predictors
Sexual orientation
Sexual orientation was assessed in waves 1999 to 2007 with the item “Which of the following best describes your feelings?” and the following response options: completely heterosexual (attracted to persons of the opposite sex), mostly heterosexual, bisexual (equally attracted to men and women), mostly homosexual, completely homosexual (gay/lesbian, attracted to persons of the same sex), and not sure. Sexual orientation groups were modeled based on the most recent report of sexual orientation within the included waves and then back-assigned to all previous waves. Mostly homosexual and completely homosexual were combined into a lesbian/gay group due to small sample sizes.
Sexual orientation mobility
Sexual orientation mobility was calculated at each wave based on changes in reported sexual orientation.[17, 18] A score was assigned to each participant based on the number of times sexual orientation changed. Scores ranged from 0 (no change at any wave) to 1 (change at all waves in which sexual orientation was reported). Sexual orientation mobility was recoded into three groups: no mobility (score = 0), low mobility (score = .01 to .50), and high mobility (score = .51 to 1).
Child abuse history
Child abuse occurrence by age 11 years was measured retrospectively in 2007 using two items from the Child Abuse Questionnaire[23], four items from the Conflict Tactics Scale[24], and two items from the Sexual Experiences Survey[25], which assessed emotional, physical, and sexual abuse, respectively. Two additional items assessed witnessing physical and verbal abuse in the household during childhood. Emotional and physical abuse were measured as never, rarely, sometimes, often, very often. Sexual abuse was measured as never, once, more than once. Witnessing physical and verbal abuse was measured as never, once, a few times, more than a few times, all the time. Specific types of abuse were dichotomized as follows: never/rarely vs. sometimes/often/very often for emotional and physical abuse, never vs. once/more than once for sexual abuse, and never vs. once/a few times/more than a few times/all the time for witnessing abuse. Then abuse was coded into: none, 1 type, 2 types, and 3–4 types.
Measures – Outcome
BMI
Age-specific raw BMI was assessed continuously as kg/m2 across nine waves from 1996 to 2007, restricted to age 12 and older. Self-reported height and weight were used to calculate BMI. Adolescents are able to provide valid self-reports of height and weight.[26] BMI reported while pregnant was treated as missing for female participants, only for the wave at which pregnancy was reported.
Measures – Covariates
Sociodemographics
Age was assessed continuously, modeled linearly and quadratically, and coded as: younger (9– 11 years), older (12– 14 years) to measure cohort effects. Gender was coded as: female, male. Race/ethnicity was coded as: white, non-white. Household income was reported by mothers in 2001 and coded as: low (< $50,000/year), high (≥ $50,000/year).
Weight-related behaviors
Over the nine waves included in these analyses, GUTS surveys have collected a large volume of repeated measures on a range of weight-related behaviors. As a data reduction method and to accommodate the variability in waves in which particular behaviors were assessed, we used latent growth mixture model methods in Mplus for each weight-related behavior to capture a participant’s overall trajectory on the variable, which were then used to categorize participants into groups (see Tables 1 and 2).[27, 28] Models used to create empirically derived trajectory groups were gender-stratified for the following weight-related behaviors: sugar-sweetened beverage consumption, binge eating, and caloric intake. Model fit was assessed using Bayesian information criterion (BIC)[29], the Lo Mendelle Rubin likelihood ratio test (LMR LRT)[30], and entropy, a weighted average of posterior probability[31]. BIC and LMR LRT were used to select the optimal number of trajectory groups, and entropy was used to assess classification quality. Participants were categorized based on the highest posterior probability of membership in a particular empirically derived trajectory group. TV-viewing was measured as mean number of hours per week and categorized as tertiles to take into account variability at each wave, across eight waves between 1996 and 2005. Sugar-sweetened beverage consumption was measured as mean number of servings (bottle/can) per month, week, or day, across six waves between 1996 and 2001. Binge eating was measured as any binge eating in the past year, across nine waves between 1996 and 2007. Family dinner was measured as mean frequency per week, across three waves between 1996 and 1998. Fast food consumption was measured as mean number of days per week, across six waves between 1996 and 2001. Caloric intake was measured as total kcals per day estimated for the past year using the Food Frequency Questionnaire[32, 33], with tertiles created for each wave across six waves between 1996 and 2001.
Table 1.
Sample Demographics and Descriptive Analyses by Gender in a Longitudinal Cohort of Adolescent Females and Males (N = 13,952)
| Measure | Females (n = 7960) |
Males (n = 5992) |
|---|---|---|
| Age at 1996 (N, %) | ||
| Younger group (9–11 years) | 49.9 | 54.6 |
| Older group (12–14 years) | 50.1 | 45.4 |
| Race/Ethnicity (%) | ||
| White | 93.0 | 92.9 |
| Non-white | 7.0 | 7.1 |
| Income (%) | ||
| Low (< $50,000) | 10.3 | 10.4 |
| High (≥ $50,000) | 68.3 | 70.4 |
| Missinga | 21.4 | 19.2 |
| Sexual Orientationb (%) | ||
| Completely heterosexual | 80.7 | 91.1 |
| Mostly heterosexual | 15.9 | 6.1 |
| Bisexual | 2.1 | 0.7 |
| Lesbian/gay | 1.3 | 2.1 |
| Sexual Orientation Mobility (%) | ||
| None (0) | 60.0 | 55.6 |
| Low (.01–.5) | 15.9 | 7.9 |
| High (.51–1) | 5.1 | 2.7 |
| Missing | 18.9 | 33.9 |
| Child Abuse History (%) | ||
| None | 34.7 | 25.8 |
| 1 type | 18.4 | 16.0 |
| 2 types | 11.0 | 7.8 |
| 3–4 types | 7.0 | 4.4 |
| Missing | 28.9 | 46.0 |
| Weight-Related Behavior Trajectory Group Membershipc (%) | ||
| TV viewing | ||
| Med to low | 38.7 | 28.4 |
| Med to high | 22.5 | 32.2 |
| High to low | 38.9 | 39.4 |
| Sugar-sweetened beverage consumption | ||
| Low | 24.1 | 22.1 |
| Medium | 31.9 | 51.2 |
| High | 29.0 | 26.8 |
| High to low | 15.1 | - |
| Binge eating | ||
| No binge | 90.9 | 99.0 |
| Binge | - | 1.0 |
| Early onset binge | 4.0 | - |
| Late onset binge | 5.1 | - |
| Family dinner | ||
| Some to never | 2.6 | 1.5 |
| Most to some | 20.4 | 16.4 |
| Most | 42.4 | 43.8 |
| Everyday | 34.6 | 38.4 |
| Fast food consumption | ||
| Low | 41.2 | 28.6 |
| Medium | 49.1 | 56.9 |
| Medium to high | 9.7 | 14.5 |
| Caloric intake | ||
| Low | - | 36.4 |
| Medium | - | 30.6 |
| High | - | 33.0 |
| Low to medium | 26.6 | - |
| Low to high | 10.1 | - |
| Medium to low | 23.5 | - |
| Medium to high | 30.3 | - |
| High to low | 9.5 | - |
Frequency of missingness is reported for variables for which missing indicator method was used to handle missingness; this method treats missing data as an additional category for nominal variables.
Sexual orientation is from the most recent wave reported.
Weight-related behavior trajectory groups were generated through latent growth model methods with repeated measures. Latent growth model methods used to create weight-related behavior trajectory groups were stratified by gender, such that models for females and males yielded different groups for some variables. Frequencies may not add up to 100% for some weight-related behaviors due to rounding. Percent missing for specific weight-related behaviors is not reported because missingness was n < 17 per gender group.
Table 2.
Sexual Orientation Mobility, Child Abuse History, and Weight-Related Behaviors by Sexual Orientation and Gender in a Longitudinal Cohort of Adolescent Females and Males (N = 13,952)
| Females (n = 7960) | Males (n = 5992) | |||||||
|---|---|---|---|---|---|---|---|---|
| Completely heterosexual (n=6422) |
Mostly heterosexual (n=1264) |
Bisexual (n=170) | Lesbian (n=104) |
Completely heterosexual (n=5456) |
Mostly heterosexual (n=368) |
Bisexual (n=43) |
Gay (n=125) |
|
| Sexual Orientation Mobility (%) | ||||||||
| None | 72.6 | 7.6 | 6.5 | 6.7 | 60.2 | 7.1 | 4.7 | 14.4 |
| Low | 5.5 | 61.5 | 54.1 | 45.2 | 3.3 | 59.0 | 32.6 | 48.8 |
| High | 1.8 | 17.1 | 25.9 | 31.7 | 1.5 | 12.0 | 27.9 | 20.0 |
| χ2 (9) = 3976.59***a | χ2 (9) = 2311.24*** | |||||||
| Child Abuse History (%) | ||||||||
| None | 35.7 | 31.7 | 21.8 | 30.8 | 25.7 | 28.3 | 14.0 | 28.0 |
| 1 type | 17.8 | 21.8 | 16.5 | 19.2 | 15.3 | 21.5 | 14.0 | 29.6 |
| 2 types | 10.1 | 14.7 | 14.7 | 17.3 | 7.1 | 15.5 | 18.6 | 12.0 |
| 3–4 types | 5.5 | 12.1 | 19.4 | 13.5 | 3.8 | 9.8 | 9.3 | 12.8 |
| χ2 (9) = 173.69***a | χ2 (9) = 150.51***a | |||||||
| Weight-Related Behav Trajec Grp Membershipb (%) | ||||||||
| TV viewing | ||||||||
| Med to low | 39.0 | 36.9 | 41.2 | 34.6 | 28.2 | 30.4 | 30.2 | 26.4 |
| Med to high | 22.1 | 23.7 | 22.9 | 26.9 | 32.4 | 32.1 | 44.2 | 23.2 |
| High to low | 38.8 | 39.5 | 35.9 | 38.5 | 39.4 | 37.5 | 25.6 | 50.4 |
| χ2 (6) = 4.58 | χ2 (6) = 12.17 | |||||||
| Sugar-sweetened beverages | ||||||||
| Low | 23.5 | 26.1 | 30.6 | 26.2 | 15.4 | 23.9 | 27.9 | 22.4 |
| Medium | 32.3 | 31.3 | 24.1 | 31.1 | 51.1 | 52.2 | 55.8 | 52 |
| High | 29.6 | 26.0 | 28.2 | 30.1 | 27.1 | 23.9 | 16.3 | 25.6 |
| High to low | 14.8 | 16.5 | 17.1 | 12.6 | - | - | - | - |
| χ2 (9) = 17.74* | χ2 (6) = 4.72 | |||||||
| Binge eating | ||||||||
| No binge | 92.5 | 84.6 | 81.8 | 87.4 | 99.3 | 97.6 | 97.7 | 92.8 |
| Binge | - | - | - | - | 0.7 | 2.4 | 2.3 | 7.2 |
| Early onset binge | 3.3 | 7.0 | 6.5 | 6.8 | - | - | - | - |
| Late onset binge | 4.3 | 8.5 | 11.8 | 5.8 | - | - | - | - |
| χ2 (6) = 101.22*** | χ2 (3) = 63.50*** | |||||||
| Family dinner | ||||||||
| Some to never | 2.3 | 3.9 | 4.7 | 2.9 | 1.4 | 3.0 | 0.0 | 1.6 |
| Most to some | 20.2 | 20.5 | 24.1 | 24.0 | 16.2 | 15.8 | 20.9 | 20.8 |
| Most | 42.3 | 44.7 | 32.4 | 32.7 | 43.6 | 44.6 | 46.5 | 42.4 |
| Everyday | 35.2 | 30.9 | 38.8 | 40.4 | 38.5 | 36.7 | 32.6 | 35.2 |
| χ2 (9) = 31.19*** | χ2 (9) = 9.92 | |||||||
| Fast food | ||||||||
| Low | 40.6 | 43.9 | 44.7 | 40.8 | 27.9 | 35.6 | 27.9 | 34.4 |
| Medium | 49.9 | 46.3 | 42.9 | 43.7 | 57.2 | 53.5 | 58.1 | 51.2 |
| Med to high | 9.5 | 9.8 | 12.4 | 15.5 | 14.8 | 10.6 | 14.0 | 14.4 |
| χ2 (6) = 13.20* | χ2 (6) = 14.32* | |||||||
| Caloric intake | ||||||||
| Low | - | - | - | - | 35.9 | 38.9 | 48.8 | 46.4 |
| Medium | - | - | - | - | 30.5 | 32.3 | 27.9 | 28.0 |
| High | - | - | - | - | 33.5 | 28.5 | 23.3 | 25.6 |
| Low to med | 26.8 | 25.6 | 25.9 | 26.2 | - | - | - | - |
| Low to high | 9.9 | 11.0 | 9.4 | 14.6 | - | - | - | - |
| Med to low | 22.8 | 26.4 | 25.9 | 25.2 | - | - | - | - |
| Med to high | 30.9 | 28.1 | 27.7 | 23.3 | - | - | - | - |
| High to low | 9.6 | 9.0 | 11.2 | 10.7 | - | - | - | - |
| χ2 (12) = 16.12 | χ2 (6) = 13.01* | |||||||
χ2 is calculated by comparing sexual orientation groups to each categorical outcome, stratified by gender.
Weight-related behavior trajectory groups were generated through latent growth model methods with repeated measures. Latent growth model methods used to create trajectories groups were stratified by gender, such that models for females and males yielded different groups for some variables.
p<.05
p<.01
p<.001
Statistical Analysis
All analyses were longitudinal and conducted in Mplus, using data collected across nine waves between 1996 and 2007. Analyses were gender-stratified, with completely heterosexual as the reference group. Descriptive statistics were calculated for all variables by gender (Table 1) and for sexual orientation mobility, child abuse history, and weight-related behavior trajectory groups by gender and sexual orientation (Table 2).
To test the hypotheses, we conducted latent quadratic growth model analyses using repeated measures to model development of BMI in youth ages 12 to 25 years. The first set of models adjusted for sexual orientation and sociodemographics only (Model 1); the second set of models additionally adjusted for child abuse history (Model 2); and the final set of models additionally adjusted for weight-related behavior trajectory groups (Model 3). BMI at age 17 years (intercept) and one-year change in BMI (slope) are reported. Relative BMI at age 17 years was used to represent the intercept because age 17 years was in the middle of the age range and this age group had the highest number of observations. Missing indicator method[34, 35] was used to handle missingness in sexual orientation mobility, household income, child abuse history, and weight-related behaviors. This method treats missing data as an additional category for nominal variables, thereby preserving statistical power that may be otherwise lost if complete case analysis method is used to handle missingness.
Results
Sample demographics and descriptive analyses by gender for all variables are reported in Table 1. Descriptive analyses for sexual orientation mobility, child abuse history, and weight-related behavior trajectory groups by sexual orientation and gender are displayed in Table 2. Sexual orientation mobility significantly differed by sexual orientation, with sexual minority females and males reporting greater mobility than completely heterosexuals. All levels of child abuse significantly differed by sexual orientation for females and males (Table 2). Among both genders, sexual minorities were more likely than heterosexuals to report experiencing more than one type of child abuse. Among females, sexual minorities had elevated rates of binge eating and fast food consumption, compared to completely heterosexuals (Table 2). Consumption of sugar-sweetened beverages and frequency of family dinners also differed significantly by sexual orientation among females, but the direction of the difference was variable. Among males, sexual minorities had elevated rates of binge eating compared to completely heterosexuals, but lower rates of fast food consumption and caloric intake (Table 2).
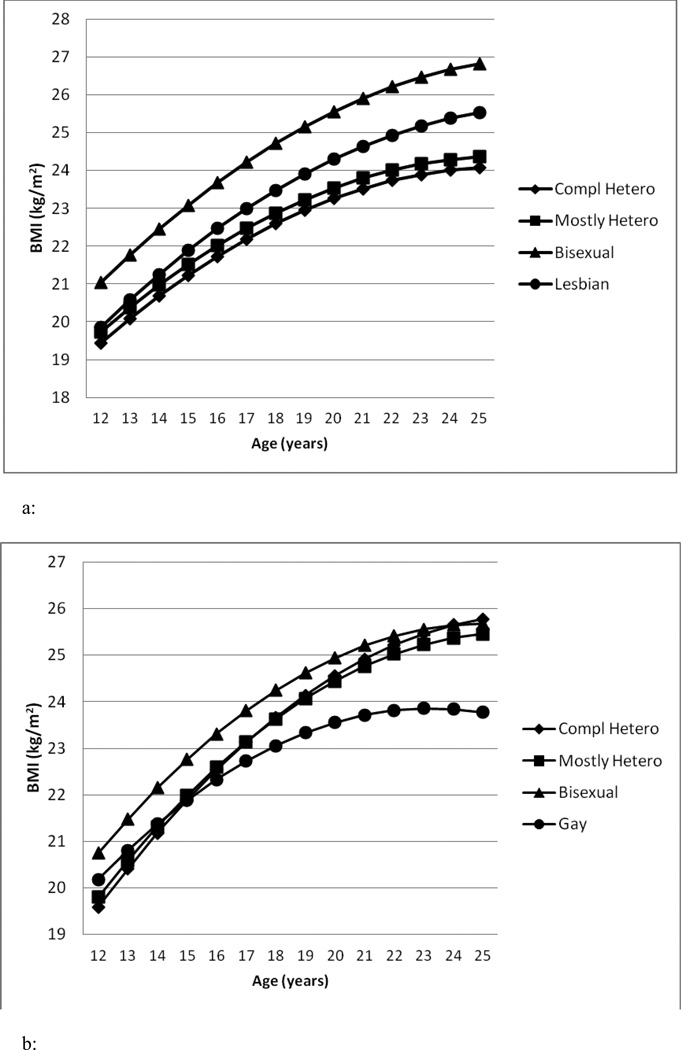
Results from latent quadratic growth models with females indicated that bisexuals had higher BMI at age 17 years (β = 1.59, 95% CI = 1.00, 2.18) and displayed greater one-year increases in BMI (β = .09, 95% CI = .03, .14), compared to completely heterosexuals (Table 3, Model 1; Figure 1a). The regression coefficient indicating one-year change in BMI for lesbians (β = .07, 95% CI = .00, .15) was similar in magnitude to bisexuals; however, it did not reach significance (p = .052). Sexual orientation mobility was positively associated with BMI at age 17 years, but not one-year change in BMI, among females.
Table 3.
Multivariable Linear Regression Coefficientsa from Models with Child Abuse History and Weight-Related Behaviors Predicting Sexual Orientation Disparities in BMI (kg/m2) Among Female Youth (N = 7960
| Estimated Group Differences in BMIb at Age 17 Years (Intercept) |
Estimated Group Differences in One-Year Change in BMI (Slope) |
|||||
|---|---|---|---|---|---|---|
| Model 1c: Sex Orient & Demographics |
Model 2d: Sex Orient, Demographics & Child Abuse |
Model 3e: Sex Orient, Demographics, Child Abuse & Weight-Related Behaviors |
Model 1: Sex Orient & Demographics |
Model 2: Sex Orient, Demographics & Child Abuse |
Model 3: Sex Orient, Demographics, Child Abuse & Weight-Related Behaviors |
|
| Measures | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) |
| Sexual Orientation | ||||||
| Completely htero (n=6422) | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) |
| Mostly hetero (n=1264) | −.08 (−.37, .22) | −.10 (−.40, .19) | −.20 (−.49, .09) | .00 (−.03, .03) | .00 (−.03, .03) | −.01 (−.04, .02) |
| Bisexual (n=170) | 1.59 (1.00, 2.18)a | 1.51 (.93, 2.10) | 1.46 (.88, 2.04) | .09 (.03, .14) | .08 (.02, .14) | .08 (.02, .13) |
| Lesbian (n=104) | .37 (−.36, 1.09) | .34 (−.39, 1.07) | .28 (−.44, 1.00) | .07 (.00, .15) | .07 (.00, .14) | .07 (.00, .14) |
| Sexual Orientation Mobility | ||||||
| None | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) |
| Low mobility | .44 (.14, .74) | .42 (.13, .72) | .36 (.07, .66) | .00 (−.03, .03) | −.01 (−.03, .02) | .00 (−.03, .03) |
| High mobility | .81 (.40, 1.22) | .76 (.34, 1.17) | .68 (.27, 1.08) | .02 (−.02, .06) | .02 (−.02, .06) | .02 (−.02, .06) |
| Child Abuse | ||||||
| None | (ref) | (ref) | (ref) | (ref) | ||
| 1 type | .28 (.05, .51) | .14 (−.08, .37) | .02 (.00, .04) | .02 (.00, .040 | ||
| 2 types | .35 (.07, .62) | .24 (−.03, .51) | .02 (−.01, .05) | .02 (−.01, .05) | ||
| 3–4 types | .65 (.32, .98) | .43 (.10, .76) | .05 (.02, .08) | .05 (.01, .08) | ||
Significant effects are bolded.
BMI was measured in kg/m2. Relative BMI at age 17 was used to represent the intercept because age 17 was more interpretable than BMI at age 0, and this age group had the highest number of participants contributing data.
Model 1 included sexual orientation, sexual orientation mobility, and the following demographic covariates: age, race/ethnicity, and income.
Model 2 included sexual orientation, sexual orientation mobility, child abuse history, and demographic covariates.
Model 3 included sexual orientation, sexual orientation mobility, child abuse history, demographic covariates, and weight-related covariates: TV-viewing, sugar-sweetened beverage consumption, binge eating, family dinner frequency, fast food consumption, and caloric intake.
Figure 1.
a: BMI Trajectories Estimated from Model 1 by Sexual Orientation for Females
b: BMI Trajectories Estimated from Model 1 by Sexual Orientation for Males
Results from latent quadratic growth models with males indicated no significant differences among sexual orientations in BMI at age 17 years (Table 4, Model 1); however, gay males displayed smaller one-year increases in BMI (β = −.19, 95% CI = −.25, −.12), compared to completely heterosexuals (Table 4, Model 1). In fact, by age 25 years, gay males had a BMI two units lower than completely heterosexuals (gay males: 23.8 kg/m2, completely heterosexuals: 25.8 kg/m2; Figure 1b). Sexual orientation mobility did not significantly predict BMI at age 17 years or one-year change in BMI among males.
Table 4.
Multivariable Linear Regression Coefficients from Models with Child Abuse History and Weight-Related Behaviors Predicting Sexual Orientation Disparities in BMI (kg/m2) Among Male Youth (N = 5992)
| Estimated Group Differences in BMIb at Age 17 Years (Intercept) |
Estimated Group Differences in One-Year Change in BMI (Slope) | |||||
|---|---|---|---|---|---|---|
| Model 1c: Sex Orient & Demographics |
Model 2d: Sex Orient, Demographics & Child Abuse |
Model 3e: Sex Orient, Demographics, Child Abuse & Weight-Related Behaviors |
Model 1: Sex Orient & Demographics |
Model 2: Sex Orient, Demographics & Child Abuse |
Model 3: Sex Orient, Demographics, Child Abuse & Weight-Related Behaviors |
|
| Measures | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) |
| Sexual Orientation | ||||||
| Completely hetero (n=5456) | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) |
| Mostly hetero (n=368) | .19 (−.29, .67) | .15 (−.33, .63) | .12 (−.35, .60) | −.03 (−.08, .02) | −.03 (−.08, .02) | −.03 (−.08, .02) |
| Bisexual (n=43) | .73 (−.42, 1.89) | .67 (−.49, 1.82) | .46 (−.67, 1.60) | −.08 (−.20, .04) | −.09 (−.21, .03) | −.09 (−.21, .03) |
| Gay (n=125) | −.23 (−.94, .48) | −.30 (−1.01, .42) | −.47 (−1.17, .23) | −.19 (−.25, −.12)a | −.19 (−.26, −.12) | −.18 (−.25, −.12) |
| Sexual Orientation Mobility | ||||||
| None | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) |
| Low | −.23 (−.67, .22) | −.26 (−.70, .18) | −.30 (−.73, .14) | −.02 (−.07, .02) | −.03 (−.07, .02) | −.03 (−.07, .02) |
| High | .01 (−.62, .64) | −.03 (−.66, .60) | −.07 (−.69, .55) | −.03 (−.09, .03) | −.03 (−.09, .03) | −.03 (−.09, .04) |
| Child Abuse | ||||||
| None | (ref) | (ref) | (ref) | (ref) | ||
| 1 type | .43 (.12, .73) | .37 (.08, .67) | .02 (−.01, .05) | .02 (−.01, .05) | ||
| 2 types | .39 (.00, .78) | .31 (−.07, .69) | .04 (.00, .07) | .03 (.00, .07) | ||
| 3–4 types | 1.04 (.55, 1.53) | .86 (.37, 1.34) | .04 (−.01, .08) | .04 (−.01, .08) | ||
Significant effects are bolded.
BMI was measured in kg/m2. Relative BMI at age 17 was used to represent the intercept because age 17 was more interpretable than BMI at age 0, and this age group had the highest number of participants contributing data.
Model 1 included sexual orientation, sexual orientation mobility, and the following demographic covariates: age, race/ethnicity, and income.
Model 2 included sexual orientation, sexual orientation mobility, child abuse history, and demographic covariates.
Model 3 included sexual orientation, sexual orientation mobility, child abuse history, demographic covariates, and weight-related covariates: TV-viewing, sugar-sweetened beverage consumption, binge eating, family dinner frequency, fast food consumption, and caloric intake.
For females, all levels of child abuse were positively associated with BMI at age 17 years, and the highest level of child abuse (3–4 types) was positively associated with one-year change in BMI (Table 3, Model 2). The relationship between the highest level of child abuse and BMI at age 17 years in females was attenuated by 34% after controlling for weight-related behaviors (Table 3, Model 3). For males, some levels of child abuse were positively associated with BMI at age 17 years, but child abuse did not predict one-year change in BMI (Table 4, Model 2). The relationship between child abuse and BMI remained after controlling for weight-related behaviors in males, but was attenuated by as much as 17%.
The estimated differences between bisexual females and completely heterosexual females in BMI at age 17 years and one-year change in BMI were attenuated by a small amount (8% and 11%, respectively), but remained significant after controlling for level of child abuse and weight-related behaviors (Table 3, Models 2 and 3). The estimated difference between gay males and completely heterosexual males in change in BMI over a one-year interval was not affected by controlling for level of child abuse and weight-related behaviors (Table 4, Models 2 and 3).
Discussion
The current study examined predictors of sexual orientation disparities in BMI among youth. Bisexual females had higher BMI at age 17 years and greater one-year increases in BMI, compared to completely heterosexual females. Lesbians also indicated a trend toward greater one-year increases in BMI compared to completely heterosexual females; but the difference was not significant perhaps due to a smaller number of lesbians in the sample (n = 104) compared to bisexuals (n = 170). Contrary to expectations, sexual minority males did not have lower BMI at age 17 years, compared to heterosexual males; however, gay males had smaller one-year increases in BMI. These patterns largely confirm previous research demonstrating gendered sexual orientation disparities in BMI.[3, 5, 6] Our study findings extend this literature by documenting that among female youth, elevated BMI in bisexuals is partially explained by disparities in child abuse and obesogenic weight-related behaviors.
Sexual orientation disparities in BMI among females may be a consequence of using unhealthy weight-related behaviors as a coping mechanism in response to critical stressors such as child abuse victimization. Importantly, results from this study do not support a similar pathway for sexual minority males, who also experience higher rates of child abuse but do not have elevated BMI compared to completely heterosexual males. Gender may modify the relationship between stressors and weight-related behaviors in sexual minorities, due to gender differences in coping strategies. For instance, females are more likely than males to respond to stress by engaging in maladaptive ruminative coping[36], which has been linked to binge eating in females.[37] Although results from the current study support this gendered stress pathway to sexual orientation disparities in BMI, other research has indicated gender and sexual orientation group similarities. Rumination and consumptive coping (coping through consumption of food, alcohol, and drugs) have been documented in response to childhood sexual abuse in both females and males.[38] In addition, females and sexual minorities may experience similar stressors based on their lowered status in society, which interact with particular coping styles (e.g., rumination), to produce greater rates of depression compared to males and heterosexuals.[39] However, this does not explain why BMI would be higher for female bisexuals and male heterosexuals, compared to other groups. Gender differences in stressors and coping styles may account for gender differences in sexual orientation disparities in BMI in the current study, but more research is needed to reconcile these contradictory findings.
Sexual orientation mobility was positively associated with BMI in females, but not in males. In a previous study with the GUTS cohort, sexual orientation mobility was positively associated with substance use and this finding was of higher magnitude among females,[18] suggesting that sexual orientation mobility might confer more risk for negative health outcomes in females than males. More research is needed to explore gender differences in how sexual orientation mobility is related to health and also how the direction of sexual orientation mobility (from heterosexual to sexual minority or vice versa) may relate to health.
Differences in BMI increases over time were observed between gay males and completely heterosexual males, emerging around age 17 (see Figure 1b). However, we did not find that child abuse or weight-related behaviors explained this difference. Compared to completely heterosexual males, gay males had higher prevalence of child abuse, which we would expect to increase, not reduce BMI. Also, although gay males appeared to have lower prevalence of some obesogenic behaviors (fast food consumption and caloric intake) compared to completely heterosexual males, they had higher binge eating. An alternative explanation for our findings may be reporting bias. Other research has found that gay males underreport their BMI by an estimated .37 units compared to heterosexual males.[40] However, in the current study the difference between gay and completely heterosexual males’ BMI at age 25 was much larger – as much as two units – which far exceeds the amount expected to be attributable to reporting bias. Other unmeasured factors are likely related to sexual orientation disparities in BMI among males.
Some potential limitations should be mentioned. Acknowledging a history of child abuse is stigmatizing, therefore underreporting may be an issue. In addition, although we gave the same weight to different types of abuse, it would be useful in future research to identify how different types of child abuse may be related to long-term negative health outcomes in sexual minority youth. These data did not allow for an investigation of the mechanisms linking sexual minority status to child abuse. Another limitation is the homogeneity of the sample in race/ethnicity and household income. More research is needed using samples with greater racial/ethnic and income diversity. Finally, all self-report measures are likely to result in some misclassification, and this is also true for one-year dietary recall. To mitigate the effects of imprecision in dietary recall, we used the validated Food Frequency Questionnaire[32, 33] to collect weight-related behavior information and then created trajectory groups for each weight-related behavior. Nevertheless, misclassification may still have affected our measures of dietary behaviors.
Sexual orientation disparities in BMI and child abuse history have important implications for adolescent and young adult health. It is clear that sexual minorities experience greater stressors, such as child abuse, compared to heterosexuals, which negatively affects their health. Health care providers caring for sexual minority youth should be aware of these disparities, particularly elevated risk for higher BMI in bisexual females and heterosexual males. More research is needed to understand the various determinants of sexual orientation health disparities, including BMI. Interventions aimed at preventing obesity should address the use of unhealthy weight-related behaviors as coping mechanisms in responses to stressors, including those differentially experienced by sexual minorities (e.g., sexual orientation-based victimization and child abuse). Interventions targeting unhealthy weight-related behaviors and obesity must be inclusive of all sexual orientations to promote health equity in all youth.
Implications and Contribution.
Health care providers working with youth should be aware of elevated risk for higher BMI and greater increases in BMI in bisexual females and heterosexual males. Programs promoting healthful weight-control and obesity prevention must be sensitive to the needs of all sexual orientation groups.
Acknowledgements
NIH R01 HD066963; Leadership Education in Adolescent Health project, Maternal and Child Health Bureau HRSA grant 6T71-MC00009.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sabra L. Katz-Wise, Division of Adolescent and Young Adult Medicine, Boston Children’s Hospital, 300 Longwood Ave (AU-Box 17), Boston, MA 02115, 617-355-0924 (office), 617-730-0004 (fax), sabra.katz-wise@childrens.harvard.edu.
Hee-Jin Jun, Boston, MA.
Heather L. Corliss, Division of Adolescent and Young Adult Medicine, Boston Children’s Hospital.
Benita Jackson, Department of Psychology, Smith College.
Jess Haines, Department of Family Relations and Applied Nutrition, University of Guelph.
S. Bryn Austin, Division of Adolescent and Young Adult Medicine, Boston Children’s Hospital.
References
- 1.Institute of Medicine. Committee on Prevention of Obesity in Children and Youth. In: Koplan JP, Liverman CT, Kraak VA, editors. Preventing childhood obesity: Health in the balance. The National Academies Press; 2005. [PubMed] [Google Scholar]
- 2.Singh AS, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity Reviews. 2008;9(5):474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 3.Austin S, et al. Sexual orientation disparities in weight status in adolescence: Findings from a prospective study. Obesity. 2009;17(9):1776–1782. doi: 10.1038/oby.2009.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowen DJ, Balsam KF, Ender SR. A review of obesity issues in sexual minority women. Obesity. 2008;16(2):221–228. doi: 10.1038/oby.2007.34. [DOI] [PubMed] [Google Scholar]
- 5.Deputy NP, Boehmer U. Determinants of body weight among men of different sexual orientation. Preventive Medicine. 2010;51(2):129–131. doi: 10.1016/j.ypmed.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 6.Smith HA, et al. Sexual abuse, sexual orientation, and obesity in women. Journal of Women's Health. 2010;19(8):1525–1532. doi: 10.1089/jwh.2009.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jun HJ, et al. Adult body mass index trajectories and sexual orientation: the Nurses' Health Study II. American Journal of Preventive Medicine. 2012;42(4):348–354. doi: 10.1016/j.amepre.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hatzenbuehler ML. How does sexual minority stigma"get under the skin"? A psychological mediation framework. Psychological Bulletin. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Katz-Wise SL, Hyde JS. Victimization experiences of lesbian, gay, and bisexual individuals: A meta-analysis. Journal of Sex Research. 2012;49(2–3):142–167. doi: 10.1080/00224499.2011.637247. [DOI] [PubMed] [Google Scholar]
- 11.Saewyc EM, et al. Hazards of stigma: the sexual and physical abuse of gay, lesbian, and bisexual adolescents in the United States and Canada. Child Welfare. 2006;85(2):195–213. [PubMed] [Google Scholar]
- 12.McLaughlin KA, et al. Disproportionate exposure to early-life adversity and sexual orientation disparities in psychiatric morbidity. Child Abuse & Neglect. 2012;36(9):645–655. doi: 10.1016/j.chiabu.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosario M, et al. Gay-related stress and emotional distress among gay, lesbian, and bisexual youths: a longitudinal examination. Journal of Consulting and Clinical Psychology. 2002;70(4):967–975. doi: 10.1037//0022-006x.70.4.967. [DOI] [PubMed] [Google Scholar]
- 14.Roberts AL, et al. Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. American Journal of Public Health. 2010;100(12):2433–2441. doi: 10.2105/AJPH.2009.168971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Austin S, et al. Sexual orientation disparities in purging and binge eating from early to late adolescence. Journal of Adolescent Health. 2009;45(3):238–245. doi: 10.1016/j.jadohealth.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feldman MB, Meyer IH. Eating disorders in diverse lesbian, gay, and bisexual populations. International Journal of Eating Disorders. 2007;40(3):218–226. doi: 10.1002/eat.20360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ott MQ, et al. Stability and change in self-reported sexual orientation identity in young people: application of mobility metrics. Archives of Sexual Behaviors. 2011;40(3):519–532. doi: 10.1007/s10508-010-9691-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ott MQ, et al. Repeated changes in reported sexual orientation identity linked to substance use behaviors in youth. Journal of Adolescent Health. 2012:1–8. doi: 10.1016/j.jadohealth.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jun HJ, et al. Growing up in a domestic violence environment: relationship with developmental trajectories of body mass index during adolescence into young adulthood. Journal of Epidemiology & Community Health. 2012;66(7):629–635. doi: 10.1136/jech.2010.110932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts AL, et al. Elevated risk of posttraumatic stress in sexual minority youths: mediation by childhood abuse and gender nonconformity. American Journal of Public Health. 2012;102(8):1587–1593. doi: 10.2105/AJPH.2011.300530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nurses’ Health Study. Brigham and Women’s Hospital/Harvard Medical School [Google Scholar]
- 22.Field AE, et al. Overweight, weight concerns, and bulimic behaviors among girls and boys. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(6):754–760. doi: 10.1097/00004583-199906000-00024. [DOI] [PubMed] [Google Scholar]
- 23.Bernstein DP, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 24.Straus MA, et al. The revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. [Google Scholar]
- 25.Koss MP, Gidycz CA. Sexual Experiences Survey: Reliability and validity. Journal of Consulting and Clinical Psychology. 1985;53(3):422–423. doi: 10.1037//0022-006x.53.3.422. [DOI] [PubMed] [Google Scholar]
- 26.Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106(1 Pt 1):52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- 27.Muthen B, et al. General growth mixture modeling for randomized preventive interventions. Biostatistics. 2002;3:459–475. doi: 10.1093/biostatistics/3.4.459. [DOI] [PubMed] [Google Scholar]
- 28.Muthen L, Muthen B. Mplus User's Guide. 4th ed. Los Angeles, CA: Muthen & Muthen; 2006. [Google Scholar]
- 29.Schwarz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6(2):461–464. [Google Scholar]
- 30.Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. [Google Scholar]
- 31.Nagin DS, Tremblay RE. Analyzing developmental trajectories of distinct but related behaviors: a group-based method. Psychological Methods. 2001;6(1):18. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 32.Rockett HR, et al. Validation of a youth/adolescent food frequency questionnaire. Preventive Medicine. 1997;26(6):808–816. doi: 10.1006/pmed.1997.0200. [DOI] [PubMed] [Google Scholar]
- 33.Rockett HR, Wolf AM, Colditz GA. Development and reproducibility of a food frequency questionnaire to assess diets of older children and adolescents. Journal of the American Dietetic Association. 1995;95(3):336–340. doi: 10.1016/S0002-8223(95)00086-0. [DOI] [PubMed] [Google Scholar]
- 34.Horton NJ, Kleinman KP. Much ado about nothing: A comparison of missing data methods and software to fit incomplete data regression models. The American Statistician. 2007;61(1):79–90. doi: 10.1198/000313007X172556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allison P. Missing data. Vol. 136. Thousand Oaks, CA: Sage Publications, Inc.; 2001. [Google Scholar]
- 36.Nolen-Hoeksema S, Jackson B. Mediators of the gender difference in rumination. Psychology of Women Quarterly. 2001;25(1):37–47. [Google Scholar]
- 37.Harrell ZAT, Jackson B. Thinking fat and feeling blue: Eating behaviors, ruminative coping, and depressive symptoms in college women. Sex Roles. 2008;58(9–10):658–665. [Google Scholar]
- 38.Sarin S, Nolen-Hoeksema S. The dangers of dwelling: An examination of the relationship between rumination and consumptive coping in survivors of childhood sexual abuse. Cognition and Emotion. 2010;24(1):71–85. [Google Scholar]
- 39.Hatzenbuehler ML, Hilt LM, Nolen-Hoeksema S. Gender, sexual orientation, and vulnerability to depression. In: Chrisler JC, McCreary DR, editors. Handbook of gender research in psychology, Vol 2: Gender research in social and applied psychology. New York, NY US: Springer Science + Business Media; 2010. pp. 133–151. [Google Scholar]
- 40.Richmond TK, Walls CE, Austin SB. Sexual orientation and bias in self-reported BMI. Obesity. 2012;20(8):1703–1709. doi: 10.1038/oby.2012.9. [DOI] [PMC free article] [PubMed] [Google Scholar]