Figure 2.
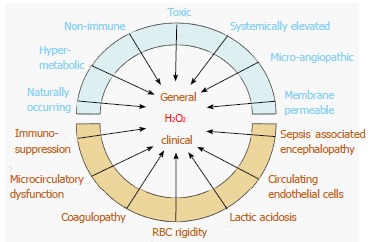
Pathologically elevated serum H2O2 levels can account for the general physiological, histological and clinical abnormalities observed in septic shock. Red blood cell glutathione accounts for a major portion of serum redox buffering capacity and is depleted in septic shock non-survivors vs. survivors. Brain neuron function is highly vulnerable to H2O2 oxidative stress and is manifested by electroencephalographic changes, which can appear before clinical encephalopathy is evident. Studies show that septic shock survivors upregulate serum antioxidant capacity (which decreases H2O2), while non-survivors are unable to do so. This suggests that elevated H2O2 is a necessary concomitant to the development of septic shock and recovery is preceded by decreasing H2O2. The individual clinical course, bookended by these extremes of H2O2, is influenced by parameters such as individual antioxidant capacity, susceptibility to oxidative stress, co-morbidities, age, general health and organ system involved.
