Figure 1.
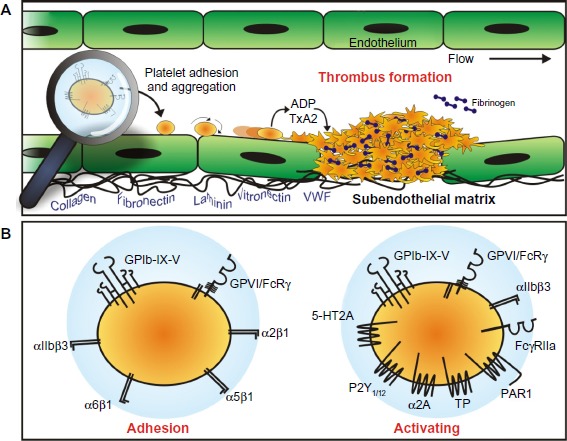
Platelet adhesion and aggregation.
Notes: (A) Platelets normally circulate through the vasculature in a nonadhesive state. Upon the detection of an exposed subendothelial matrix, platelets are induced to come into close contact with the vessel wall and roll, then arrest, at the site of vessel injury. The process of adhesion is orchestrated by the platelet adhesion receptors GPVI and GPIb-IX-V. The release of soluble agonists, such as ADP and thromboxane A2 (TxA2) amplify platelet activation. Platelet adhesion and activation, results in the formation of a platelet plug (thrombus). (B) Platelet engagement with the blood vessel wall is predominantly mediated by GPVI and GPIb-IX-V; however, the platelet surface possesses receptors that can engage matrix proteins. Additional involvement of these other adhesion proteins, including integrins α2β1, α5β1, and α6β1, which bind collagen, fibronectin, and laminin, respectively, and αIIbβ3 that binds VWF and fibrinogen, among others, help to stabilize the initial attachment and facilitate platelet recruitment and thrombus growth. Platelet activation occurs following agonist binding to GPIb-IX-V and GPVI, integrin αIIbβ3, FcγRIIa, and the G protein-coupled receptors for serotonin (5-HT2A), ADP (P2Y1/12), epinephrine (α2A adrenergic receptor), TxA2 (TP), and thrombin (PAR1).
Abbreviations: ADP, adenosine diphosphate; VWF, von Willebrand factor; GP, glycoprotein.
