Abstract
Metastases to orbit occur rarely but are the most common form of malignant orbital tumors. Usually the orbital metastases occur in disseminated disease. Very rarely orbital metastases can be the presenting feature of systemic malignancy. We report here a case with orbital metastases as the presenting feature of lung malignancy and describe the utility of FDG PET/CT as one-stop-shop imaging modality in this setting.
Keywords: FDG PET/CT, Orbital metastases, Lung carcinoma
Introduction
Orbital metastases, although the most common form of malignant orbital tumors, are rarely encountered in the clinical practice [1]. Usually orbital metastases occur in disseminated disease. Rarely, however, orbital metastasis can be the presenting feature of systemic malignancy. Extensive work-up using various imaging modalities such as contrast-enhanced computed tomography (CeCT) of chest and abdomen and skeletal scintigraphy is required to diagnose the primary cause and establish the disease burden. FDG PET/CT is able to image the entire body in one session and therefore can be useful in identifying the primary tumor and demonstrating total disease burden in these cases. We report here a case of lung adenocarcinoma presenting as an orbital metastasis and usefulness of FDG PET/CT for diagnosing the primary malignancy and demonstrating the disease burden.
Case Report
A 60-year-old female presented with diplopia and pain in the left eye for a period of 1 month. Magnetic resonance imaging (MRI) was performed with both T1 and T2 sequences, which revealed a relatively well defined mass lesion in the orbital cone of the left eye. The mass was homogenous and hypointense on T1 sequences and hyperintense on T2 sequences (Fig. 1). The differential diagnosis was a benign tumor of the orbit or a metastatic lesion. However the patient did not have any systemic symptoms or signs on clinical examination suggestive of malignancy. Excision biopsy was performed keeping in mind the high probability of a benign tumor, but histopathological examination of the excised mass revealed metastatic adenocarcinoma. Subsequently the patient was subjected to FDG PET/CT for diagnosis of the occult primary tumor.
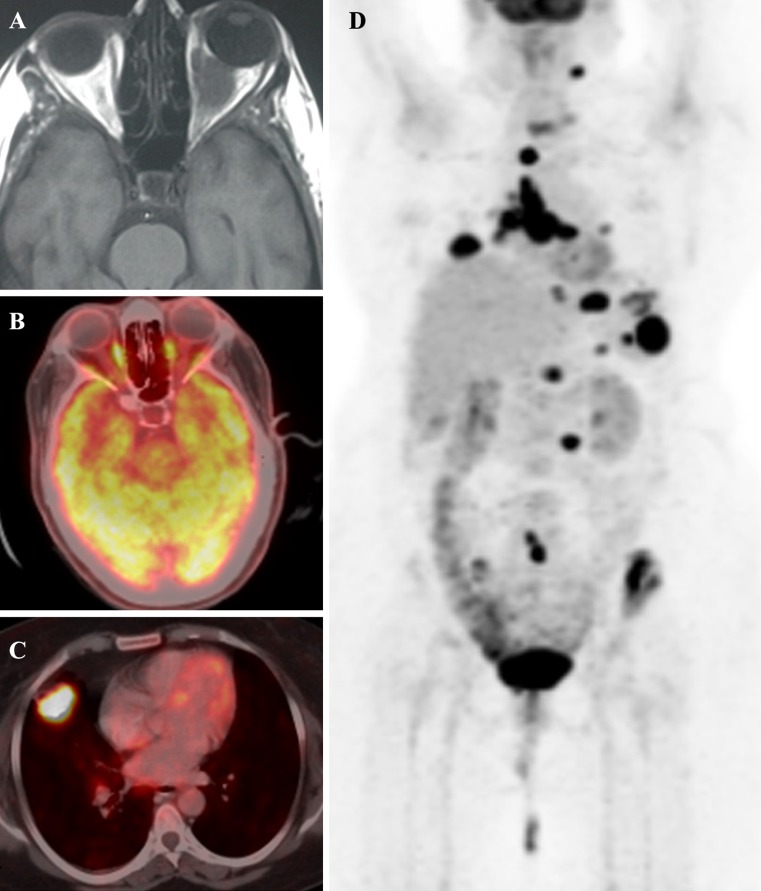
Fig. 1a–d.
Transaxial T1 sequence. a Magnetic resonance image showing a hypointense, homogenous relatively well-defined intraconal mass lesion in the left orbit. b Transaxial FDG PET/CT images done post excision of mass do not show any residual disease in the orbit. c Transaxial FDG PET/CT images showing an intensely FDG-avid (SUV = 18.5) soft tissue mass in the middle lobe of the right lung. d Maximum intensity projection image showing FDG-avid mediastinal, cervical, abdominal lymph nodal metastases, and metastatic lesions in the spleen, pelvic bones, T6, T12, and C6 vertebrae and left sixth rib
FDG PET/CT study was performed on a hybrid PET/CT scanner 60 min after intravenous injection of FDG. Scan findings revealed intense FDG uptake (SUV = 18.5) in a soft tissue mass in the middle lobe of the right lung (Fig. 1). In addition, intense FDG uptake was also noted in the bilateral mediastinal, cervical, and abdominal lymph nodes and in a hypodense lesion in the spleen and wall of stomach. Multiple mixed lytic and sclerotic bone metastases with intense FDG uptake were also seen in the pelvic bones and T6, T12, C6 vertebrae and left sixth rib. A provisional diagnosis of primary malignancy in the lung with widespread metastases was made based on FDG PET/CT findings. Subsequently CT-guided FNAC of the lung mass revealed adenocarcinoma.
Discussion
Metastases to the orbit are rare events in clinical practice. Presentation of a systemic malignancy as orbital metastasis is still rarer. Clinical symptoms of orbital metastases are usually due to mass effect causing pain or restriction of eye movements leading to diplopia, exophthalmos, etc. [1, 2]. Orbital metastases are usually hematogenously spread and are associated with disseminated disease rather than being an isolated metastatic site. Primary tumors that present as orbital metastasis include breast, lung, carcinoid, and melanoma, with breast and lung being the most common sites [2–6]. Provisional diagnosis of the primary site by imaging is important for guiding biopsy to determine the primary malignancy, as chemotherapy regimens might differ based on primary site. Also, in the case of breast malignancies, hormone therapy can be of use in disseminated disease. Work up of these patients routinely includes chest X ray, CeCT of the abdomen and thorax, and whole body bone scans to determine the primary malignancy and establish the total extent of disease. FDG PET/CT, as a whole body imaging modality, can be useful in detecting the primary site and in defining the total extent of disseminated disease. Advantages of FDG PET/CT in this kind of case are that the whole body is imaged in one session and with high sensitivity. The use of FDG PET/CT has been widely evaluated for detecting the primary malignancy in both cervical and extracervical carcinoma of unknown primary site [7, 8]. We have previously reported use of FDG PET/CT in patients with choroidal metastases [9], and this case demonstrates the usefulness of FDG PET/CT in diagnosing primary malignancy and estimating disease burden in a lung cancer patient with orbital metastasis as the presenting feature.
References
- 1.Shields JA, Shields CL, Brotman HK, Carvalho C, Perez N, Eagle RC, Jr, et al. Cancer metastatic to the orbit: the 2000 Robert M. Curts Lecture. Ophthal Plast Reconstr Surg. 2001;17:346–54. doi: 10.1097/00002341-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opin Ophthalmol. 2007;18:405–13. doi: 10.1097/ICU.0b013e3282c5077c. [DOI] [PubMed] [Google Scholar]
- 3.Zografos L, Ducrey N, Beati D, Schalenbourg A, Spahn B, Balmer A, et al. Metastatic melanoma in the eye and orbit. Ophthalmology. 2003;110:2245–56. doi: 10.1016/j.ophtha.2003.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Dieing A, Schulz CO, Schmid P, Roever AC, Lehenbauer-Dehm S, Jehn C, et al. Orbital metastases in breast cancer: report of two cases and review of the literature. J Cancer Res Clin Oncol. 2004;130:745–48. doi: 10.1007/s00432-004-0606-3. [DOI] [PubMed] [Google Scholar]
- 5.Macedo JE, Machado M, Araujo A, Angélico V, Lopes JM. Orbital metastasis as a rare form of clinical presentation of nonsmall cell lung cancer. J Thorac Oncol. 2007;2:166–67. doi: 10.1097/JTO.0b013e318031b633. [DOI] [PubMed] [Google Scholar]
- 6.Mehta JS, Abou-Rayyah Y, Rose GE. Orbital carcinoid metastases. Ophthalmology. 2006;113:466–72. doi: 10.1016/j.ophtha.2005.10.051. [DOI] [PubMed] [Google Scholar]
- 7.Deron PB, Bonte KM, Vermeersch HF, Van de Wiele C. Lymph node metastasis of squamous cell carcinoma from an unknown primary in the upper and middle neck: impact of (18) F-fluorodeoxyglucose positron emission tomography/computed tomography. Cancer Biother Radiopharm. 2011;26:331–4. doi: 10.1089/cbr.2010.0918. [DOI] [PubMed] [Google Scholar]
- 8.Moller AK, Loft A, Berthelsen AK. Damgaard Pedersen K, Graff J, Christensen CB et al. 18 F-FDG PET/CT as a diagnostic tool in patients with extracervical carcinoma of unknown primary site: a literature review. Oncologist. 2011;16:445–51. doi: 10.1634/theoncologist.2010-0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manohar K, Mittal BR, Kulkarni P, Singh N, Bhattacharya A, Gupta A. Usefulness of F-18 FDG PET/CT as one stop shop imaging modality for diagnosis of occult primary and estimation of disease burden in patients with intra-ocular masses. Clin Nucl Med [In press]. [DOI] [PubMed]