Abstract
Background
Few studies have examined residents' perspectives on the adequacy of women's health (WH) training in internal medicine (IM). This study sought residents' opinions regarding comfort level managing 13 core WH topics, their perceived adequacy of training in these areas, and the frequency with which they managed each topic. The association between reported comfort level and perceived adequacy of training and management frequency was also assessed.
Methods
A 67-item questionnaire was administered from April to June 2009 to 100 (64%) of the 156 residents from the traditional, primary care, and IM-pediatrics residency programs at a single institution. Descriptive and correlation statistics were used to examine the relationships between self-reported comfort level, perceived adequacy of training opportunities, and frequency managing WH issues. Data was stratified by sex, IM program, and post-graduate year (PGY).
Results
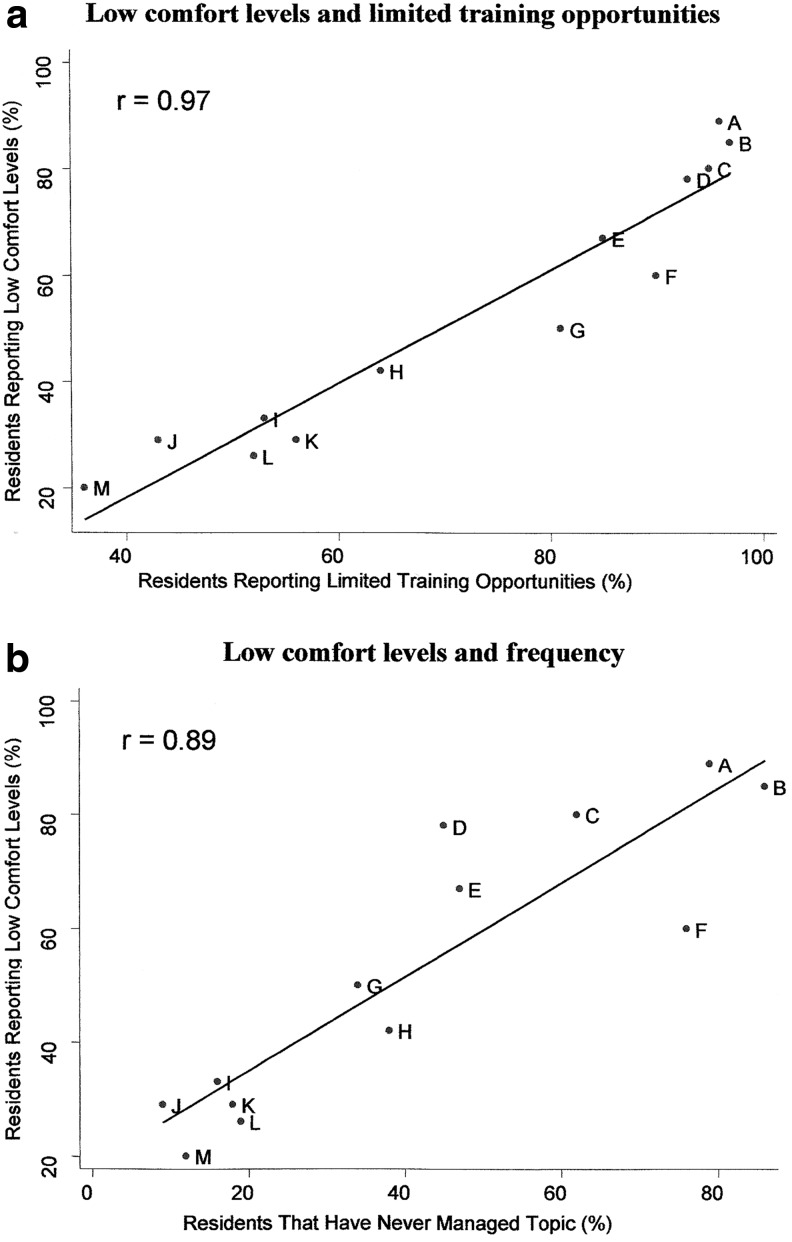
The majority of residents reported low comfort levels managing 7 of 13 topics. Over half of residents perceived limited training opportunities for 11 of 13 topics. With the exception of cardiovascular disease in women, greater than 75% of residents reported managing the 13 topics five or more times in the prior 6 months. Correlation analysis suggested a linear relationship between low comfort levels and limited training opportunities, and between low comfort levels and low frequency managing WH topics (r=0.97 and r=0.89, respectively). Stratified analyses by sex, IM program, and PGY showed no significant differences.
Conclusions
Key gaps remain in WH training. Our results emphasize the importance of reinforcing WH training with hands-on management opportunities. Understanding institution-specific strengths and weaknesses may help guide the development of targeted initiatives.
Introduction
Clinical competence in women's health (WH) is a recognized objective for graduating Internal Medicine (IM) physicians; however, studies evaluating residents in IM training programs have documented gaps in WH training.1–5 Additional studies among IM residency graduates,6,7 as well as surveys of program directors,8,9 have reported similar findings.
In the mid-1990s, the American Board of Internal Medicine (ABIM) outlined specific core competencies in WH,10 as well as recommendations for educators for training internists in WH.11 A decade later, in response to continued deficiencies in WH training, the Accreditation Council for Graduate Medical Education (ACGME) mandated that residency program continuity clinic panels comprise a minimum of 25% female patients.12 In addition to ensuring adequate numbers of female patients for training, some residency programs adopted program-specific approaches to improving WH training, including the creation of evidence-based WH didactic sessions,13 problem-based learning modules,14 special skills workshops,15 increased continuity clinic exposures,16,17 targeted interdisciplinary ambulatory experiences,18,19 and, at some institutions, formal WH tracks.20
Few studies have systematically surveyed residents regarding their perceived mastery of WH competencies4 or their perception of the adequacy of WH training opportunities.1,4 To help guide meaningful curricular change at a single institution in the Northeast United States, we assessed residents' self-reported comfort levels managing 13 core WH topics as a measure of their confidence and perceived competence in these areas. To identify strengths and weaknesses, we sought residents' opinions about the adequacy of existing training opportunities in each core WH topic. Finally, because prior studies have suggested a correlation between the frequency with which residents manage a clinical problem and their perceived competence for that problem, we also evaluated the self-reported frequency with which residents managed each WH topic.15,21
Materials and Methods
Study design and population
We conducted a cross-sectional questionnaire study with IM residents from a single institution in the Northeast United States from April 24–June 22, 2009. The institution's institutional review board reviewed and deemed the study exempt. Eligible participants included all categorical residents from the institution's three IM programs—traditional, primary care (emphasizing general internist training), and combined IM-pediatrics (leading to board eligibility in both internal medicine and pediatrics).
Questionnaire
The study questionnaire consisted of 67 items divided into six sections. The first three sections focused on a list of 13 core WH topic areas, selected based on ABIM-recommended core competencies in WH,10 as well as a review of WH curricula at existing IM residency programs across the United States.22 They included topics from the domain of obstetrics/gynecology, urology, and reproductive endocrinology that are also under the purview of IM, as well as preventive health topics in WH. Section 1 asked residents to rate their comfort level managing the 13 WH topics on an ordinal scale of 1 to 4 (1=not comfortable, 2=somewhat comfortable, 3=comfortable, 4=very comfortable). Section 2 asked residents to enumerate the number of times they had managed each WH topic during the last 6 months. Section 3 asked residents to rate on a three-point scale the adequacy of opportunities to develop their knowledge base and clinical skills in each WH topic (1=not adequate, 2=somewhat adequate, 3=adequate).
The next segment of the questionnaire gave residents the opportunity to consider potential clinical elective and scholarly training opportunities in WH that would augment existing didactic and clinical activities. Specifically, section 4 asked residents to group a list of 19 potential clinical elective opportunities, modeled after elective offerings at existing WH programs,22 by relative importance to their overall IM training experience using a three-point scale (1=not important, 2=somewhat important, 3=very important/should be part of core curriculum). Section V assessed residents' interest in additional WH scholarly training opportunities and asked them to specify interest in one or more of the following activities: a WH Journal club, dedicated WH conferences, a formal didactic curriculum/directed readings, a mentored research project, leadership training opportunities, and a WH policy seminar. Both section 4 and section 5 allowed residents to write in additional desired experiences not listed. Finally, section 6 requested information about the participant's sex, IM program, and post-graduate year (PGY).
We distributed the preliminary version of the questionnaire to three residents and used cognitive interviewing methods to assess the instrument for ease of use, clarity of questions, and consistency of answers.23 Two faculty members reviewed the questionnaire as well to comment on the appropriateness and scope of the topic list and training opportunities presented. We made minor changes to the final questionnaire based on those comments.
Data collection
The questionnaire contained no personal identifiers, and took approximately 5 minutes to complete either online or on paper. We sent all IM residents an initial electronic invitation to participate in the questionnaire at the beginning of the study period and sent weekly reminders throughout that period. Residents also received paper copies of the questionnaire in their mailboxes and had access to paper questionnaires during resident report and noontime teaching conferences. Residents could also obtain paper copies of the questionnaire at four designated locations in the hospital (outside certain educational offices, continuity clinic areas, or faculty offices) and could leave completed forms in designated collection envelopes at those same locations. Recruitment took place over the course of 2 consecutive months to ensure that residents not on service during one block could participate during the following block.
Statistical analysis
Descriptive statistics were performed to generate simple frequencies and proportions. We operationalized perceived comfort level among residents as low comfort (“not comfortable” and “somewhat comfortable”) or high comfort (“comfortable” and “very comfortable”). Perceived adequacy of training opportunities for each WH topic was categorized as limited (“not adequate” and “somewhat adequate”) or adequate (“adequate”). We grouped resident responses for frequency managing each WH topic into those who had never managed a given topic in the last 6 months, those who had managed the topic one to five times in the last 6 months, or those who managed the topic more than five times in the last 6 months.
We classified residents' ratings of potential clinical elective opportunities as not important, somewhat important, and very important/should be part of core curriculum based upon the most commonly selected response for each topic (i.e., the mode). We also calculated the proportion of residents who reported interest in additional scholarly opportunities.
We stratified perceived comfort level by resident sex, IM program, and PGY using Chi-squared and Fisher's exact tests. Stratified analyses compared residents at the beginning of training (PGY1) with those completing training (PGY3 and PGY4). We also assessed for correlation between low comfort and limited training opportunities, as well as low comfort and never managing a topic in the last 6 months using Spearman's rank coefficients. All analyses were carried out using Intercooled Stata 8 (Stata Corporation).
Results
Characteristics of participants
A total of 100 out of 156 residents completed questionnaires (64% participation rate). At least half of the residents in each PGY completed the questionnaire. A larger proportion of female residents responded (69%) than male residents (59%) with the greatest participation among PGY2 residents (73%). Participation varied by IM program from 48% in the primary care program to 71% in the traditional program (Table 1). However, the overall proportion of respondents by sex, PGY, and IM program was not statistically different from the distribution of total IM residents in each of those groups.
Table 1.
Characteristics of Study Participants (n=100)
| Characteristic | Respondents (% of total) | Total number of residents | p |
|---|---|---|---|
| Total | |||
| 100 (64) | 156 | ||
| Sex | |||
| Female | 52 (69) | 75 | 0.54 |
| Male | 48 (59) | 81 | 0.54 |
| Post-graduate year | |||
| 1 | 36 (66) | 55 | 0.90 |
| 2 | 35 (73) | 48 | 0.48 |
| 3 | 27 (55) | 49 | 0.45 |
| 4 | 2 (50) | 4 | 0.77 |
| Internal medicine program | |||
| Traditional | 70 (71) | 98 | 0.24 |
| Primary care | 20 (48) | 42 | 0.21 |
| Medicine-pediatrics | 10 (63) | 16 | 0.95 |
Comfort level, perceived adequacy of training opportunities, and frequency managing core WH topics
The majority of residents reported low comfort levels managing 7 of 13 topics (Table 2). The largest proportion of residents reported low comfort levels managing topics traditionally in the domains of obstetrics/gynecology and urology, followed by topics in reproductive endocrinology. Fewer residents reported low comfort levels managing topics associated with preventive health screening, such as the breast exam and evaluation of a breast mass, the pelvic exam and Pap smear interpretation, and osteoporosis screening and management. Only 20% of residents reported low comfort levels managing cardiovascular disease risk and prevention in women, indicating high comfort levels among residents managing this topic.
Table 2.
Proportion of Residents Reporting Low Comfort Levels (n=100), Limited Training Opportunities (n=99), and Categories of Frequency (n=100) Managing 13 Core Women's Health Topics
| Frequency in past 6 months (%) | |||||
|---|---|---|---|---|---|
| Low comfort level managing topic (%) | Limited training opportunities (%) | Never | 1–5 times | >5 times | |
| Obstetrics/gynecology and urology topics | |||||
| Medical complications of pregnancy | 89 | 96 | 79 | 20 | 1 |
| Female sexual response & dysfunction | 85 | 97 | 86 | 13 | 1 |
| Preconceptual counseling (including EC) | 80 | 95 | 62 | 31 | 7 |
| Urinary incontinence & pelvic floor dysfunction | 78 | 93 | 45 | 52 | 3 |
| Reproductive endocrinology topics | |||||
| Amenorrhea & abnormal vaginal bleeding | 67 | 85 | 47 | 50 | 3 |
| Evaluation of galactorrhea | 60 | 90 | 76 | 24 | 0 |
| Menopausal symptoms | 50 | 81 | 34 | 63 | 3 |
| Preventive health topics | |||||
| Domestic violence screening & intervention | 42 | 64 | 38 | 44 | 18 |
| Breast exam & evaluation of breast mass | 33 | 53 | 16 | 75 | 9 |
| Pelvic exam & pap smear interpretation | 29 | 43 | 9 | 69 | 22 |
| Osteoporosis screening & management | 29 | 56 | 18 | 65 | 18 |
| Vaginal discharge & STIs | 26 | 52 | 19 | 71 | 10 |
| Cardiovascular disease risk & prevention | 20 | 36 | 12 | 42 | 46 |
EC, emergency contraception; STI, sexually transmitted infection.
More than half of residents perceived limited training opportunities for 11 of 13 WH topics. The two exceptions included the pelvic exam and Pap smear interpretation, and cardiovascular disease risk and prevention in women. Residents also reported managing most WH topics infrequently, with cardiovascular disease risk and prevention in women being the only topic that over 25% of residents had managed more than five times in the last 6 months (Table 2).
Stratifying comfort levels by sex and IM program yielded no statistically significant differences with the exception of higher comfort levels reported among primary care residents managing domestic violence screening and intervention. Similarly, when we compared comfort levels among residents in their first year of training (PGY1) to those completing training (PGY3 and 4), we found no statistically significant difference. To investigate this finding further, we compared perceived opportunities for training, as well as frequency managing the 13 core WH topics, among PGY1 residents compared with PGY3 and 4 residents. PGY3 and 4 residents perceived more training opportunities than PGY1 residents in reproductive endocrinology and preventive health topics. However, their reported frequency managing these topics in the past 6 months was not statistically significantly different from that of PGY1 residents. The one exception was an increased frequency managing osteoporosis (p=0.01) among PGY3 and PGY4 residents.
Correlation of comfort levels with training opportunities and frequency managing core WH topics
We found high correlation between the proportion of residents reporting low comfort levels and the proportion who perceived limited training opportunities for each WH topic (r=0.97, Fig. 1a). Similarly, when we examined the relationship between low comfort levels and the proportion of residents who had never managed each WH topic in the last 6 months, correlation analysis again suggested a linear relationship between the two variables (r=0.89, Fig. 1b). Topics for which residents perceived more training opportunities or managed more frequently, such as cardiovascular disease risk and prevention in women, received high comfort level ratings. Conversely, topics for which residents perceived limited training opportunities or managed rarely, such as female sexual response and dysfunction and preconceptual counseling, received low comfort level ratings.
FIG. 1.
Correlation of low comfort levels with limited training opportunities (a) and frequency (b). A, medical complications of pregnancy; B, female sexual response and dysfunction; C, preconceptual counseling (including emergency contraception); D, urinary incontinence and pelvic floor dysfunction; E, amenorrhea and abnormal vaginal bleeding; F, evaluation of galactorrhea; G, menopausal symptoms; H, domestic violence screening and intervention; I, breast exam and evaluation of breast mass; J, pelvic exam and pap smear interpretation; K, osteoporosis screening and management; L, vaginal discharge and sexually transmitted infections; M, cardiovascular disease risk and prevention.
Potential clinical elective and scholarly training opportunities
Among the 19 potential clinical elective opportunities that residents prioritized, residents designated 10 of the elective opportunities as very important/should be part of the core IM curriculum, and categorized the remaining nine elective opportunities as somewhat important (Table 3). In general, potential elective opportunities deemed very important by residents tended to correspond with the WH topics for which residents reported high comfort levels, such as “Women and Cardiovascular Disease” and “STIs and HIV among Women.” Other potential clinical electives proposed by residents in the open-ended response section included irritable bowel syndrome/constipation in women, lesbian health, weight disorders, rheumatologic disease in women, female hormone replacement, and lactation counseling.
Table 3.
Potential Clinical Elective Opportunities as Prioritized by Residents (n=100)
| Very important | % Residents | Somewhat important | % Residents |
|---|---|---|---|
| Women and cardiovascular disease | 94 | Adolescent medicine | 55 |
| STIs & HIV among women | 88 | Sports injuries among women | 55 |
| Care of menopausal women | 82 | Global women's health | 55 |
| Bone metabolism | 77 | Female sexual response and dysfunction | 55 |
| Domestic violence/battered women's shelter | 66 | Health of immigrant women | 53 |
| Breast disorders | 63 | Urinary incontinence & pelvic floor dysfunction | 51 |
| Mental health among women | 62 | Medical complications of pregnancy | 50 |
| Management of abnormal pap test/colposcopy | 61 | Reproductive endocrinology | 47 |
| Routine gynecologic care | 59 | Preconceptual care | 43 |
| Conception counseling | 49 |
HIV, human immunodeficiency virus; STI, sexually transmitted infection.
In addition to the potential clinical elective experiences mentioned above, 82 of the 100 residents who responded to the survey indicated desire to participate in additional scholarly opportunities. Fifty-seven percent of those expressed interested in a formal didactic WH curriculum or directed readings, and almost half indicated interest in a monthly WH conference (47%) or journal club (46%). A subgroup of residents sought more focused opportunities, such as a WH policy seminar (16%), leadership training opportunities (8%), or mentored research (4%).
Discussion
In this survey of residents from an internal medicine training program in the Northeast United States, residents reported particularly low comfort levels managing topics traditionally in the domains of obstetrics/gynecology, urology, and reproductive endocrinology that are also considered core competencies in IM. By comparison, WH topics associated with preventive health received the highest comfort level ratings from residents, in particular, cardiovascular disease risk and prevention in women. Surprisingly, our study found no differences in reported comfort levels when stratified by sex, IM program, or PGY, and when we compared the frequency with which residents managed WH topics in the last 6 months, PGY3 and PGY4 residents only reported increased frequency managing osteoporosis compared with PGY1 residents. Our study also found a positive correlation between reported comfort levels and perceived adequacy of training and between comfort levels and frequency managing topics in WH.
These findings are consistent with prior studies reporting lack of confidence and knowledge among IM residents in the realm of caring for women of reproductive age, and demonstrate a persistent deficit.1,2,5 Residents in our study also reported low comfort levels managing the female sexual response and dysfunction, urinary incontinence and pelvic floor dysfunction, and menopausal symptoms. The fact that residents reported greater comfort levels with WH topics related to preventive health is encouraging, and may reflect established protocols in outpatient clinic settings for screening of these conditions, leading to more opportunities for training and management. Notably, residents consistently ranked cardiovascular disease among women as the most comfortable, most adequately taught, and most frequently managed topic, which may reflect the relative emphasis of cardiovascular health in internal medicine training at this institution and therefore, increased exposure in both inpatient and outpatient settings. Our findings also support previous studies from other specialties that have demonstrated a correlation between resident comfort levels and frequency managing topics in medicine, underscoring the importance of direct and reinforced clinical exposure during residency training.24,25 Perhaps it is not surprising then that we found no differences in comfort levels between residents at the beginning of their training compared with those completing training, as there was no increase in frequency managing 12 of 13 WH topics between the two groups.
In light of the sheer volume of training objectives outlined for IM residency curricula, programs should take a directed approach towards maximizing training opportunities for residents in WH. Our results emphasize the importance of repeated exposure to hands-on management opportunities in order to reinforce resident learning and improve comfort levels. Because many WH topics are classically encountered in the outpatient clinic setting, the 2009 ACGME mandate that one third of residency training take place in the ambulatory setting may provide a unique opportunity to incorporate targeted WH training opportunities into residency curricula.26 Our findings also suggest that recognizing program-specific strengths (such as the emphasis on cardiovascular health at this institution) or preexisting infrastructure (such as preventive health screening protocols) can help generate important and sustainable training opportunities. Furthermore, identifying institutional resources, such as particularly effective faculty from other departments, leaders in women's health, ambulatory clinics from other disciplines (e.g., breast clinic, ambulatory gynecology clinic, mental health clinic), outside of the IM department can lead to the creation of valuable interdisciplinary opportunities for resident training.
Our study also identified a large subgroup of residents with scholarly interests in WH beyond the core competencies. This included a significant number of residents who were interested in curricular additions such as a formal didactic WH curriculum, directed readings, a monthly WH conference, or a journal club. A small group of residents expressed interest in more focused training opportunities such as a WH policy seminar or mentored research, suggesting potential career aspirations related to WH. Residency programs should therefore strive to develop training opportunities that can meet both fundamental WH learning objectives for all residents, as well as additional mechanisms aimed at fostering career development in WH. While creating a dedicated WH track is not necessarily practical or feasible at all institutions, creating a journal club, designing WH electives or pairing interested residents with clinical or research mentors who have expertise in WH may provide important first steps. In our study, clinical elective opportunities deemed highly important by residents tended to correspond with the WH topics for which residents reported high comfort levels. Finally, strong teaching in WH requires that IM faculty members themselves feel confident in their knowledge base in WH, which is often not the case.27,28 Investing in faculty development in WH offers another important indirect means of improving the quality of WH training opportunities for residents.
We acknowledge certain limitations in our study. Only two-thirds of residents participated in this study, which could lead to respondent bias. However, those responding are likely to be more invested in WH than non-responders, and may have been more discriminating in their answers. In addition, because our study represents a single institution, it may not be generalizable to other training programs. Furthermore, we only selected 13 core WH topics for our assessments. However, we selected topics based upon careful review of existing recommendations for WH training, with the aim of identifying a group of relevant and practical topics as opposed to being exhaustive. Finally, we present correlational data and therefore cannot draw conclusions about causality or directionality between variables.
Conclusions
Although core competencies exist for WH training in IM, our study highlights that important gaps still remain, especially for topics in the realm of obstetrics/gynecology, urology, and reproductive endocrinology that are also under the purview of IM. These gaps may exist in part due to lack of reinforced training, highlighting the importance of repeated exposures to management opportunities that build upon and solidify prior learning experiences. Understanding program-specific strengths and weaknesses, and maximizing interdisciplinary institutional resources, can help guide the development of targeted and effective WH training opportunities for residents. Acknowledging the diverse career goals of residents in IM will allow for creation of fundamental WH learning opportunities as well as more directed opportunities for career development. Finally, investing in faculty development in WH plays a critical role in ensuring high quality and sustainable training opportunities for residents in this field.
Acknowledgments
The authors would like to acknowledge Stephen Huot, MD, PhD, Associate Chair for Education/Academic Affairs, Department of Internal Medicine, Yale School of Medicine. Funding for this project was provided by the Department of Internal Medicine, Yale School of Medicine; this study was reviewed and exempt by the Yale Human Investigations Committee.
Disclosure Statement
The authors of this manuscript have no personal or financial conflicts of interest to disclose.
References
- 1.Coodley MK. Coodley GO. Levinson W. Rosenerg MR. Dull VT. Internal medicine training in ambulatory gynecology: A house staff survey. Arch Intern Med. 1993;153:2588–2592. [PubMed] [Google Scholar]
- 2.Conway R. Hu TC. Mason E. Mueller C. Are primary care residents adequately prepared to care for women of reproductive age? Fam Plann Perspect. 1995;27:66–70. [PubMed] [Google Scholar]
- 3.Pursley HG. Kwolek DS. Griffith CH. Wilson JF. Women's health issues and residents' knowledge. J Ky Med Assoc. 2002;100:238–244. [PubMed] [Google Scholar]
- 4.Orsetti KE. Frohna JG. Gruppen LD. Del Valle J. Impact of a veteran affairs continuity clinic on resident competencies in women's health. J Gen Intern Med. 2003;18:419–422. doi: 10.1046/j.1525-1497.2003.20733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lohr PA. Schwarz EB. Gladstein JE. Nelson AL. Provision of contraceptive counseling by internal medicine residents. J Women's Health. 2009;18:127–131. doi: 10.1089/jwh.2008.0809. [DOI] [PubMed] [Google Scholar]
- 6.Coodley GO. Elliot DL. Goldberg L. Internal medicine training in ambulatory gynecology. J Gen Intern Med. 1992;7:636–639. doi: 10.1007/BF02599205. [DOI] [PubMed] [Google Scholar]
- 7.Wayne DB. DaRosa DA. Evaluating and enhancing a women's health curriculum in an internal medicine residency program. J Gen Intern Med. 2004;19:754–759. doi: 10.1111/j.1525-1497.2004.30017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Starpoli CA. Moulton AW. Cyr MG. Primary care internal medicine training and women's health. J Gen Intern Med. 1997;12:129–131. doi: 10.1046/j.1525-1497.1997.00019.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spencer AL. Kern LM. Primary care program directors' perceptions of women's health education: A gap in graduate medical education persists. J Women's Health. 2008;17:549–556. doi: 10.1089/jwh.2007.0473. [DOI] [PubMed] [Google Scholar]
- 10.Cassel C. Blank L. Braunstein G. Burke W. Fryhofer SA. Pinn V. What internists need to know: Core competencies in women's health. American Journal of Medicine. 1997;102:507–12. doi: 10.1016/s0002-9343(97)00227-1. [DOI] [PubMed] [Google Scholar]
- 11.Day SC. Cassel CK. Kimball HR. Training internists in women's health: recommendations for educators. Am J Med. 1996;100:375–379. doi: 10.1016/s0002-9343(97)89510-1. [DOI] [PubMed] [Google Scholar]
- 12.Accreditation Council for Graduate Medical Education. Program requirements for residency education in internal medicine, effective. Jul 1, 2007. http://www.acgme.org http://www.acgme.org
- 13.Pursley HG. Kwolek DS. A women's health track for internal medicine residents using evidence-based medicine. Academic Medicine. 2002;77(7):743–4. doi: 10.1097/00001888-200207000-00031. [DOI] [PubMed] [Google Scholar]
- 14.Spencer AL. McNeil M. Interdisciplinary curriculum to train internal medicine and obstetrics-gynecology residents in ambulatory women's health: Adapting problem-based learning to residency education. J Women's Health. 2009;18:1369–1375. doi: 10.1089/jwh.2008.1253. [DOI] [PubMed] [Google Scholar]
- 15.Watkins RS. Moran WP. Competency-based learning: The impact of targeted resident education and feedback on Pap smear adequacy rates. J Gen Intern Med. 2004;19:545–548. doi: 10.1111/j.1525-1497.2004.30150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haskell SG. Reisman AB. A novel program to increase the number of women patients seen by residents in a VA hospital. Acad Med. 2004;79(9):851–854. doi: 10.1097/00001888-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Conigliaro RL. An innovative program to provide adequate women's health education to residents with VA-based ambulatory care experiences. Teach Learn Med. 2007;19:148–153. doi: 10.1080/10401330701332896. [DOI] [PubMed] [Google Scholar]
- 18.Henrich JB. Chambers JT. Steiner JL. Development of an interdisciplinary women's health training model. Acad Med. 2003;78:877–884. doi: 10.1097/00001888-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Singh MK. Einstadter D. Lawrence R. A structured women's preventive health clinic for residents: A quality improvement project designed to meet training needs and improve cervical cancer screening rates. Qual Saf Health Care. 2010;19:e45. doi: 10.1136/qshc.2009.033274. [DOI] [PubMed] [Google Scholar]
- 20.Spencer AL. Bost JE. McNeil M. Do women's health internal medicine residency tracks make a difference? J Women's Health. 2007;16:1219–1223. doi: 10.1089/jwh.2006.0274. [DOI] [PubMed] [Google Scholar]
- 21.Chew RB. Chew LD. Bradley K. The association between number of Pap smears performed and self-reported confidence in an internal medicine residency. J Women's Health. 2006;15:928–933. doi: 10.1089/jwh.2006.15.928. [DOI] [PubMed] [Google Scholar]
- 22.Association of Academic Women's Health Programs. Directory of Residency and Fellowship Programs in interdisciplinary women's health. J Women's Health. 2010;19:1005–1043. doi: 10.1089/jwh.2010.DIR4. [DOI] [PubMed] [Google Scholar]
- 23.Willis G. Reducing survey error through research on the cognitive and decision processes in surveys. Short course presented at the Meeting of the American Statistical Association; Baltimore, Maryland. Aug 8–12;1999 . [Google Scholar]
- 24.Tang JW. Freed B. Baker T, et al. Internal Medicine residents' comfort with and frequency of providing dietary counseling to diabetic patients. J Gen Intern Med. 2009;24:1140–1143. doi: 10.1007/s11606-009-1084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy KM. Miller MP. Schmidt K. Sagy M. Pediatric residents experience a significant decline in their response capabilities to simulated life-threatening events as their training frequency in cardiopulmonary resuscitation decreases. Pediatr Crit Care Med. 2011 May 12;:e141–144. doi: 10.1097/PCC.0b013e3181f3a0d1. [DOI] [PubMed] [Google Scholar]
- 26.Accreditation Council for Graduate Medical Education Program Requirements for Graduate Medical Education in Internal Medicine, effective July 1. 2009. http://www.acgme.org http://www.acgme.org
- 27.Dixon JG. Bognar BA. Keyserling TC. DuPre CT. Xie SX. Wickstrom GC. Kolar MM. Teaching women's health skills: Confidence, attitudes, and practice patterns of academic generalist physicians. J Gen Intern Med. 2003;18:411–418. doi: 10.1046/j.1525-1497.2003.10511.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wickstrom GC. Kelley DK. Keyserling TC, et al. Confidence of academic general internists and family physicians to teach ambulatory practices. J Gen Inten Med. 2000;15:353–360. doi: 10.1046/j.1525-1497.2000.04109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]