Figure 2.
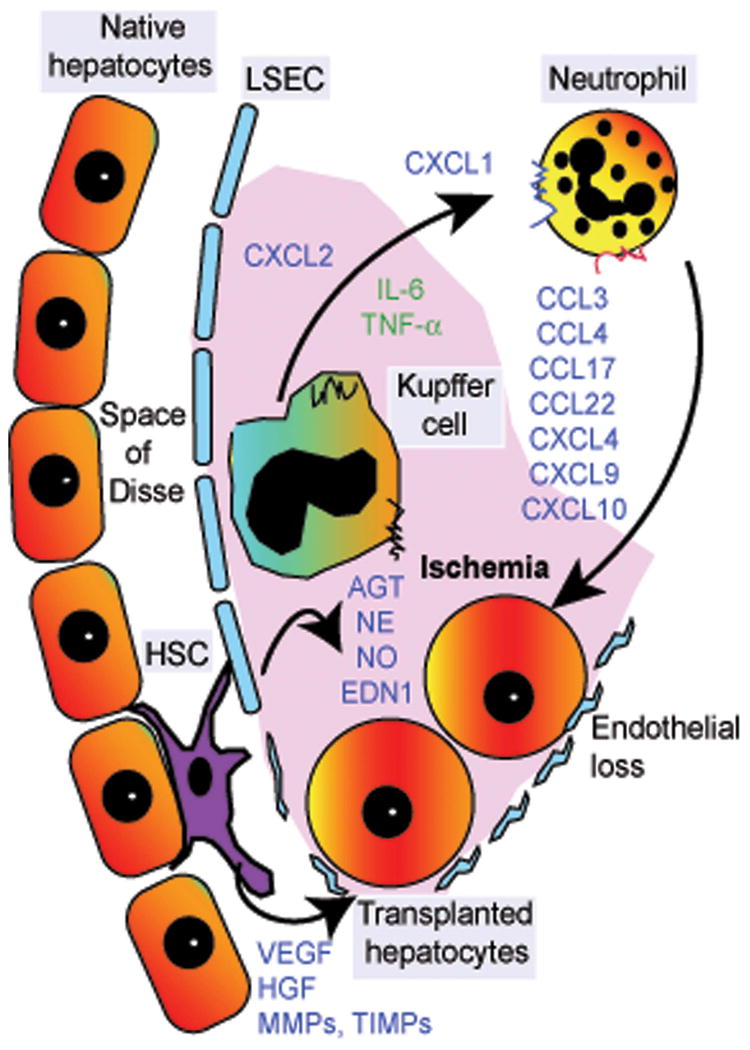
Schematic of early hepatic sinusoidal events following cell transplantation. Arrival of transplanted hepatocytes in hepatic sinusoids triggers ischemia-type processes, which lead to the release of locally acting vascular substances (e.g., angiotensin, norepinephrine, nitrous oxide, endothelin-1) as well as activation of neutrophils and Kupffer cells. This, in turn, leads to the release of multiple cytokines, chemokines, and receptors, including those with cytotoxic properties, which leads to transplanted cell clearance. Simultaneously, ischemic damage to liver sinusoidal endothelial cells (LSECs), along with cell–cell interactions resulting from adhesion of transplanted hepatocytes to LSECs, advances the entry of transplanted cells into the space of Disse. Activation of hepatic stellate cells (HSCs) causes expression of matrix-type metalloproteinases (MMPs), tissue inhibitors of MMPs (TIMPs), etc., which facilitates tissue remodeling during the integration of transplanted cells into the liver parenchyma. Release of additional substances (e.g., VEGF, HGF) from native hepatocytes, LSECs, and HSCs also assists transplanted cell engraftment. These mechanisms provide opportunities for drug-based approaches to control deleterious inflammatory events and to promote beneficial cell engraftment processes. The mechanisms are different in the setting of normal liver and are less well defined in the setting of chronic liver disease, including WD.
