Abstract
Acute kidney injury (AKI) is a common and serious problem affecting millions and causing death and disability for many. In 2012, Kidney Disease: Improving Global Outcomes completed the first ever international multidisciplinary clinical practice guideline for AKI. The guideline is based on evidence review and appraisal, and covers AKI definition, risk assessment, evaluation, prevention, and treatment. Two topics, contrast-induced AKI and management of renal replacement therapy, deserve special attention because of the frequency in which they are encountered and the availability of evidence. Recommendations are based on systematic reviews of relevant trials. Appraisal of the quality of the evidence and the strength of recommendations followed the Grading of Recommendations Assessment, Development and Evaluation approach. Limitations of the evidence are discussed and a detailed rationale for each recommendation is provided. This review is an abridged version of the guideline and provides additional rationale and commentary for those recommendation statements that most directly impact the practice of critical care.
Introduction
While the last few years have witnessed a massive increase in new information concerning acute kidney injury (AKI), two areas have experienced much of this growth: contrast-induced acute kidney injury (CI-AKI) and renal replacement therapy (RRT). In early 2012, Kidney Disease: Improving Global Outcomes (KDIGO), a nonprofit foundation, published the first international, interdisciplinary clinical practice guideline on AKI [1], which is available in its entirety on the KDIGO website [2]. We present here a shortened version of the guideline covering CI-AKI and management of RRT for AKI, and provide additional rationale and commentary for those recommendation statements that most directly impact the practice of critical care.
Methods
A complete and detailed description of the methods can been found online [3]. The KDIGO Co-Chairs appointed two Co-Chairs of the Work Group, who then assembled experts in several domains (nephrology, critical care medicine, internal medicine, pediatrics, cardiology, radiology, infectious diseases, and epidemiology). The Evidence Review Team at Tufts Medical Center, Boston, MA, USA consisted of physician-methodologists with expertise in nephrology and internal medicine, and research associates and assistants.
The evidence selection, appraisal, and presentation have followed methodology previously described in KDIGO clinical practice guidelines [4]. Work Group members reviewed all retrieved relevant articles, data extraction forms, summary tables, and evidence profiles for accuracy and completeness. The four major topic areas of interest for AKI included: definition and classification; prevention; pharmacologic treatment; and RRT. Populations of interest were those at risk for AKI (including those after intravascular contrast-media exposure, aminoglycosides, and amphotericin), and patients with sepsis or trauma or those receiving critical care or undergoing cardiothoracic surgery. We excluded studies on AKI from rhabdomyolysis, specific infections, and poisoning or drug overdose. Overall, we screened 18,385 citations.
Outcome selection, judgments, values, and preferences
We limited outcomes to those important for decision-making, including development of AKI, need for or dependence on RRT, and all-cause mortality. When weighting the evidence across different outcomes, we selected as the crucial outcome that which weighed most heavily in the assessment of the overall quality of evidence. Values and preferences articulated by the Work Group included: a desire to be inclusive in terms of meeting criteria for AKI; a progressive approach to risk and cost such that, as severity increased, the group put greater value on possible effectiveness of strategies, but maintained high value for avoidance of harm; and intent to guide practice but not limit future research.
Grading the quality of evidence and the strength of recommendations
The grading approach followed in this guideline and the wording of each recommendation are adopted from the Grading of Recommendations Assessment, Development and Evaluation system [4,5]. The strength of each recommendation is rated as level 1 (strong) or level 2 (weak or discretionary). In addition, each statement is assigned a grade for the quality of the supporting evidence: A (high), B (moderate), C (low), or D (very low). Furthermore, on topics that cannot be subjected to systematic evidence review, the Work Group issued statements that are not graded which hopefully will provide general guidance based on clinical experience.
The Grading of Recommendations Assessment, Development and Evaluation system is best suited to evaluate evidence on comparative effectiveness. Some of our most important guideline topics involve diagnosis and staging of AKI, and here the Work Group chose to provide ungraded statements. These statements are indirectly supported by evidence on risk relationships and resulted from unanimous consensus of the Work Group and should not be viewed as weaker than graded recommendations.
Recommendations and rationale
The Work Group developed 61 graded recommendation statements and 26 ungraded statements. The six major domains are: (A) definition and staging; (B) risk assessment; (C) evaluation and general management; (D) prevention and treatment; (E) CI-AKI; and (F) RRT for AKI. Domains (E) and (F) are presented here, while domains (A) through (D) are discussed in the preceding review.
E. Contrast-induced acute kidney injury
Classification and risk assessment
Pending the validation of future biomarkers that would allow a more straightforward comparison and integration of CI-AKI in the overall framework of AKI, we suggest that the same criteria using the changes in serum creatinine (SCr) concentrations and urine output be used as for the other forms of AKI. A CI-AKI Consensus Working Panel agreed that the risk of CI-AKI becomes clinically important when the baseline SCr concentration is ≥1.3 mg/dl (≥115 μmol/l) in men and ≥1.0 mg/dl (≥88.4 μmol/l) in women, equivalent to an estimated glomerular filtration rate <60 ml/minute per 1.73 m2 [6]. However, Bruce and colleagues showed that the incidence of true AKI became significant only between controls and contrast-media administered patients from a baseline SCr concentration >1.8 mg/dl (>159 μmol/l) onward [7]. The CI-AKI Consensus Working Panel recommended that precautions to reduce the risk should be implemented in patients with a baseline estimated glomerular filtration rate <60 ml/minute per 1.73 m2 [6]. In light of more recent information, this threshold could probably be lowered to 45 ml/minute per 1.73 m2. Table 1 provides a CI-AKI risk-scoring model for percutaneous coronary intervention.
Table 1.
Contrast-induced acute kidney injury risk-scoring model for percutaneous coronary intervention
| Risk factor | Integer score (calculated)a |
|---|---|
| Hypotension | 5 |
| Intra-aortic balloon pump | 5 |
| Congestive heart failure | 5 |
| Age >75 years | 4 |
| Anemia | 3 |
| Diabetes | 3 |
| Contrast-media volume | 1 per 100 ml |
| SCr >1.5 mg/dl (>132.6 μmol/l) or | 4 |
| eGFR <60 ml/minute per 1.73 m2 | 2 for 40 to 60 ml/minute per 1.73 m2, 4 for 20 to 39 ml/minute per 1.73 m2, 6 for <20 ml/minute per 1.73 m2 |
eGFR, estimated glomerular filtration rate; SCr, serum creatinine. Reprinted from [9] with permission from the American College of Cardiology Foundation. aLow risk, cumulative score <5; high risk, cumulative score >16.
In patients at increased risk for CI-AKI, the risks and benefits of iodinated contrast-media administration should be discussed with the radiologist. One should note that magnetic resonance imaging with gadolinium contrast is not a safe alternative for many patients with pre-existing renal dysfunction. New labeling describes the risk for nephrogenic systemic fibrosis following exposure to gadolinium in patients with a glomerular filtration rate <30 ml/minute per 1.73 m2 and in patients with AKI of any severity due to hepatorenal syndrome or in the perioperative liver transplantation period. Additional recommendations were recently proposed by Perazella [8] and were endorsed by the Work Group.
E1: Define and stage AKI after administration of intravascular contrast media as per Recommendations A1 and A2 (not graded)
E1.1: In individuals who develop changes in kidney function after administration of intravascular contrast media, evaluate for CI-AKI as well as for other possible causes of AKI (not graded)
E2: Assess the risk for CI-AKI and, in particular, screen for pre-existing impairment of kidney function in all patients who are considered for a procedure that requires intravascular (intravenous or intraarterial) administration of iodinated contrast medium (not graded)
Contrast type and volume
The correlation between the volume of contrast media administered and the risk of CI-AKI has been recognized [10]. A recent study by Nyman and colleagues in patients undergoing coronary angioplasty calculated the probability of CI-AKI (SCr rise >0.5 mg/dl (>44.2 μmol/l) or oliguria/anuria) at various estimated glomerular filtration rate levels based on grams of iodine/estimated glomerular filtration rate ratios of 1:2, 1:1, 2:1, and 3:1 [11]. At a ratio <1 the risk of CI-AKI was 3%, while it was 25% at a ratio ≥1. This study and other preliminary studies indicate that a ratio <1 may be relatively safe in a patient without multiple risk factors [11-13].
Both the review by Goldfarb and colleagues [14] and the meta-analysis from Barrett and Carlisle combining 24 randomized studies [15] suggest that the risk of CI-AKI is similarly low with high-osmolar and low-osmolar agents among otherwise stable patients with normal renal function. In contrast to high-osmolar contrast media, however, low-osmolar contrast media are less nephrotoxic in patients with pre-existing kidney function impairment.
Among low and iso-osmolar contrast, of eight studies comparing contrast media [16-23] some showed superiority of iso-osmolar contrast media (iodixanol) compared with iohexol [16] and iopromide [21]. There was no difference when iodixanol was compared with iopamidol [18,23], iopromide [17,19], and ioversal [22]. A recent meta-analysis [24] analyzed studies comparing iodixanol with low-osmolar contrast media. The pooled relative risk was 0.68 (95% confidence interval = 0.46 to 1.01; P = 0.06). Iodixanol is thus not associated with a significantly reduced risk of CI-AKI compared with the low-osmolar contrast media pooled together. In patients with decreased kidney function, however, iodixanol is associated with a reduced risk of CI-AKI compared with iohexol.
For iodixanol versus ioxaglate, two studies fulfilled our inclusion criteria; one study showed a superiority of iodixanol versus ioxaglate [25], but this was not confirmed in the study by Mehran and colleagues that found no difference between these two contrast agents [26]. Based on this evidence and the most recent meta-analysis of the studies comparing iso-osmolar versus low-osmolar contrast media [24], the Work Group found no evidence to recommend a preference for either type of agent.
E3: Consider alternative imaging methods in patients at increased risk for CI-AKI (not graded)
E4: Use the lowest possible dose of contrast medium in patients at risk for CI-AKI (not graded)
E5: We recommend using either iso-osmolar or low-osmolar iodinated contrast media, rather than high-osmolar iodinated contrast media, in patients at increased risk of CI-AKI (Grade 1B)
Volume expansion
Sodium bicarbonate solutions have been tested in the prevention of CI-AKI in comparison with isotonic saline, either with or without N-acetylcysteine (NAC). A number of systematic reviews on the role of sodium bicarbonate compared with isotonic saline in the prevention of CI-AKI are available [27-33]. The most recent and probably the most complete systematic review analyzed randomized controlled trials (RCTs) of intravenous sodium bicarbonate that prespecified the outcome of CI- AKI as a 25% increase in baseline SCr concentration or an absolute increase of 0.5 mg/dl (44.2 μmol/l) after contrast-media administration [33]. Twenty-three published and unpublished trials with information on 3,563 patients and 396 CI-AKI events were included. The pooled relative risk was 0.62 (95% confidence interval = 0.45 to 0.86), with evidence of significant heterogeneity across studies due to the difference in the estimates between published and unpublished studies. Meta-regression showed that small, poor-quality studies that assessed outcomes soon after contrast-media administration were more likely to suggest the benefit of bicarbonate (P <0.05 for all). No clear effects of treatment on the risk for dialysis, heart failure, and total mortality were identified.
One should note that mixing of the bicarbonate solution is often done at the bedside or in the hospital pharmacy, with the possibility for errors leading to the infusion of a hypertonic bicarbonate solution. The potential for harm from dosing errors and the added burden from this bedside preparation have to be taken into account in clinical practice when making a choice between using bicarbonate rather than standard isotonic saline solutions. Taken together, the Work Group concluded that there is a possible but inconsistent benefit of bicarbonate solutions based on overall moderate-quality evidence. The potential of harm and the burden for preparing the bicarbonate solutions led the Work Group not to express a preference for or against one solution (isotonic saline or isotonic bicarbonate). Either solution can therefore be used for the prevention of CI-AKI. In any case, volume expansion should be intravenous. Oral volume expansion may have some benefit, but there is insufficient evidence to show it is as effective as intravenous volume expansion [34].
E6: We recommend intravenous volume expansion with either isotonic sodium chloride or sodium bicarbonate solutions, rather than no intravenous volume expansion, in patients at increased risk for CI-AKI (Grade 1A)
E7: We recommend not using oral fluids alone in patients at increased risk for CI-AKI (Grade 1C)
Other interventions to reduce contrast-induced AKI
Many, but not all, studies have shown NAC to have a protective effect on CI-AKI when administered before the onset of renal insult (for a review, see McCullough [35]). In addition, NAC is inexpensive and appears to be safe, although it may have some detrimental effects on myocardial and coagulation function [36-38]. The safety of NAC should further be amended, particularly when high intravenous doses are used, as in some of the RCTs in CI-AKI. When prospectively studied in acetaminophen poisoning, intravenous NAC produced anaphylactoid reactions in up to 48% of participants [39]. Although most of these reactions were mild, at least one death has been reported in a patient with asthma [40]. Based on the existing evidence, the overall benefit of NAC is not consistent or overwhelming. On the other hand, oral NAC has a low risk of adverse events and usually a low cost.
The efficacy of theophylline in preventing CI-AKI has been addressed by a systematic review and meta-analysis in 2005 [41], and by another meta-analysis in 2008 [42]. Both meta-analyses indicated a nonsignificant trend toward a renoprotective effect of theophylline prophylaxis but the overall benefit was small and findings were inconsistent across studies. The benefit tended to be less marked in patients receiving iso-osmolar, nonionic contrast media, and in patients undergoing a predefined saline protocol. Two prospective randomized trials of fenoldopam for CI-AKI showed negative results [43,44].
Contrast media can be efficiently removed from blood by intermittent hemodialysis (IHD), and a single session effectively removes 60 to 90% of contrast media [45,46]. On the basis of these observations, several studies have explored the prophylactic value of IHD in patients at high risk for AKI, but most of these studies have not demonstrated a reduced incidence of CI-AKI [46,47]. A recent meta-analysis of studies using periprocedural extra-corporeal blood purification techniques concluded that such treatments did not decrease the incidence of CI-AKI [45].
E8: We suggest using oral NAC, together with intravenous isotonic crystalloids, in patients at increased risk of CI-AKI (Grade 2D)
E9: We suggest not using theophylline to prevent CI-AKI (Grade 2C)
E10: We recommend not using fenoldopam to prevent CI-AKI (Grade 1B)
E11: We suggest not using prophylactic IHD or hemofiltration for contrast-media removal in patients at increased risk for CI-AKI (Grade 2C)
F. Renal replacement therapy for treatment of AKI
Initiating and discontinuing RRT for patients with AKI
While no RCTs exist for dialysis for life-threatening indications, it is widely accepted that patients with severe hyperkalemia, severe acidosis, pulmonary edema, and uremic complications should be dialyzed emergently. In the absence of kidney function, and when therapeutic measures that promote the intracellular shift of potassium (such as correction of acidosis with bicarbonate, glucose and insulin infusion, and β2 agonists) are exhausted, an excess of potassium can only be eliminated with RRT.
Provision of acute RRT to children requires special consideration. The epidemiology of pediatric AKI has changed from primary kidney disease in the 1980s to injury resulting from another systemic illness or its treatment (for example, sepsis and nephrotoxic medications) [48,49]. Newborns with inborn errors of metabolism who do not respond to dietary and pharmacologic management require expeditious dialytic removal of ammonia to decrease the risk of death and long-term neurologic dysfunction [50], and infants who receive surgical correction of congenital heart disease often receive peritoneal dialysis early after cardiopulmonary bypass to prevent fluid overload and/or minimize the proinflammatory response. Finally, children develop multiorgan dysfunction very rapidly in their ICU course, with the maximal organ dysfunction occurring with 72 hours and mortality occurring within 7 days of ICU admission, respectively [51,52]. In both children and adults, therefore, the issue of timing of dialysis initiation is critically important. Fluid overload has emerged as a significant factor associated with mortality in children as well as adults with AKI requiring RRT, although the physiological link between increasing percentage volume overload and mortality is not completely clear [53-59].
Many, but not all, patients requiring RRT will recover enough function not to require long-term RRT [60-62]. The mean duration of RRT in two recent large RCTs was 12 to 13 days [63,64]. Daily assessment of both intrinsic kidney function and the ongoing appropriateness of RRT consistent with the goals of therapy for the patient is therefore required. Analysis from the BEST KIDNEY study showed that continuous renal replacement therapy (CRRT) was withdrawn in 13% of the patients, representing 29% of those who died while on CRRT and 21% of all nonsurvivors [65].
Only one RCT has evaluated the potential role of diuretics in resolving AKI in patients receiving RRT [66]. In this trial, there were no differences in need for repeated continuous venovenous hemofiltration or renal recovery during the ICU or hospital stay. An observational study of discontinuation of RRT also found no difference in diuretic use between patents with successful or unsuccessful discontinuation of IHD [67].
F1: Initiate RRT emergently when life-threatening changes in fluid, electrolyte, and acid-base balance exist (not graded)
F2: Consider the broader clinical context, the presence of conditions that can be modified with RRT, and trends of laboratory tests - rather than single blood urea nitrogen and creatinine thresholds alone - when making the decision to start RRT (not graded)
F3: Discontinue RRT when it is no longer required, either because intrinsic kidney function has recovered to the point that it is adequate to meet patient needs, or because RRT is no longer consistent with the goals of care (not graded)
F4: We suggest not using diuretics to enhance kidney function recovery or to reduce the duration or frequency of RRT (Grade 2B)
Anticoagulation for RRT
A recent meta-analysis of 11 RCTs comparing unfractionated heparin with low-molecular-weight heparin in chronic IHD concluded that both are equally safe in terms of bleeding complications and equally as effective in preventing extracorporeal thrombosis [68]. Mainly because of the convenience of using a single bolus injection at the start of IHD, the reduced risk of heparin-induced thrombocytopenia (HIT), and long-term side effects such as abnormal serum lipids, osteoporosis, and hypoaldosteronism, the European practice guideline for prevention of dialyzer clotting suggests using low-molecular-weight heparin rather than unfractionated heparin in chronic dialysis patients [69]. Many European centers have extrapolated this to IHD for AKI, although studies in this setting are lacking.
Crossover comparison of prostacyclin with low-molecular-weight heparin in chronic dialysis patients shows reduced efficiency [70]. A small trial showed reduced bleeding complications compared with low-dose heparin, but at the expense of slightly more premature terminations [71]. Additional drawbacks are systemic hypotension and the high costs. The routine use of alternative anticoagulants therefore cannot be recommended in patients with AKI.
Five randomized trials have compared citrate with heparins during CRRT [72-76]. For ethical reasons, these trials were performed in patients without increased bleeding risk. Overall, citrate appears to be superior to heparin in terms of either filter survival or patient outcomes or both. In the largest and most recent randomized trial, 200 patients treated with postdilution continuous venovenous hemofiltration were randomized to citrate or to nadroparin, a low-molecular-weight heparin [76]. Safety was significantly better in the citrate group while circuit survival did not significantly differ. Rather surprisingly, an improved renal recovery and an improved hospital survival were also found in the citrate group. This observation requires further investigation. Metabolic complications were infrequent in these randomized trials. In observational trials, the most frequent metabolic complication with citrate is metabolic alkalosis, occurring in up to 50% of the patients [77-79]. In recently published surveys or large clinical trials, the use of regional citrate anticoagulation is still limited to 0 to 20% of the patients/treatments [63,64,80]. The Work Group therefore only recommends the use of citrate for anticoagulation during CRRT in patients that do not have shock or severe liver failure, and in centers that have an established protocol for citrate anticoagulation.
Unfractionated heparin still remains the most widely used anticoagulant during CRRT [63,64,80], mostly administered as a prefilter infusion, with large variability in the administered doses. When choosing a dose of heparin, the clinician should realize that the relationship between the heparin dose, the activated partial thromboplastin time, filter survival, and bleeding complications is not straightforward [81-87], but it is common practice to measure the activated partial thromboplastin time for safety reasons and to adapt the target to the bleeding risk of the patient. No advantage has been found for low-molecular-weight heparin for CRRT [83]. In one study, daily costs, including the coagulation assays, were 10% higher with dalteparin [88]. Alternative anticoagulants include the protease inhibitor nafamostat and the platelet inhibitors, prostacyclin and analogues. Both have a short half-life and a low molecular weight, with the theoretical advantage of extracorporeal elimination and reduced systemic anticoagulation. Nafamostat is a protease inhibitor that is mainly used in Japan and is not available in the USA or Europe. Small observational trials in chronic dialysis patients with increased bleeding risk suggest a reduced bleeding incidence [89-91]. Concerns with nafamostat include the absence of an antidote, and side effects such as anaphylaxis, hyperkalemia, and bone marrow suppression [92-94].
A few small trials showed improved filter survival during CRRT when adding prostaglandins to heparin compared with heparin alone [95-97]. However, prostaglandins appear to have a limited efficacy when used alone, induce systemic hypotension [98,99], and are expensive. Their use during CRRT therefore cannot be recommended.
We suggest performing RRT without anticoagulation in patients with increased bleeding risk. A possible exception can be made for patients who do not have contraindications for citrate. With regard to the diagnosis and management of HIT, we refer to the recent guideline of the American College of Chest Physicians [100] and the European best practice guideline on chronic dialysis [69]. Alternative nonheparin anticoagulants in patients with strong suspicion of HIT are recommended. Candidates are the direct thrombin inhibitors lepirudin, argatroban, or bivaluridin, or the antithrombin-dependent activated factor X inhibitors danaparoid or fondaparinix. Pharmacokinetic data and dosing guidelines for these alternative anticoagulants have been published for IHD [101,102] and CRRT [103].
F5: In a patient with AKI requiring RRT, base the decision to use anticoagulation for RRT on assessment of the patient's potential risks and benefits from anticoagulation (see Figure 1) (not graded)
Figure 1.
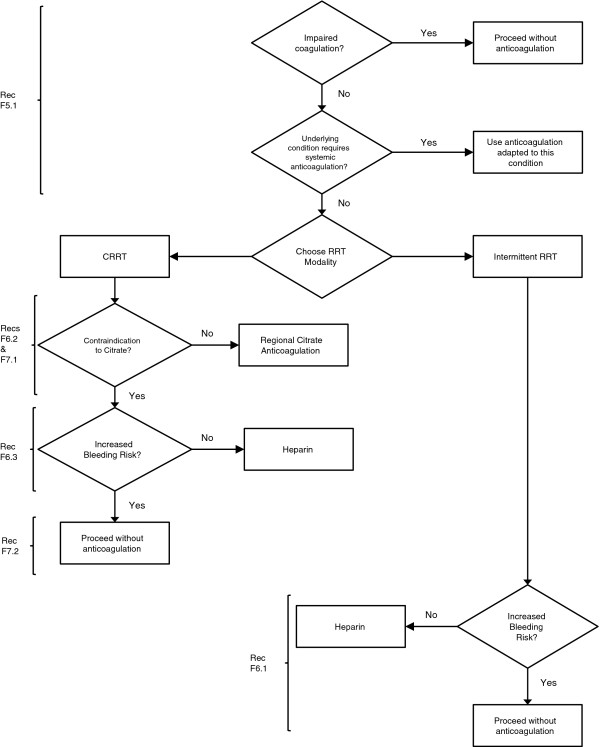
Flow-chart summary of recommendations. Heparin includes low-molecular-weight heparin or unfractionated heparin. CRRT, continuous renal replacement therapy; RRT, renal replacement therapy.
F5.1: We recommend using anticoagulation during RRT in AKI if a patient does not have an increased bleeding risk or impaired coagulation and is not already receiving systemic anticoagulation (Grade 1B)
F6: For patients without an increased bleeding risk or impaired coagulation and not already receiving effective systemic anticoagulation, we suggest the following:
F6.1: For anticoagulation in intermittent RRT, we recommend using either unfractionated heparin or low-molecular-weight heparin, rather than other anticoagulants (Grade 1C)
F6.2: For anticoagulation in CRRT, we suggest using regional citrate anticoagulation rather than heparin in patients who do not have contraindications for citrate (Grade 2B)
F6.3: For anticoagulation during CRRT in patients who have contraindications for citrate, we suggest using either unfractionated heparin or low-molecular-weight heparin, rather than other anticoagulants (Grade 2C)
F7: For patients with increased bleeding risk who are not receiving anticoagulation, we suggest the following for anticoagulation during RRT:
F7.1: We suggest using regional citrate anticoagulation, rather than no anticoagulation, during CRRT in a patient without contraindications for citrate (Grade 2C)
F7.2: We suggest avoiding regional heparinization during CRRT in a patient with increased risk of bleeding (Grade 2C)
F8: In a patient with HIT, all heparin must be stopped and we recommend using directthrombin inhibitors (such as argatroban) or Factor Xa inhibitors (such as danaparoid or fondaparinux) rather than other or no anticoagulation during RRT (Grade 1A)
F8.1: In a patient with HIT who does not have severe liver failure, we suggest using argatroban rather than other thrombin or Factor Xa inhibitors during RRT (Grade 2C)
Vascular access and dialysis membranes
Both the Centers for Disease Control guidelines for prevention of catheter-related infections and the Kidney Disease Outcomes Quality Initiative guideline for vascular access in chronic dialysis patients recommend using a cued catheter for dialysis if a prolonged (for example, >1 to 3 weeks) period of temporary access is anticipated [104,105]. In two recent large randomized trials, the mean duration of RRT for AKI was 12 to 13 days [63,64]. This duration probably does not justify the burden of an initial tunneled catheter in all patients with AKI receiving RRT. Rather, selected use of tunneled catheters in patients who require prolonged RRT is warranted.
Although generally associated with the lowest rate of infectious complications, the Centers for Disease Control guideline as well as the Kidney Disease Outcomes Quality Initiative guideline recommend avoiding the subclavian vein for RRT access [104,105], because this may lead to central vein stenosis and jeopardize subsequent permanent access. Recirculation has been shown to be more frequent in femoral than subclavian or jugular dialysis catheters, especially with shorter femoral catheters [106,107]. Catheter insertion should be performed with strict adherence to infection-control policies, including maximal sterile barrier precautions and chlorhexidine 2% skin antisepsis [105,108,109].
Two meta-analyses exploring the role of real-time two-dimensional ultrasound for central vein cannulation concluded that, compared with the landmark method, ultrasound-guided venous access increases the probability of successful catheter placement and reduces the risk of complications, the need for multiple catheter placement attempts, and the time required for the procedure. The advantage appears most pronounced for the jugular vein, whereas the evidence is scarce for the subclavian and femoral vein [110,111]. Subsequent large randomized trials have confirmed the superiority of ultrasound guidance [112,113]. The Kidney Disease Outcomes Quality Initiative guideline for vascular access also recommends using ultrasound-assisted insertion [104].
A postprocedural chest radiograph is conventionally performed to confirm the correct position of the catheter and to assess for potential complications. Although this procedure has been debated after uneventful placement of a central venous catheter, the high blood flows used during RRT and the administration of anticoagulants necessitate confirming the correct position before initiating dialysis therapy [104]. For detailed instructions on catheter care, the reader is referred to published guidelines [104,105,108,109]. These guidelines also recommend not using dialysis catheters for applications other than RRT, except under emergency circumstances [105]. The Centers for Disease Control, the National Health Service, and the Infectious Diseases Society of America guidelines strongly recommend against routinely using antibiotic lock solutions in the central venous catheter, because of their potential to promote fungal infections, antimicrobial resistance, and systemic toxicity [105,108,109].
A recent meta-analysis of 10 randomized trials or quasi-RCTs in 1,100 patients could not establish any advantage for biocompatible or high-flux membranes [114]. Of note, the authors chose to include modified cellulose membranes in the bioincompatible group, although other investigators consider modified cellulosic membranes to be biocompatible. When comparing the synthetic membranes with cuprophane, there was a trend towards reduced mortality with the synthetic membranes. This meta-analysis also did not assess the side effects of different membrane compositions on more proximal, temporal associations, such as acute hypotension or fever. As a result, the Work Group agrees with the authors' conclusion that the use of either a biocompatible or modified cellulose acetate membrane appears to be appropriate.
F9: We suggest initiating RRT in patients with AKI via an uncuffed nontunneled dialysis catheter, rather than a tunneled catheter (Grade 2D)
F10: When choosing a vein for insertion of a dialysis catheter in patients with AKI, consider these preferences (not graded):
• first choice: right jugular vein;
• second choice: femoral vein;
• third choice: left jugular vein;
• last choice: subclavian vein with preference for the dominant side
F11: We recommend using ultrasound guidance for dialysis catheter insertion (Grade 1A)
F12: We recommend obtaining a chest radiograph promptly after placement and before first use of an internal jugular or subclavian dialysis catheter (Grade 1B)
F13: We suggest not using topical antibiotics over the skin insertion site of a nontunneled dialysis catheter in ICU patients with AKI requiring RRT (Grade 2C)
F14: We suggest not using antibiotic locks for prevention of catheter-related infections ofnontunneled dialysis catheters in AKI requiring RRT (Grade 2C)
F15: We suggest using dialyzers with a biocompatible membrane for IHD and CRRT in patients with AKI (Grade 2C)
Modality of RRT for AKI
Several RCTs have compared CRRT with IHD in AKI patients. The most inclusive meta-analysis was performed by the Cochrane Collaboration, analyzing 15 RCTs in 1,550 AKI patients. This analysis concluded that outcomes were not different for critically ill AKI patients treated with CRRT versus IHD for hospital mortality, ICU mortality, length of hospitalization, and renal recovery (free of dialysis on discharge) in survivors [115]. Comparable results have been reported by other meta-analyses [116,117]. Most trials excluded patients with hypotension or maximized efforts to improve the hemodynamic tolerance of IHD. The high rate of crossover between the treatment modalities also complicates the interpretation of the results.
Many clinicians prefer CRRT in critically ill AKI patients with severe hemodynamic instability, because of better hemodynamic tolerance due to the slower fluid removal and the absence of fluid shifts induced by rapid solute removal. The Cochrane meta-analysis, however, could not establish a difference in the number of patients with hemodynamic instability (however defined) or with hypotension. On the contrary, the mean arterial pressure at the end of the treatment was significantly higher with CRRT than with IHD and the number of patients requiring escalation of vasopressor therapy was significantly lower with CRRT compared with IHD [115].
Slow low-efficiency dialysis has been proposed as an alternative to other forms of RRT and is used in many centers worldwide for logistical reasons. A recent review summarizes the results obtained with slow low-efficiency dialysis in several studies and discusses in detail the technical aspects of this dialysis method [118]. However, randomized trials comparing IHD with slow low-efficiency dialysis have not been performed. Also, clinical experience is far more limited with slow low-efficiency dialysis compared with CRRT, and very few randomized studies have compared slow low-efficiency dialysis to CRRT.
In a patient with acute brain injury, IHD may worsen neurological status by compromising cerebral perfusion pressure. This may be the result of a decrease of mean arterial pressure (dialysis-induced hypotension) or an increase of cerebral edema and intracranial pressure (dialysis disequilibrium), and may jeopardize the potential for neurologic recovery. Dialysis disequilibrium results from the rapid removal of solutes, resulting in intracellular fluid shifts. Both hypotension and disequilibrium can be avoided by the slow progressive removal of fluids and solutes that occurs during CRRT [119]. Small observational trials and case reports in patients with intracranial pressure monitoring indeed reported increases in intracranial pressure with IHD [120,121]. Using computed tomography scans to measure brain density, Ronco and colleagues [122] showed an increase of brain water content after IHD whereas no such changes were observed after CRRT.
F16: Use continuous and intermittent RRT as complementary therapies in AKI patients (not graded)
F17: We suggest using CRRT, rather than standard intermittent RRT, for hemodynamically unstable patients (Grade 2B)
F18: We suggest using CRRT, rather than intermittent RRT, for AKI patients with acute brain injury or other causes of increased intracranial pressure or generalized brain edema (Grade 2B)
Dialysate and replacement fluid
Use of bicarbonate as a buffer in the dialysate or replacement fluid of AKI patients results in better correction of acidosis, lower lactate levels, and improved hemodynamic tolerance [123,124]. These effects are most pronounced in patients with circulatory problems and in those with liver dysfunction. An international quality standard for dialysis fluid is in preparation by the International Society for Standardization. Until international standards are in place, we recommend that dialysis fluids and replacement fluids in patients with AKI, at a minimum, comply with American Association of Medical Instrumentation standards for bacteria and endotoxins [125-127]. When local standards exceed American Association of Medical Instrumentation standards, local standards should be followed.
F19: We suggest using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI (Grade 2C)
F20: We recommend using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI and circulatory shock (Grade 1B)
F21: We suggest using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI and liver failure and/or lactic acidemia (Grade 2B)
F22: We recommend that dialysis fluids and replacement fluids in patients with AKI, at a minimum, comply with American Association of Medical Instrumentation standards regarding contamination with bacteria and endotoxins (Grade 1B)
Intensity of RRT
Several clinical investigations have shown that the actual delivered dose of RRT in AKI patients is frequently smaller than the prescribed dose, and is even smaller than the recommended minimum for chronic kidney disease patients [128-132]. Impediments to adequate dose delivery were hemodynamic instability, patient size, access problems, technical problems, need for patient transportation, and early filter clotting. In determining a prescription of RRT it is mandatory to consider parameters other than small-solute clearance, such as patients' fluid balance, acid-base and electrolyte homeostasis, and nutrition, among others, as possible components of an optimal RRT dose. In fact, positive fluid balance appears to be an independent risk factor for mortality in AKI patients [133].
There are only two adequately designed and executed RCTs testing intermittent or extended RRT doses in AKI [64,134]. Neither study showed improvement in mortality or renal recovery when the dialysis dose was increased, either by increasing the clearance × time/volume (Kt/V) ratio above 3.9 weekly or by achieving a plasma urea target below 90 mg/dl (15 mmol/l) in AKI patients. Consistent with data on the dose of IHD in chronic kidney disease [135] and consistent with the lower-dose arm in the Acute Renal Failure Trial Network study [64], however, we recommend a thrice-weekly Kt/V ratio of 1.3 or a weekly Kt/V ratio of 3.9 for IHD in AKI. Similarly, there are now consistent data from two large multicenter trials showing no benefits of increasing CRRT doses in AKI patients above effluent flows of 20 to 25 ml/kg/hour [63,64]. In clinical practice, in order to achieve a delivered dose of 20 to 25 ml/kg/hour, it is generally necessary to prescribe in the range of 25 to 30 ml/kg/hour and to minimize interruptions in CRRT.
F23: The dose of RRT to be delivered should be prescribed before starting each session of RRT (not graded). We recommend frequent assessment of the actual delivered dose in order to adjust the prescription (Grade 1B)
F24: Provide RRT to achieve the goals of electrolyte, acid-base, solute, and fluid balance that will meet the patient's needs (not graded)
F25: We recommend delivering a Kt/V ratio of 3.9 per week when using intermittent or extended RRT in AKI (Grade 1A)
F26: We recommend delivering an effluent volume of 20 to 25 ml/kg/hour for CRRT in AKI (Grade 1A). This will usually require a higher prescription of effluent volume (not graded)
Abbreviations
AKI: acute kidney injury; CI-AKI: contrast-induced acute kidney injury; CRRT: continuous renal replacement therapy; HIT: heparin-induced thrombocytopenia; ICU: intensive care unit; IHD: intermittent hemodialysis; KDIGO, Kidney Disease: Improving Global Outcomes; Kt/V: clearance×time/volume; NAC: N-acetylcysteine; RCT: randomized controlled trial; RRT: renal replacement therapy; SCr: serum creatinine.
Competing interests
NL declares that he has no competing interests. JAK has served as an Advisor/ Consultant for Abbott, Alere, Astute Medical, Baxter, CytoSorbents, EBI, Eli Lilly, Fresenius, Gambro, Siemens and Spectral Diagnostics, and as a Speaker for Baxter, Fresenius, and Gambro. He has also received grant/research support from Astute Medical, Baxter, CytoSorbents and Gambro.
Authors' information
NL is Emeritus Professor of Medicine and former Chief of the Renal Division at the University Hospital of Ghent. JAK is Professor of Critical Care Medicine, Medicine, Bioengineering and Clinical and Translational Science, and Vice Chair for Research within the Department of Critical Care Medicine at the University of Pittsburgh. He is also the Director of the Program on Bioengineering and Organ Support for the Clinical Research Investigation and Systems Modeling of Acute Illness Center at the University of Pittsburgh.
Contributor Information
Norbert Lameire, Email: norbert.lameire@ugent.be.
John A Kellum, Email: kellumja@ccm.upmc.edu.
Acknowledgements
A special debt of gratitude is owed to the KDIGO Co-Chairs Kai-Uwe Eckardt and Bertram Kasiske and the KDIGO Board for their invaluable guidance throughout the development of this guideline. In particular, the authors thank the Evidence Review Team members - Katrin Uhlig, Jose Calvo-Broce, Aneet Deo, and Amy Earley - for their substantial contribution to the rigorous assessment of the available evidence. They are also especially grateful to the Work Group members for their expertise throughout the entire process of literature review, data extraction, meeting participation, the critical writing and editing of the statements and rationale, which made the publication of this guideline possible. The generous gift of their time and dedication is greatly appreciated. Finally, and on behalf of the Work Group, the authors gratefully acknowledge the careful assessment of the draft guideline by external reviewers. The Work Group considered all of the valuable comments made, and where appropriate suggested changes were incorporated into the final publication.
References
- KDIGO AKI Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;17:1–138. [Google Scholar]
- Kidney Disease: Improving Global Outcomes. http://www.kdigo.org
- KDIGO Clinical Practice Guidelines: Online Appendix F. http://www.kdigo.org/clinical_practice_guidelines/AKI.php
- Uhlig K, Macleod A, Craig J, Lau J, Levey AS, Levin A, Moist L, Steinberg E, Walker R, Wanner C, Lameire N, Eknoyan G. Grading evidence and recommendations for clinical practice guidelines in nephrology. A position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2006;17:2058–2065. doi: 10.1038/sj.ki.5001875. [DOI] [PubMed] [Google Scholar]
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O'Connell D, Oxman AD, Phillips B, Schunemann HJ, Edejer TT, Varonen H, Vist GE, Williams JW Jr, Zaza S. GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;17:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lameire N, Adam A, Becker CR, Davidson C, McCullough PA, Stacul F, Tumlin J. Baseline renal function screening. Am J Cardiol. 2006;17:21K–26K. doi: 10.1016/j.amjcard.2006.01.021. [DOI] [PubMed] [Google Scholar]
- Bruce RJ, Djamali A, Shinki K, Michel SJ, Fine JP, Pozniak MA. Background fluctuation of kidney function versus contrast-induced nephrotoxicity. AJR Am J Roentgenol. 2009;17:711–718. doi: 10.2214/AJR.08.1413. [DOI] [PubMed] [Google Scholar]
- Perazella MA. Current status of gadolinium toxicity in patients with kidney disease. Clin J Am Soc Nephrol. 2009;17:461–469. doi: 10.2215/CJN.06011108. [DOI] [PubMed] [Google Scholar]
- Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, Leon MB, Dangas G. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;17:1393–1399. doi: 10.1016/j.jacc.2004.06.068. [DOI] [PubMed] [Google Scholar]
- Cigarroa RG, Lange RA, Williams RH, Hillis LD. Dosing of contrast material to prevent contrast nephropathy in patients with renal disease. Am J Med. 1989;17(6 Pt 1):649–652. doi: 10.1016/0002-9343(89)90437-3. [DOI] [PubMed] [Google Scholar]
- Nyman U, Bjork J, Aspelin P, Marenzi G. Contrast medium dose-to-GFR ratio: a measure of systemic exposure to predict contrast-induced nephropathy after percutaneous coronary intervention. Acta Radiol. 2008;17:658–667. doi: 10.1080/02841850802050762. [DOI] [PubMed] [Google Scholar]
- Laskey WK, Jenkins C, Selzer F, Marroquin OC, Wilensky RL, Glaser R, Cohen HA, Holmes DR Jr. Volume-to-creatinine clearance ratio: a pharmacokinetically based risk factor for prediction of early creatinine increase after percutaneous coronary intervention. J Am Coll Cardiol. 2007;17:584–590. doi: 10.1016/j.jacc.2007.03.058. [DOI] [PubMed] [Google Scholar]
- Nyman U, Almen T, Aspelin P, Hellstrom M, Kristiansson M, Sterner G. Contrast-medium-Induced nephropathy correlated to the ratio between dose in gram iodine and estimated GFR in ml/min. Acta Radiol. 2005;17:830–842. doi: 10.1080/02841850500335051. [DOI] [PubMed] [Google Scholar]
- Goldfarb S, Spinler S, Berns JS, Rudnick MR. Low-osmolality contrast media and the risk of contrast-associated nephrotoxicity. Invest Radiol. 1993;17(Suppl 5):S7–S10. doi: 10.1097/00004424-199311001-00003. discussion S11-S12. [DOI] [PubMed] [Google Scholar]
- Barrett BJ, Carlisle EJ. Metaanalysis of the relative nephrotoxicity of high- and low-osmolality iodinated contrast media. Radiology. 1993;17:171–178. doi: 10.1148/radiology.188.1.8511292. [DOI] [PubMed] [Google Scholar]
- Aspelin P, Aubry P, Fransson SG, Strasser R, Willenbrock R, Berg KJ. Nephrotoxic effects in high-risk patients undergoing angiography. N Engl J Med. 2003;17:491–499. doi: 10.1056/NEJMoa021833. [DOI] [PubMed] [Google Scholar]
- Feldkamp T, Baumgart D, Elsner M, Herget-Rosenthal S, Pietruck F, Erbel R, Philipp T, Kribben A. Nephrotoxicity of iso-osmolar versus low-osmolar contrast media is equal in low risk patients. Clin Nephrol. 2006;17:322–330. doi: 10.5414/cnp66322. [DOI] [PubMed] [Google Scholar]
- Hardiek KJ, Katholi RE, Robbs RS, Katholi CE. Renal effects of contrast media in diabetic patients undergoing diagnostic or interventional coronary angiography. J Diabetes Complications. 2008;17:171–177. doi: 10.1016/j.jdiacomp.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Juergens CP, Winter JP, Nguyen-Do P, Lo S, French JK, Hallani H, Fernandes C, Jepson N, Leung DY. Nephrotoxic effects of iodixanol and iopromide in patients with abnormal renal function receiving N-acetylcysteine and hydration before coronary angiography and intervention: a randomized trial. Intern Med J. 2009;17:25–31. doi: 10.1111/j.1445-5994.2008.01675.x. [DOI] [PubMed] [Google Scholar]
- Laskey W, Aspelin P, Davidson C, Rudnick M, Aubry P, Kumar S, Gietzen F, Wiemer M. Nephrotoxicity of iodixanol versus iopamidol in patients with chronic kidney disease and diabetes mellitus undergoing coronary angiographic procedures. Am Heart J. 2009;17:822–828. doi: 10.1016/j.ahj.2009.08.016. [DOI] [PubMed] [Google Scholar]
- Nie B, Cheng WJ, Li YF, Cao Z, Yang Q, Zhao YX, Guo YH, Zhou YJ. A prospective, double-blind, randomized, controlled trial on the efficacy and cardiorenal safety of iodixanol vs. iopromide in patients with chronic kidney disease undergoing coronary angiography with or without percutaneous coronary intervention. Catheter Cardiovasc Interv. 2008;17:958–965. doi: 10.1002/ccd.21713. [DOI] [PubMed] [Google Scholar]
- Rudnick MR, Davidson C, Laskey W, Stafford JL, Sherwin PF. Nephrotoxicity of iodixanol versus ioversol in patients with chronic kidney disease: the Visipaque Angiography/Interventions with Laboratory Outcomes in Renal Insufficiency (VALOR) Trial. Am Heart J. 2008;17:776–782. doi: 10.1016/j.ahj.2008.05.023. [DOI] [PubMed] [Google Scholar]
- Solomon RJ, Natarajan MK, Doucet S, Sharma SK, Staniloae CS, Katholi RE, Gelormini JL, Labinaz M, Moreyra AE. Cardiac Angiography in Renally Impaired Patients (CARE) study: a randomized double-blind trial of contrast-induced nephropathy in patients with chronic kidney disease. Circulation. 2007;17:3189–3196. doi: 10.1161/CIRCULATIONAHA.106.671644. [DOI] [PubMed] [Google Scholar]
- Heinrich MC, Haberle L, Muller V, Bautz W, Uder M. Nephrotoxicity of iso-osmolar iodixanol compared with nonionic low-osmolar contrast media: meta-analysis of randomized controlled trials. Radiology. 2009;17:68–86. doi: 10.1148/radiol.2501080833. [DOI] [PubMed] [Google Scholar]
- Jo SH, Youn TJ, Koo BK, Park JS, Kang HJ, Cho YS, Chung WY, Joo GW, Chae IH, Choi DJ, Oh BH, Lee MM, Park YB, Kim HS. Renal toxicity evaluation and comparison between visipaque (iodixanol) and hexabrix (ioxaglate) in patients with renal insufficiency undergoing coronary angiography: the RECOVER study: a randomized controlled trial. J Am Coll Cardiol. 2006;17:924–930. doi: 10.1016/j.jacc.2006.06.047. [DOI] [PubMed] [Google Scholar]
- Mehran R, Nikolsky E, Kirtane AJ, Caixeta A, Wong SC, Teirstein PS, Downey WE, Batchelor WB, Casterella PJ, Kim YH, Fahy M, Dangas GD. Ionic low-osmolar versus nonionic iso-osmolar contrast media to obviate worsening nephropathy after angioplasty in chronic renal failure patients: the ICON (Ionic versus non-ionic Contrast to Obviate worsening Nephropathy after angioplasty in chronic renal failure patients) study. JACC Cardiovasc Interv. 2009;17:415–421. doi: 10.1016/j.jcin.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Brar SS, Hiremath S, Dangas G, Mehran R, Brar SK, Leon MB. Sodium bicarbonate for the prevention of contrast induced-acute kidney injury: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2009;17:1584–1592. doi: 10.2215/CJN.03120509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan SE, L'Allier P, Chetcuti S, Grossman PM, Nallamothu BK, Duvernoy C, Bates E, Moscucci M, Gurm HS. Current role of sodium bicarbonate-based preprocedural hydration for the prevention of contrast-induced acute kidney injury: a meta-analysis. Am Heart J. 2008;17:414–421. doi: 10.1016/j.ahj.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Hoste EA, De Waele JJ, Gevaert SA, Uchino S, Kellum JA. Sodium bicarbonate for prevention of contrast-induced acute kidney injury: a systematic review and meta-analysis. Nephrol Dial Transplant. 2010;17:747–758. doi: 10.1093/ndt/gfp389. [DOI] [PubMed] [Google Scholar]
- Joannidis M, Schmid M, Wiedermann CJ. Prevention of contrast media-induced nephropathy by isotonic sodium bicarbonate: a meta-analysis. Wien Klin Wochenschr. 2008;17:742–748. doi: 10.1007/s00508-008-1117-z. [DOI] [PubMed] [Google Scholar]
- Kanbay M, Covic A, Coca SG, Turgut F, Akcay A, Parikh CR. Sodium bicarbonate for the prevention of contrast-induced nephropathy: a metaanalysis of 17 randomized trials. Int Urol Nephrol. 2009;17:617–627. doi: 10.1007/s11255-009-9569-2. [DOI] [PubMed] [Google Scholar]
- Navaneethan SD, Singh S, Appasamy S, Wing RE, Sehgal AR. Sodium bicarbonate therapy for prevention of contrast-induced nephropathy: a systematic review and meta-analysis. Am J Kidney Dis. 2009;17:617–627. doi: 10.1053/j.ajkd.2008.08.033. [DOI] [PubMed] [Google Scholar]
- Zoungas S, Ninomiya T, Huxley R, Cass A, Jardine M, Gallagher M, Patel A, Vasheghani-Farahani A, Sadigh G, Perkovic V. Systematic review: sodium bicarbonate treatment regimens for the prevention of contrast-induced nephropathy. Ann Intern Med. 2009;17:631–638. doi: 10.7326/0003-4819-151-9-200911030-00008. [DOI] [PubMed] [Google Scholar]
- Taylor AJ, Hotchkiss D, Morse RW, McCabe J. PREPARED: Preparation for Angiography in Renal Dysfunction: a randomized trial of inpatient vs outpatient hydration protocols for cardiac catheterization in mild-to-moderate renal dysfunction. Chest. 1998;17:1570–1574. doi: 10.1378/chest.114.6.1570. [DOI] [PubMed] [Google Scholar]
- McCullough PA. Contrast-induced acute kidney injury. J Am Coll Cardiol. 2008;17:1419–1428. doi: 10.1016/j.jacc.2007.12.035. [DOI] [PubMed] [Google Scholar]
- Molnar Z, Szakmany T, Koszegi T. Prophylactic N-acetylcysteine decreases serum CRP but not PCT levels and microalbuminuria following major abdominal surgery. A prospective, randomised, double-blinded, placebo-controlled clinical trial. Intensive Care Med. 2003;17:749–755. doi: 10.1007/s00134-003-1723-1. [DOI] [PubMed] [Google Scholar]
- Niemi TT, Munsterhjelm E, Poyhia R, Hynninen MS, Salmenpera MT. The effect of N-acetylcysteine on blood coagulation and platelet function in patients undergoing open repair of abdominal aortic aneurysm. Blood Coagul Fibrinolysis. 2006;17:29–34. doi: 10.1097/01.mbc.0000195922.26950.89. [DOI] [PubMed] [Google Scholar]
- Peake SL, Moran JL, Leppard PI. N-acetyl-l-cysteine depresses cardiac performance in patients with septic shock. Crit Care Med. 1996;17:1302–1310. doi: 10.1097/00003246-199608000-00006. [DOI] [PubMed] [Google Scholar]
- Lynch RM, Robertson R. Anaphylactoid reactions to intravenous N-acetylcysteine: a prospective case controlled study. Accid Emerg Nurs. 2004;17:10–15. doi: 10.1016/j.aaen.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Appelboam AV, Dargan PI, Knighton J. Fatal anaphylactoid reaction to N-acetylcysteine: caution in patients with asthma. Emerg Med J. 2002;17:594–595. doi: 10.1136/emj.19.6.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagshaw SM, Ghali WA. Theophylline for prevention of contrast-induced nephropathy: a systematic review and meta-analysis. Arch Intern Med. 2005;17:1087–1093. doi: 10.1001/archinte.165.10.1087. [DOI] [PubMed] [Google Scholar]
- Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: eff ectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;17:284–294. doi: 10.7326/0003-4819-148-4-200802190-00007. [DOI] [PubMed] [Google Scholar]
- Allaqaband S, Tumuluri R, Malik AM, Gupta A, Volkert P, Shalev Y, Bajwa TK. Prospective randomized study of N-acetylcysteine, fenoldopam, and saline for prevention of radiocontrast-induced nephropathy. Catheter Cardiovasc Interv. 2002;17:279–283. doi: 10.1002/ccd.10323. [DOI] [PubMed] [Google Scholar]
- Stone GW, McCullough PA, Tumlin JA, Lepor NE, Madyoon H, Murray P, Wang A, Chu AA, Schaer GL, Stevens M, Wilensky RL, O'Neill WW. CONTRAST Investigators. Fenoldopam mesylate for the prevention of contrast-induced nephropathy: a randomized controlled trial. JAMA. 2003;17:2284–2291. doi: 10.1001/jama.290.17.2284. [DOI] [PubMed] [Google Scholar]
- Cruz DN, Perazella MA, Ronco C. The role of extracorporeal blood purification therapies in the prevention of radiocontrast-induced nephropathy. Int J Artif Organs. 2008;17:515–524. doi: 10.1177/039139880803100607. [DOI] [PubMed] [Google Scholar]
- Deray G. Dialysis and iodinated contrast media. Kidney Int Suppl. 2006;17:S25–S29. doi: 10.1038/sj.ki.5000371. [DOI] [PubMed] [Google Scholar]
- Vogt B, Ferrari P, Schönholzer C, Marti HP, Mohaupt M, Wiederkehr M, Cereghetti C, Serra A, Huynh-Do U, Uehlinger D, Frey FJ. Prophylactic hemodialysis after radiocontrast media in patients with renal insufficiency is potentially harmful. Am J Med. 2001;17:692–698. doi: 10.1016/S0002-9343(01)00983-4. [DOI] [PubMed] [Google Scholar]
- Hui-Stickle S, Brewer ED, Goldstein SL. Pediatric ARF epidemiology at a tertiary care center from 1999 to 2001. Am J Kidney Dis. 2005;17:96–101. doi: 10.1053/j.ajkd.2004.09.028. [DOI] [PubMed] [Google Scholar]
- Williams DM, Sreedhar SS, Mickell JJ, Chan JC. Acute kidney failure: a pediatric experience over 20 years. Arch Pediatr Adolesc Med. 2002;17:893–900. doi: 10.1001/archpedi.156.9.893. [DOI] [PubMed] [Google Scholar]
- Picca S, Dionisi-Vici C, Abeni D, Pastore A, Rizzo C, Orzalesi M, Sabetta G, Rizzoni G, Bartuli A. Extracorporeal dialysis in neonatal hyperammonemia: modalities and prognostic indicators. Pediatr Nephrol. 2001;17:862–867. doi: 10.1007/s004670100702. [DOI] [PubMed] [Google Scholar]
- Proulx F, Fayon M, Farrell CA, Lacroix J, Gauthier M. Epidemiology of sepsis and multiple organ dysfunction syndrome in children. Chest. 1996;17:1033–1037. doi: 10.1378/chest.109.4.1033. [DOI] [PubMed] [Google Scholar]
- Proulx F, Gauthier M, Nadeau D, Lacroix J, Farrell CA. Timing and predictors of death in pediatric patients with multiple organ system failure. Crit Care Med. 1994;17:1025–1031. doi: 10.1097/00003246-199406000-00023. [DOI] [PubMed] [Google Scholar]
- Foland JA, Fortenberry JD, Warshaw BL, Pettignano R, Merritt RK, Heard ML, Rogers K, Reid C, Tanner AJ, Easley KA. Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit Care Med. 2004;17:1771–1776. doi: 10.1097/01.CCM.0000132897.52737.49. [DOI] [PubMed] [Google Scholar]
- Gillespie RS, Seidel K, Symons JM. Effect of fluid overload and dose of replacement fluid on survival in hemofiltration. Pediatr Nephrol. 2004;17:1394–1399. doi: 10.1007/s00467-004-1655-1. [DOI] [PubMed] [Google Scholar]
- Goldstein SL, Currier H, Graf C, Cosio CC, Brewer ED, Sachdeva R. Outcome in children receiving continuous venovenous hemofiltration. Pediatrics. 2001;17:1309–1312. doi: 10.1542/peds.107.6.1309. [DOI] [PubMed] [Google Scholar]
- Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, Bunchman TE, Baker C, Mottes T, McAfee N, Barnett J, Morrison G, Rogers K, Fortenberry JD. Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int. 2005;17:653–658. doi: 10.1111/j.1523-1755.2005.67121.x. [DOI] [PubMed] [Google Scholar]
- Hayes LW, Oster RA, Tofil NM, Tolwani AJ. Outcomes of critically ill children requiring continuous renal replacement therapy. J Crit Care. 2009;17:394–400. doi: 10.1016/j.jcrc.2008.12.017. [DOI] [PubMed] [Google Scholar]
- Michael M, Kuehnle I, Goldstein SL. Fluid overload and acute renal failure in pediatric stem cell transplant patients. Pediatr Nephrol. 2004;17:91–95. doi: 10.1007/s00467-003-1313-z. [DOI] [PubMed] [Google Scholar]
- Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, Hackbarth R, Somers MJ, Baum M, Symons JM, Flores FX, Benfield M, Askenazi D, Chand D, Fortenberry JD, Mahan JD, McBryde K, Blowey D, Goldstein SL. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis. 2010;17:316–325. doi: 10.1053/j.ajkd.2009.10.048. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Mortis G, Godinez-Luna T, Doig CJ, Laupland KB. Renal recovery after severe acute renal failure. Int J Artif Organs. 2006;17:1023–1030. doi: 10.1177/039139880602901102. [DOI] [PubMed] [Google Scholar]
- Liano F, Pascual J. Epidemiology of acute renal failure: a prospective, multicenter, community-based study. Madrid Acute Renal Failure Study Group. Kidney Int. 1996;17:811–818. doi: 10.1038/ki.1996.380. [DOI] [PubMed] [Google Scholar]
- Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;17:930–936. doi: 10.1053/ajkd.2002.32766. [DOI] [PubMed] [Google Scholar]
- Bellomo R, Cass A, Norton R, Gallagher M, Lo S, Su S, Cole L, Finfer S, McArthur C, McGuinness S, Myburgh J, Scheinkestel C, Bellomo R, Lee J, Ali D, Cass A, Cole L, Finfer S, Gallagher M, Goldsmith D, McGuinness S, Myburgh J, Norton R, Scheinkestel C, Bellomo R, Banerjee A, Bhonagiri D, Blythe D, Botha J, Cade J. et al. Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med. 2009;17:1627–1638. doi: 10.1056/NEJMoa0902413. [DOI] [PubMed] [Google Scholar]
- VA/NIH Acute Renal Failure Trial Network. Palevsky PM, Zhang JH, O'Connor TZ, Chertow GM, Crowley ST, Choudhury D, Finkel K, Kellum JA, Paganini E, Schein RM, Smith MW, Swanson KM, Thompson BT, Vijayan A, Watnick S, Star RA, Peduzzi P. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;17:7–20. doi: 10.1056/NEJMoa0802639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Straaten HO, Ronco C, Kellum JA. Discontinuation of continuous renal replacement therapy: a post hoc analysis of a prospective multicenter observational study. Crit Care Med. 2009;17:2576–2582. doi: 10.1097/CCM.0b013e3181a38241. [DOI] [PubMed] [Google Scholar]
- van der Voort PH, Boerma EC, Koopmans M, Zandberg M, de Ruiter J, Gerritsen RT, Egbers PH, Kingma WP, Kuiper MA. Furosemide does not improve renal recovery after hemofiltration for acute renal failure in critically ill patients: a double blind randomized controlled trial. Crit Care Med. 2009;17:533–538. doi: 10.1097/CCM.0b013e318195424d. [DOI] [PubMed] [Google Scholar]
- Wu VC, Ko WJ, Chang HW, Chen YW, Lin YF, Shiao CC, Chen YM, Chen YS, Tsai PR, Hu FC, Wang JY, Lin YH, Wu KD. National Taiwan University Surgical ICU Acute Renal Failure Study Group (NSARF) Risk factors of early redialysis after weaning from postoperative acute renal replacement therapy. Intensive Care Med. 2008;17:101–108. doi: 10.1007/s00134-007-0813-x. [DOI] [PubMed] [Google Scholar]
- Lim W, Cook DJ, Crowther MA. Safety and efficacy of low molecular weight heparins for hemodialysis in patients with end-stage renal failure: a meta-analysis of randomized trials. J Am Soc Nephrol. 2004;17:3192–3206. doi: 10.1097/01.ASN.0000145014.80714.35. [DOI] [PubMed] [Google Scholar]
- European Best Practice Guidelines Expert Group on Hemodialysis European Renal Association. European Best Practice Guidelines for Haemodialysis (Part 1). V. Chronic intermittent haemodialysis and prevention of clotting in the extracorporal system. Nephrol Dial Transplant. 2002;17(Suppl 7):63–71. doi: 10.1093/ndt/17.suppl_7.63. [DOI] [PubMed] [Google Scholar]
- Novacek G, Kapiotis S, Jilma B, Quehenberger P, Michitsch A, Traindl O, Speiser W. Enhanced blood coagulation and enhanced fibrinolysis during hemodialysis with prostacyclin. Thromb Res. 1997;17:283–290. doi: 10.1016/S0049-3848(97)00255-7. [DOI] [PubMed] [Google Scholar]
- Swartz RD, Flamenbaum W, Dubrow A, Hall JC, Crow JW, Cato A. Epoprostenol (PGI2, prostacyclin) during high-risk hemodialysis: preventing further bleeding complications. J Clin Pharmacol. 1988;17:818–825. doi: 10.1002/j.1552-4604.1988.tb03222.x. [DOI] [PubMed] [Google Scholar]
- Betjes MG, van Oosterom D, van Agteren M, van de Wetering J. Regional citrate versus heparin anticoagulation during venovenous hemofiltration in patients at low risk for bleeding: similar hemofilter survival but significantly less bleeding. J Nephrol. 2007;17:602–608. [PubMed] [Google Scholar]
- Fealy N, Baldwin I, Johnstone M, Egi M, Bellomo R. A pilot randomiz ed controlled crossover study comparing regional heparinization to regional citrate anticoagulation for continuous venovenous hemofiltration. Int J Artif Organs. 2007;17:301–307. doi: 10.1177/039139880703000404. [DOI] [PubMed] [Google Scholar]
- Kutsogiannis DJ, Gibney RT, Stollery D, Gao J. Regional citrate versus systemic heparin anticoagulation for continuous renal replacement in critically ill patients. Kidney Int. 2005;17:2361–2367. doi: 10.1111/j.1523-1755.2005.00342.x. [DOI] [PubMed] [Google Scholar]
- Monchi M, Berghmans D, Ledoux D, Canivet JL, Dubois B, Damas P. Citrate vs. heparin for anticoagulation in continuous venovenous hemofiltration: a prospective randomized study. Intensive Care Med. 2004;17:260–265. doi: 10.1007/s00134-003-2047-x. [DOI] [PubMed] [Google Scholar]
- Oudemans-van Straaten HM, Bosman RJ, Koopmans M, van der Voort PH, Wester JP, van der Spoel JI, Dijksman LM, Zandstra DF. Citrate anticoagulation for continuous venovenous hemofiltration. Crit Care Med. 2009;17:545–552. doi: 10.1097/CCM.0b013e3181953c5e. [DOI] [PubMed] [Google Scholar]
- Mehta RL, McDonald BR, Aguilar MM, Ward DM. Regional citrate antico agulation for continuous arteriovenous hemodialysis in critically ill patients. Kidney Int. 1990;17:976–981. doi: 10.1038/ki.1990.300. [DOI] [PubMed] [Google Scholar]
- Morgera S, Scholle C, Voss G, Haase M, Vargas-Hein O, Krausch D, Melzer C, Rosseau S, Zuckermann-Becker H, Neumayer HH. Metabolic complications during regional citrate anticoagulation in continuous venovenous hemodialysis: single-center experience. Nephron Clin Pract. 2004;17:c131–c136. doi: 10.1159/000079171. [DOI] [PubMed] [Google Scholar]
- Thoenen M, Schmid ER, Binswanger U, Schuepbach R, Aerne D, Schmidlin D. Regional citrate anticoagulation using a citrate-based substitution solution for continuous venovenous hemofiltration in cardiac surgery patients. Wien Klin Wochenschr. 2002;17:108–114. [PubMed] [Google Scholar]
- Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten H, Ronco C, Kellum JA. Continuous renal replacement therapy: a worldwide practice survey. The beginning and ending supportive therapy for the kidney (B.E.S.T. kidney) investigators. Intensive Care Med. 2007;17:1563–1570. doi: 10.1007/s00134-007-0754-4. [DOI] [PubMed] [Google Scholar]
- Davies HT, Leslie G, Pereira SM, Webb SA. A randomized comparative crossover study to assess the affect on circuit life of varying pre-dilution volume associated with CVVH and CVVHDF. Int J Artif Organs. 2008;17:221–227. doi: 10.1177/039139880803100305. [DOI] [PubMed] [Google Scholar]
- Holt AW, Bierer P, Bersten AD, Bury LK, Vedig AE. Continuous renal replacement therapy in critically ill patients: monitoring circuit function. Anaesth Intensive Care. 1996;17:423–429. doi: 10.1177/0310057X9602400402. [DOI] [PubMed] [Google Scholar]
- Joannidis M, Kountchev J, Rauchenzauner M, Schusterschitz N, Ulmer H, Mayr A, Bellmann R. Enoxaparin vs. unfractionated heparin for anticoagulation during continuous veno-venous hemofiltration: a randomized controlled crossover study. Intensive Care Med. 2007;17:1571–1579. doi: 10.1007/s00134-007-0719-7. [DOI] [PubMed] [Google Scholar]
- Stefanidis I, Hagel J, Frank D, Maurin N. Hemostatic alterations during continuous venovenous hemofiltration in acute renal failure. Clin Nephrol. 1996;17:199–205. [PubMed] [Google Scholar]
- Tan HK, Baldwin I, Bellomo R. Continuous veno-venous hemofiltration without anticoagulation in high-risk patients. Intensive Care Med. 2000;17:1652–1657. doi: 10.1007/s001340000691. [DOI] [PubMed] [Google Scholar]
- van de Wetering J, Westendorp RG, van der Hoeven JG, Stolk B, Feuth JD, Chang PC. Heparin use in continuous renal replacement procedures: the struggle between filter coagulation and patient hemorrhage. J Am Soc Nephrol. 1996;17:145–150. doi: 10.1681/ASN.V71145. [DOI] [PubMed] [Google Scholar]
- Yang RL, Liu DW. [Clinical evaluation of hemofiltration without anticoagulation in critically ill patients at high risk of bleeding] Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2007;17:651–655. [PubMed] [Google Scholar]
- Reeves JH, Cumming AR, Gallagher L, O'Brien JL, Santamaria JD. A co ntrolled trial of low-molecular-weight heparin (dalteparin) versus unfractionated heparin as anticoagulant during continuous venovenous hemodialysis with filtration. Crit Care Med. 1999;17:2224–2228. doi: 10.1097/00003246-199910000-00026. [DOI] [PubMed] [Google Scholar]
- Akizawa T, Koshikawa S, Ota K, Kazama M, Mimura N, Hirasawa Y. Nafamostat mesilate: a regional anticoagulant for hemodialysis in patients at high risk for bleeding. Nephron. 1993;17:376–381. doi: 10.1159/000187357. [DOI] [PubMed] [Google Scholar]
- Matsuo T, Kario K, Nakao K, Yamada T, Matsuo M. Anticoagulation with nafamostat mesilate, a synthetic protease inhibitor, in hemodialysis patients with a bleeding risk. Haemostasis. 1993;17:135–141. doi: 10.1159/000216866. [DOI] [PubMed] [Google Scholar]
- Yang JW, Han BG, Kim BR, Lee YH, Kim YS, Yu JM, Choi SO. Superior outcome of nafamostat mesilate as an anticoagulant in patients undergoing maintenance hemodialysis with intracerebral hemorrhage. Ren Fail. 2009;17:668–675. doi: 10.3109/08860220903180616. [DOI] [PubMed] [Google Scholar]
- Maruyama H, Miyakawa Y, Gejyo F, Arakawa M. Anaphylactoid reaction induced by nafamostat mesilate in a hemodialysis patient. Nephron. 1996;17:468–469. doi: 10.1159/000189371. [DOI] [PubMed] [Google Scholar]
- Muto S, Imai M, Asano Y. Mechanisms of hyperkalemia caused by nafamostat mesilate. Gen Pharmacol. 1995;17:1627–1632. doi: 10.1016/0306-3623(95)00072-0. [DOI] [PubMed] [Google Scholar]
- Okada H, Suzuki H, Deguchi N, Saruta T. Agranulocytosis in a haemod ialysed patient induced by a proteinase inhibitor, nafamostate mesilate. Nephrol Dial Transplant. 1992;17:980. doi: 10.1093/ndt/7.9.980a. [DOI] [PubMed] [Google Scholar]
- Birnbaum J, Spies CD, Klotz E, Hein OV, Morgera S, Schink T, Ziemer S, Grund MS, Saalmann R, Kox WJ, Lehmann C. Iloprost for additional anticoagulation in continuous renal replacement therapy - a pilot study. Ren Fail. 2007;17:271–277. doi: 10.1080/08860220601166222. [DOI] [PubMed] [Google Scholar]
- Kozek-Langenecker SA, Spiss CK, Gamsjager T, Domenig C, Zimpfer M. Anticoagulation with prostaglandins and unfractionated heparin during continuous venovenous haemofiltration: a randomized controlled trial. Wien Klin Wochenschr. 2002;17:96–101. [PubMed] [Google Scholar]
- Fabbri LP, Nucera M, Al Malyan M, Becchi C. Regional anticoagulation and antiaggregation for CVVH in critically ill patients: a prospective, randomized, controlled pilot study. Acta Anaesthesiol Scand. 2010;17:92–97. doi: 10.1111/j.1399-6576.2009.02031.x. [DOI] [PubMed] [Google Scholar]
- Fiaccadori E, Maggiore U, Rotelli C, Minari M, Melfa L, Cappe G, Cabassi A. Continuous haemofiltration in acute renal failure with prostacyclin as the sole anti-haemostatic agent. Intensive Care Med. 2002;17:586–593. doi: 10.1007/s00134-002-1249-y. [DOI] [PubMed] [Google Scholar]
- Langenecker SA, Felfernig M, Werba A, Mueller CM, Chiari A, Zimpfer M. Anticoagulation with prostacyclin and heparin during continuous venovenous hemofiltration. Crit Care Med. 1994;17:1774–1781. [PubMed] [Google Scholar]
- Warkentin TE, Greinacher A, Koster A, Lincoff AM. Treatment and prevention of heparin-induced thrombocytopenia: American College of Chest Physicians Evidence-based Clinical Practice Guidelines (8th edition) Chest. 2008;17(6 Suppl):340S–380S. doi: 10.1378/chest.08-0677. [DOI] [PubMed] [Google Scholar]
- Fischer KG. Essentials of anticoagulation in hemodialysis. Hemodial Int. 2007;17:178–189. doi: 10.1111/j.1542-4758.2007.00166.x. [DOI] [PubMed] [Google Scholar]
- O'Shea SI, Ortel TL, Kovalik EC. Alternative methods of anticoagulation for dialysis-dependent patients with heparin-induced thrombocytopenia. Semin Dial. 2003;17:61–67. doi: 10.1046/j.1525-139X.2003.03014.x. [DOI] [PubMed] [Google Scholar]
- Davenport A. Anticoagulation options for patients with heparin-induced thrombocytopenia requiring renal support in the intensive care unit. Contrib Nephrol. 2007;17:259–266. doi: 10.1159/000102110. [DOI] [PubMed] [Google Scholar]
- National Kidney Foundation. KDOQI clinical practice guidelines for vascular access. Am J Kidney Dis. 2006;17(Suppl 1):S248–S273. doi: 10.1053/j.ajkd.2006.04.040. [DOI] [PubMed] [Google Scholar]
- O'Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, Masur H, McCormick RD, Mermel LA, Pearson ML, Raad II, Randolph A, Weinstein RA. Healthcare Infection Control Practices Advisory Committee. Guidelines for the prevention of intravascular catheter-related infections. Infect Control Hosp Epidemiol. 2002;17:759–769. doi: 10.1086/502007. [DOI] [PubMed] [Google Scholar]
- Leblanc M, Fedak S, Mokris G, Paganini EP. Blood recirculation in temporary central catheters for acute hemodialysis. Clin Nephrol. 1996;17:315–319. [PubMed] [Google Scholar]
- Little MA, Conlon PJ, Walshe JJ. Access recirculation in temporary hemodialysis catheters as measured by the saline dilution technique. Am J Kidney Dis. 2000;17:1135–1139. doi: 10.1053/ajkd.2000.19821. [DOI] [PubMed] [Google Scholar]
- Marschall J, Mermel LA, Classen D, Arias KM, Podgorny K, Anderson DJ, Burstin H, Calfee DP, Coffin SE, Dubberke ER. et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;17(Suppl 1):S22–S30. doi: 10.1086/591059. [DOI] [PubMed] [Google Scholar]
- Pratt RJ, Pellowe CM, Wilson JA, Loveday HP, Harper PJ, Jones SR, McDougall C, Wilcox MH. epic2: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2007;17(Suppl 1):S1–S64. doi: 10.1016/S0195-6701(07)60002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C, Thomas S. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;17:361. doi: 10.1136/bmj.327.7411.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;17:2053–2058. doi: 10.1097/00003246-199612000-00020. [DOI] [PubMed] [Google Scholar]
- Karakitsos D, Labropoulos N, De Groot E, Patrianakos AP, Kouraklis G, Poularas J, Samonis G, Tsoutsos DA, Konstadoulakis MM, Karabinis A. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;17:R162. doi: 10.1186/cc5101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung J, Duffy M, Finckh A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Ann Emerg Med. 2006;17:540–547. doi: 10.1016/j.annemergmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Alonso A, Lau J, Jaber BL. Biocompatible hemodialysis membranes for acute renal failure. Cochrane Database Syst Rev. 2008;17:CD005283. doi: 10.1002/14651858.CD005283.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabindranath K, Adams J, Macleod AM, Muirhead N. Intermittent versus continuous renal replacement therapy for acute renal failure in adults. Cochrane Database Syst Rev. 2007;17:CD003773. doi: 10.1002/14651858.CD003773.pub3. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Berthiaume LR, Delaney A, Bellomo R. Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: a meta-analysis. Crit Care Med. 2008;17:610–617. doi: 10.1097/01.CCM.0B013E3181611F552. [DOI] [PubMed] [Google Scholar]
- Pannu N, Klarenbach S, Wiebe N, Manns B, Tonelli M. Renal replacement therapy in patients with acute renal failure: a systematic review. JAMA. 2008;17:793–805. doi: 10.1001/jama.299.7.793. [DOI] [PubMed] [Google Scholar]
- Kielstein JT, Schiffer M, Hafer C. Back to the future: extended dialysis for treatment of acute kidney injury in the intensive care unit. J Nephrol. 2010;17:494–501. [PubMed] [Google Scholar]
- Davenport A. Continuous renal replacement therapies in patients with acute neurological injury. Semin Dial. 2009;17:165–168. doi: 10.1111/j.1525-139X.2008.00548.x. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Peets AD, Hameed M, Boiteau PJ, Laupland KB, Doig CJ. Dialysis disequilibrium syndrome: brain death following hemodialysis for metabolic acidosis and acute renal failure - a case report. BMC Nephrol. 2004;17:9. doi: 10.1186/1471-2369-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CM, Lin JW, Tsai JT, Ko CP, Hung KS, Hung CC, Su YK, Wei L, Chiu WT, Lee LM. Intracranial pressure fluctuation during hemodialysis in renal failure patients with intracranial hemorrhage. Acta Neurochir Suppl. 2008;17:141–144. doi: 10.1007/978-3-211-78205-7_24. [DOI] [PubMed] [Google Scholar]
- Ronco C, Bellomo R, Brendolan A, Pinna V, La Greca G. Brain density changes during renal replacement in critically ill patients with acute renal failure. Continuous hemofiltration versus intermittent hemodialysis. J Nephrol. 1999;17:173–178. [PubMed] [Google Scholar]
- Barenbrock M, Hausberg M, Matzkies F, de la Motte S, Schaefer RM. Effects of bicarbonate- and lactate-buffered replacement fluids on cardiovascular outcome in CVVH patients. Kidney Int. 2000;17:1751–1757. doi: 10.1046/j.1523-1755.2000.00336.x. [DOI] [PubMed] [Google Scholar]
- McLean AG, Davenport A, Cox D, Sweny P. Effects of lactate-buffered and lactate-free dialysate in CAVHD patients with and without liver dysfunction. Kidney Int. 2000;17:1765–1772. doi: 10.1046/j.1523-1755.2000.00338.x. [DOI] [PubMed] [Google Scholar]
- Association for the Advancement of Medical Instrumentation. Water for Hemodialysis and Related Therapies. Arlington, VA: AAMI; 2010. ANSI/AAMI/ISO 13959:2009. [Google Scholar]
- Association for the Advancement of Medical Instrumentation. Concentrates for Hemodialysis and Related Therapies. Arlington, VA: AAMI; 2011. ANSI/AAMI/ISO 13958:2009. [Google Scholar]
- Association for the Advancement of Medical Instrumentation. Quality of Dialysis Fluid for Hemodialysis and Related Therapies. Arlington, VA: AAMI; 2010. ANSI/AAMI/ISO 11663:2009. [Google Scholar]
- Evanson JA, Himmelfarb J, Wingard R, Knights S, Shyr Y, Schulman G, Ikizler TA, Hakim RM. Prescribed versus delivered dialysis in acute renal failure patients. Am J Kidney Dis. 1998;17:731–738. doi: 10.1016/S0272-6386(98)70127-1. [DOI] [PubMed] [Google Scholar]
- Evanson JA, Ikizler TA, Wingard R, Knights S, Shyr Y, Schulman G, Himmelfarb J, Hakim RM. Measurement of the delivery of dialysis in acute renal failure. Kidney Int. 1999;17:1501–1508. doi: 10.1046/j.1523-1755.1999.00355.x. [DOI] [PubMed] [Google Scholar]
- Paganini EP, Tapolyai M, Goormastic M, Halstenberg WK, Kozlowski L. Establishing a dialysis therapy/patient outcome link in intensive care unit acute dialysis for patients with acute renal failure. Am J Kidney Dis. 1996;17(Suppl 3):S81–S89. [Google Scholar]
- Schiffl H. Disease severity adversely affects delivery of dialysis in acute renal failure. Nephron Clin Pract. 2007;17:c163–c169. doi: 10.1159/000110592. [DOI] [PubMed] [Google Scholar]
- Schiffl H, Lang SM, Fischer R. Daily hemodialysis and the outcome of acute renal failure. N Engl J Med. 2002;17:305–310. doi: 10.1056/NEJMoa010877. [DOI] [PubMed] [Google Scholar]
- Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;17:422–427. doi: 10.1038/ki.2009.159. [DOI] [PubMed] [Google Scholar]
- Faulhaber-Walter R, Hafer C, Jahr N, Vahlbruch J, Hoy L, Haller H, Fliser D, Kielstein JT. The Hannover Dialysis Outcome study: comparison of standard versus intensified extended dialysis for treatment of patients with acute kidney injury in the intensive care unit. Nephrol Dial Transplant. 2009;17:2179–2186. doi: 10.1093/ndt/gfp035. [DOI] [PubMed] [Google Scholar]
- Gotch FA, Sargent JA. A mechanistic analysis of the National Cooperative Dialysis Study (NCDS) Kidney Int. 1985;17:526–534. doi: 10.1038/ki.1985.160. [DOI] [PubMed] [Google Scholar]


