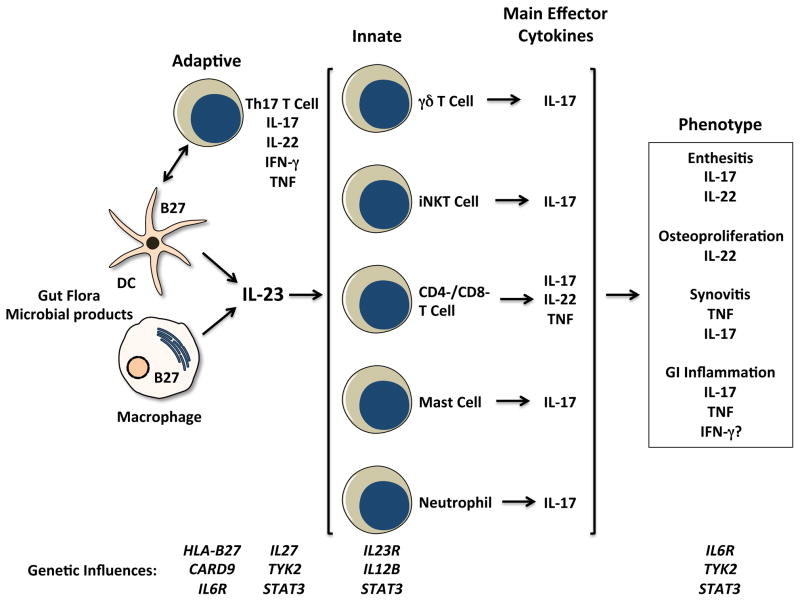
Figure 1.
Schematic depicting cells, effector cytokines, and possible contributions to spondyloarthritis (SpA) pathogenesis. Dendritic cells (DC) and macrophages are major sources of IL-23, which is produced in response to microbes and their products signaling through pattern recognition receptors. Consequences of HLA-B27 misfolding and ER stress can augment IL-23 and IL-1α production, and CARD9 variants could affect production of this cytokine as well. Cells of the adaptive and innate immune response are implicated in SpA pathogenesis. CD4+ Th17 T cell expansion has been reported, KIR3DL2+ cells may be triggered by surface HLA-B27 dimers to produce IL-17. Th17 development and survival may be influenced by variants of the IL-23 and IL-6 receptors (IL23R, IL6R), as well as IL-27 and TYK2- and STAT3-mediated cytokine responses. Tissue inflammation in SpA involves innate immune IL-17-expressing mast cells (synovium), neutrophils (facet joints), and CD3+CD4-CD8- entheseal-resident T cells. The latter produce IL-22, which can drive osteoproliferation in rodent models. Variants in IL6R, TYK2, and STAT3 may affect tissue responses to cytokines.