Abstract
Purpose:
The aim of this study was to evaluate the tissue stiffness of solid pancreatic lesions by using acoustic radiation force impulse (ARFI) elastography to differentiate benign from malignant pancreatic lesions.
Methods:
ARFI elastography was performed in 26 patients who had 27 focal solid pancreatic lesions, including 8 benign lesions (mass-forming pancreatitis, 5; autoimmune pancreatitis, 3) and 19 malignant lesions (pancreatic adenocarcinoma, 16; metastasis from colorectal cancer, 2; malignant neuroendocrine tumor, 1). On the elastographic images of virtual touch tissue imaging (VTI), the echogenicity of the mass was categorized on a 5-grade scale. On the elastographic image of virtual touch tissue quantification (VTQ), the shear wave velocities (SWVs) of the lesion and surrounding parenchyma were measured.
Results:
On the VTI images, the mean echogenicity score of the malignant lesions (3.7±1.0) was higher than that of the benign lesions (3.1±0.4; P=0.023). On the VTQ images, there were no statistical differences in the mean SWV between the benign (2.4±1.1 m/sec) and malignant (3.3±1.0 m/sec) lesions (P=0.101). However, the mean SWV difference values between the lesion and background parenchyma of the malignant lesions (1.5±0.8 m/sec) were higher than those of the benign lesions (0.4±0.3 m/sec; P=0.011).
Conclusion:
ARFI elastography can determine the relative stiffness between a lesion and the background pancreatic parenchyma using VTI and VTQ, which is helpful in the differentiation between benign and malignant solid pancreatic lesions.
Keywords: Ultrasonography, Elasticity imaging Techniques, Pancreas, Pancreatic neoplasms
Introduction
Ultrasonography (US) is a useful imaging modality for detection of focal pancreatic lesions. To characterize the lesions and determine malignancy, however, its role is limited; differentiation between pancreatic cancer and mass-forming pancreatitis is challenging in many cases encountered in daily practice [1].
Elastography is a method for visualizing the elastic properties of tissue using ultrasound. This technology is divided into strain elastography to visualize the tissue deformation induced by external compression and shear wave elastography, which estimates the shear wave velocity generated using an acoustic push pulse [2]. Initial clinical applications of strain elastography have focused on superficial organs such as the breast, thyroid, and prostate. Many investigators have reported that elastography was helpful in differentiating between benign and malignant tumors and that it improved the specificity of the US [3-9].
Recently, acoustic radiation force impulse (ARFI) elastography has emerged as a new method for measuring the stiffness of deep tissue, making transcutaneous elastography of the pancreas more feasible as a result. Pancreatic applications of US elastography are relatively recent because of the difficulty in pressing the pancreas, which is located deep in the body. Endoscopic ultrasound (EUS) elastography is rather widely used for diagnostic purposes, and its effectiveness has been well documented [10-14]. Transcutaneous elastography of the pancreas has been discussed in several studies, but the efficacy of this technique has yet to be proven due to small sample sizes [15,16].
Pancreatic ductal adenocarcinoma is a firm mass, owing to the presence of fibrosis and a marked desmoplastic reaction [17]. Focal pancreatitis is also characterized by fibrosis but manifests with varying patterns according to the degree of atrophy and fibrosis of the lesion and adjacent parenchyma, depending on the acute or chronic stages. We hypothesized that elastography could be helpful in the differentiation of solid pancreatic lesions based on these histological characteristics. This study was aimed at evaluating the feasibility of ARFI elastography in differentiating benign from malignant solid pancreatic masses.
Materials and Methods
Patients
Permission from the Institutional Review Board (IRB) at our institution was granted to perform this review and analysis. The IRB waived the requirement for informed consent for this retrospective study. We retrospectively identified a total of 29 patients with focal solid pancreatic lesions who underwent ARFI elastography, with the diagnosis confirmed by histopathologic examinations after surgical resection or US-guided biopsy between May 2010 and March 2013 by searching the medical databases. Three patients were excluded from the study due to technical failure from the patient’s inability to hold his or her breath properly.
Thus, our study population consisted of a total 26 patients (16 males, 10 females). There were 27 lesions included in this study because one patient with mass-forming pancreatitis had two lesions. The pancreatic lesions included 8 benign lesions (mass-forming pancreatitis, 5; autoimmune pancreatitis, 3) and 19 malignant lesions (pancreatic adenocarcinoma, 16; metastasis from colorectal cancer, 2; malignant neuroendocrine tumor, 1). The mean age of the benign group and malignant group was 62 years (range, 51 to 81 years) and 57 years (range, 37 to 75 years), respectively.
Image Acquisition and Analysis
All of the patients underwent conventional abdominal US and ARFI scans, and a radiologist (JHC) with 17 years' experience of abdominal US conducted all of the examinations. Siemens Acuson S2000 CDFI (Siemens, Mountain View, CA, USA) and ARFI imaging technology using a 4C1 convex array probe with a frequency of 2.0-4.0 MHz were used in this study. Two kinds of ARFI elastography imaging studies, virtual touch tissue imaging (VTI) and virtual touch tissue quantification (VTQ), were performed and analyzed to assess the qualitative and quantitative lesion stiffness. When ARFI scanning was performed, the patient was asked to stop breathing for a moment for accurate and reproducible estimation.
A VTI image visualizes the relative stiffness in the selected region of interest (ROI) with a gray-scale map. It uses a dual imaging screen with the left screen showing the B-mode image and the right screen showing the elastographic image. Tissue softness is portrayed by high echogenicity and hardness by low echogenicity [18,19]. In this study, the echogenicity of the lesion was scored on a 5-grade scale to determine lesion stiffness relative to the adjacent pancreatic parenchymal echogenicity: very hyperechoic (1 point, white), hyperechoic (2 points, light gray), isoechoic (3 points, gray), hypoechoic (4 points, patchy black), and very hypoechoic (5 points, dark black). A higher score denotes stiffer tissue (Fig. 1). All of the results were agreed upon by two radiologists who were blinded to the pathological and clinical data.
Fig. 1. Representative virtual touch tissue imaging (VTI) for each echogenicity score.
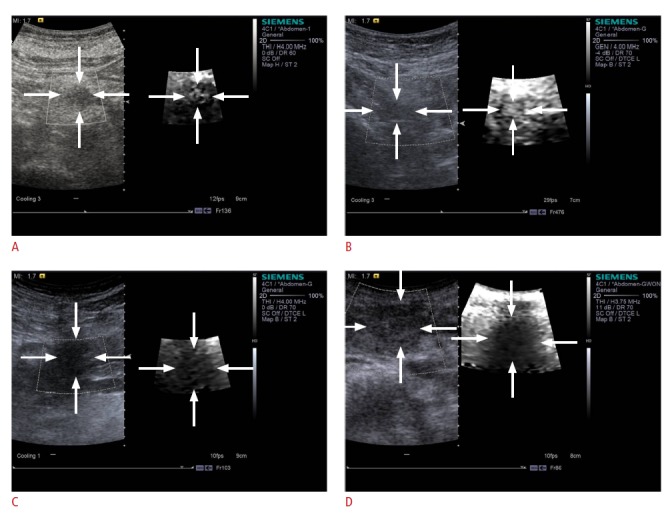
A. On a VTI image, a score 2 lesion appears to have a light gray color. B. On a VTI image, a score 3 lesion has a gray color. C. On a VTI image, a score 4 lesion appears to have a patchy black color. D. On a VTI image, a score 5 lesion appears dark black.
The VTQ image measures the shear wave velocity (m/sec) of the lesion by placing the ROI within the lesion tissues. The stiffer the tissue, the faster the shear waves propagate. Thus it provides numerical measurements about tissue elasticity properties [18, 19]. The value is objective and reproducible as a quantitative indicator. Therefore, it can be used for comparison with the tissue elasticity properties of other patients, without taking the hardness of adjacent parenchyma into consideration [20]. In this study, the shear wave velocity (m/sec) was measured in the ROI of the lesion and surrounding parenchyma five times each. The mean value (±SD) was calculated from a total of three scores excluding the highest and lowest scores. The ROI was located within the mass, without including any vessels or biliary structures. The necrotic, cystic, hemorrhagic, or calcified portion should not be included in the ROI. The surrounding pancreatic parenchyma was also measured, with the ROI located 2-3 cm from the focal lesion, taking care not to include any vessels or biliary structures.
Statistical Analysis
The statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The mean sizes of the benign and malignant lesions were compared with each other with the use of a t-test. Comparisons of the mean echogenicity score in the VTI image, mean shear wave velocitie (SWV, m/sec) of the lesion and surrounding parenchyma, mean SWV difference value (=mean SWV of the lesion-parenchymal mean SWV, m/sec) in the VTQ image between benign and malignant lesions were performed by a Mann-Whitney U-test. Differences were considered significant at P<0.05. Correlations between the SWV and lesion size were tested using Spearman’s correlation coefficient.
Results
The mean maximum diameter of the benign group and malignant group was 2.5 cm (range, 1.1 to 10.3 cm) and 2.9 cm (range, 1.2 to 7.4 cm), respectively. There was no significant difference in the mean maximum diameter between the benign and malignant liver lesions (P=0.303).
On the VTI images, the mean echogenicity score of the malignant lesions (3.7±1.0) appeared higher compared with that of the benign lesions (3.1±0.4; P=0.023) (Table 1, Figs. 2-4). On the VTQ images, there were no statistical differences in the mean SWV between the benign (2.4±1.1 m/sec) and malignant (3.3±1.0 m/sec) lesions (P=0.101) (Table 1, Fig. 5A). However, the mean SWV difference values between the lesion and background parenchyma of the malignant lesions (1.5±0.8 m/sec) were higher than those of the benign lesions (0.4±0.3 m/sec; P=0.011) (Table 1, Figs. 3, 4, 5B).
Table 1.
Comparison of the acoustic radiation force impulse values in the benign and malignant groups
| Variable | Benign | Malignant | P-value |
|---|---|---|---|
| Mean echogenicity score | 3.1±0.4 (2–4) | 3.7±1.0 (2–5) | 0.023 |
| Mean SWV of the mass (m/sec) | 2.4±1.1 (0.9–3.7) | 3.3±1.0 (1.3–4.8) | 0.101 |
| Parenchymal mean SWV (m/sec) | 2.11±0.8 (1.2–3.4) | 1.55±0.6 (0.9–3.8) | 0.121 |
| Mean SWV difference valuea) (m/sec) | 0.4±0.3 (0.1–1.6) | 1.5±0.8 (0.3–3.4) | 0.011 |
SWV, shear wave velocity.
Mean SWV difference value (m/sec)=mean SWV of the mass (m/sec)-parenchymal mean SWV (m/sec).
Fig. 2. Comparison of the virtual touch tissue imaging values of the benign and malignant groups.
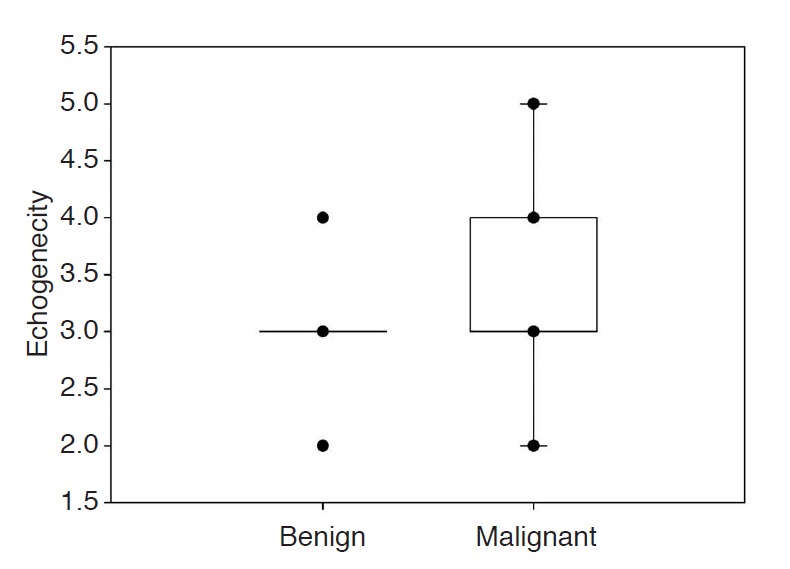
The mean echogenicity score for the benign group and malignant group were 3.1±0.4 and 3.7±1.0, respectively (P=0.023).
Fig. 4. A 67-year-old woman with pancreatic adenocarcinoma.
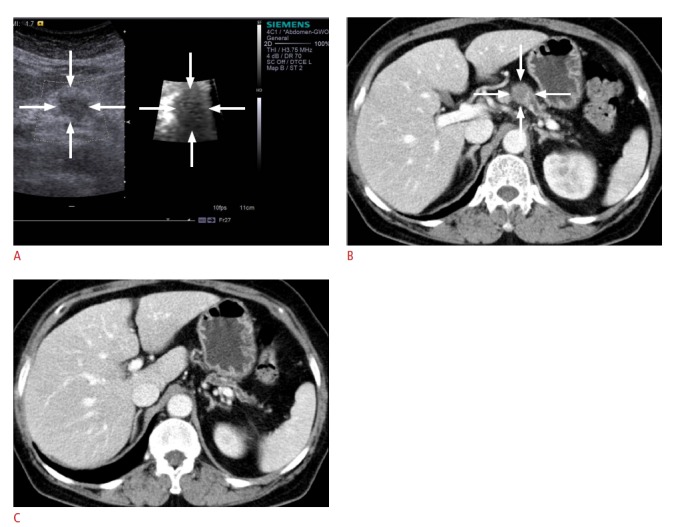
A. On a conventional B-mode image, the lesion appears as an illdefined hypoechoic mass (left image). On a virtual touch tissue imaging elastographic image, the lesion appears to be stiffer than the surrounding pancreatic parenchyma (echogenicity score, 4; right image). The shear wave velocity of the lesion and surrounding pancreatic parenchyma was 4.85 m/sec and 2.23 m/sec, respectively. B, C. Axial computed tomography scans show an ill-defined hypodense mass in the pancreatic body, distal p-duct dilatation, and parenchymal atrophy, suggesting pancreatic cancer.
Fig. 5. Comparison of virtual touch tissue quantification values of the benign and malignant groups.
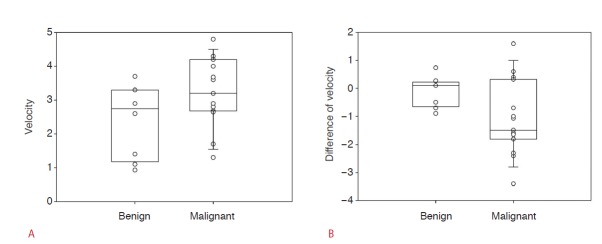
A. The mean shear wave velocity (SWV; m/sec) for the benign group and malignant group were 2.4±1.1 and 3.3±1.0, respectively (P=0.101). B. The mean shear wave velocity difference value (SWV of lesion-SWV of normal parenchyma) for the benign group and malignant group were 0.4±0.3 and 1.5±0.8, respectively (P=0.011).
Fig. 3. A 62-year-old woman with focal pancreatitis.
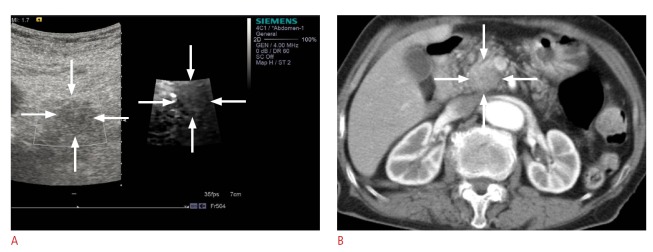
A. On a conventional B-mode image, the lesion appears as a hypoechoic mass (left image). On a virtual touch tissue imaging elastographic image, the lesion shows a stiffness similar to the surrounding pancreatic parenchyma (echogenicity score, 3) (right image). The shear wave velocity of the lesion and surrounding pancreatic parenchyma was 2.08 m/sec and 2.02 m/sec, respectively. B. Axial computed tomography scan shows an ill-defined hypodense mass in the pancreatic head region.
The mean ARFI value of the extra-lesional pancreatic parenchyma was 1.78 m/sec. The malignant group (1.55±0.6 m/sec) showed a higher ARFI value than the benign groups (2.11±0.8 m/sec), although the difference was not statistically significant (Table 1). The SWV was independent of lesion size (Spearman correlation coefficient, -0.178; P=0.416).
Discussion
Regarding the transcutaneous or EUS elastography in the assessment of focal pancreatic lesions, some earlier studies analyzing elastographic patterns were rather inconclusive due to the subjectivity of the interpretation of the color map and a lack of reliability and consistency [10,11,13,15]. On the other hand, Itokawa et al. [21] asserted that strain elastography during EUS effectively determined the strain ratio of the pancreatic cancer to be significantly higher than that of mass-forming pancreatitis in a study using quantitative second-generation strain elastography followed by a multicenter study showing high accuracy of about 80%-90% [22]. However, EUS is invasive and not easy for the patient because sedation is required. In addition, there are some technical limitations because it is difficult to control the compression of a target tissue by endoscopic probe or to exclude the very soft or hard tissues of adjacent structures like the heart, major vessels, and vertebrae in a selected ROI. Furthermore, undesirable results can be expected when a lesion is larger than 3 cm or deeply seated and can be affected by motion artifacts such as those from breathing or the heartbeat [13].
Several studies on transcutaneous elastography of the pancreas have been published in the recent literature but with limited validity. Uchida et al. [15] reported that the lesion detection rate and diagnostic rate could be improved to over 90% by the combined use of B-mode and elastographic images, compared to using B-mode images alone. Kawada et al. [16] analyzed the elastographic patterns of three benign masses and 30 malignant masses in terms of the predominant color and color distribution and reported that 90% of ductal adenocarcinoma cases, particularly all of them over 25 mm in size, were characterized by blue color patterns and 72% of them showed a heterogeneous distribution. In their study, the mean strain ratio of the ROI placed over a mass to the ROI over the adjacent parenchyma was 4.15 for the benign masses and 12.16 for the malignant masses, although the difference was not statistically significant (P=0.234), which might be limited by the small number of benign lesions [16].
ARFI is a kind of shearwave elastography. It provides information about tissue stiffness by focusing high-intensity acoustic pulses on a target area using a conventional ultrasound probe to propagate shear waves and detect the tissue's response by using a tracking pulse emitted by numerous transmission channels [19]. It enables operators to measure tissue elasticity in the desired region by monitoring real-time anatomical details provided by the B-mode image, as well as perform quick assessment. Since it does not use external compression, image acquisition is less affected by the operator, including the degree of force the operator uses to press the probe, and allows quantitative measurement of tissue, including elasticity and speed. High reproducibility is another advantage of ARFI [20,23]. In addition, transcutaneous elastography of the pancreas with ARFI scanning is less invasive than EUS and does not require sedation of the patient during examination. It is also easy to use without a delayed setup period during conventional B-mode ultrasonography [24,25].
According to earlier studies investigating the role of ARFI, the mean ARFI value for normal pancreatic parenchyma was approximately 1.28 to 1.40 m/sec [26,27]. In the present study, the mean ARFI value for extra-lesional pancreatic parenchyma was 1.78 m/sec; and the benign group showed a higher ARFI value than the malignant group, although the difference was not statistically significant. Although pancreatic cancer is a firm mass characterized by high ARFI values, the distribution of ARFI values varied among studies and the number of studies was limited [28]. Chronic pancreatitis, the most important disease entity for differential diagnosis from pancreatic adenocarcinoma, is also commonly accompanied by fibrosis and calcification, leading to high ARFI values [26,29].
In the present study, the relative stiffness of a lesion to the adjacent parenchyma was significantly higher in the malignant group than in the benign group on both VTI and VTQ images. The stiffness of extra-lesional pancreatic parenchyma was also higher in the benign group than the malignant group. This means that fibrosis and calcification that developed not only in the lesion but also in the surrounding parenchyma in the benign group resulted in higher stiffness than would be found in normal parenchyma, making the difference in stiffness between the lesion and surrounding parenchyma insignificant. Based on the results of the present study, because both pancreatic adenocarcinoma and mass-forming chronic pancreatitis are characterized by hardness, the relative stiffness of a lesion to its adjacent parenchyma can be expected to provide more accurate information than the absolute ARFI value of a lesion.
This study has several limitations. First of all, a smaller number of subjects with benign lesions, that is, mass-forming pancreatitis, than those with pancreatic adenocarcinoma made it difficult to generalize the results of the study. Further research needs to include a larger number of patients with benign lesions. Regarding the technical limitations, ARFI is a static image that is sensitive to motion during measurement; thus it is not effective in examining patients with a lesion near a large blood vessel and those who have difficulty sustaining a breath hold. Five-time sampling would not be enoughfor obtaining conclusive results.
In conclusion, ARFI elastography identified relative stiffness values between the lesion and background pancreatic parenchyma using VTI and VTQ, which could be helpful in differentiating malignant tumors from benign inflammatory lesions, although there was a considerable degree of overlap between the ARFI values of the benign and malignant lesions.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Reference
- 1.D'Onofrio M, Zamboni G, Tognolini A, Malago R, Faccioli N, Frulloni L, et al. Mass-forming pancreatitis: value of contrast-enhanced ultrasonography. World J Gastroenterol. 2006;12:4181–4184. doi: 10.3748/wjg.v12.i26.4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ophir J, Cespedes I, Ponnekanti H, Yazdi Y, Li X. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrasonic Imaging. 1991;13:111–134. doi: 10.1177/016173469101300201. [DOI] [PubMed] [Google Scholar]
- 3.Garra BS, Cespedes EI, Ophir J, Spratt SR, Zuurbier RA, Magnant CM, et al. Elastography of breast lesions: initial clinical results. Radiology. 1997;202:79–86. doi: 10.1148/radiology.202.1.8988195. [DOI] [PubMed] [Google Scholar]
- 4.Lorenz A, Sommerfeld HJ, Garcia-Schurmann M, Philippou S, Senge T, Ermert H. A new system for the acquisition of ultrasonic multicompression strain images of the human prostate in vivo. IEEE Trans Ultrason Ferroelectr Freq Control. 1999;46:1147–1154. doi: 10.1109/58.796120. [DOI] [PubMed] [Google Scholar]
- 5.Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–350. doi: 10.1148/radiol.2391041676. [DOI] [PubMed] [Google Scholar]
- 6.Cochlin DL, Ganatra RH, Griffiths DF. Elastography in the detection of prostatic cancer. Clin Radiol. 2002;57:1014–1020. doi: 10.1053/crad.2002.0989. [DOI] [PubMed] [Google Scholar]
- 7.Lyshchik A, Higashi T, Asato R, Tanaka S, Ito J, Mai JJ, et al. Thyroid gland tumor diagnosis at US elastography. Radiology. 2005;237:202–211. doi: 10.1148/radiol.2363041248. [DOI] [PubMed] [Google Scholar]
- 8.Goddi A, Bonardi M, Alessi S. Breast elastography: a literature review. J Ultrasound. 2012;15:192–198. doi: 10.1016/j.jus.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dighe M, Luo S, Cuevas C, Kim Y. Efficacy of thyroid ultrasound elastography in differential diagnosis of small thyroid nodules. Eur J Radiol. 2013;82:e274–e280. doi: 10.1016/j.ejrad.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Janssen J, Schlörer E, Greiner L. EUS elastography of the pancreas: feasibility and pattern description of the normal pancreas, chronic pancreatitis, and focal pancreatic lesions. Gastrointest Endosc. 2007;65:971–978. doi: 10.1016/j.gie.2006.12.057. [DOI] [PubMed] [Google Scholar]
- 11.Hirche TO, Ignee A, Barreiros AP, Schreiber-Dietrich D, Jungblut S, Ott M, et al. Indications and limitations of endoscopic ultrasound elastography for evaluation of focal pancreatic lesions. Endoscopy. 2008;40:910–917. doi: 10.1055/s-2008-1077726. [DOI] [PubMed] [Google Scholar]
- 12.Saftoiu A, Vilmann P, Gorunescu F, Gheonea DI, Gorunescu M, Ciurea T, et al. Neural network analysis of dynamic sequences of EUS elastography used for the differential diagnosis of chronic pancreatitis and pancreatic cancer. Gastrointest Endosc. 2008;68:1086–1094. doi: 10.1016/j.gie.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 13.Iglesias-Garcia J, Larino-Noia J, Abdulkader I, Forteza J, Dominguez-Munoz JE. EUS elastography for the characterization of solid pancreatic masses. Gastrointest Endosc. 2009;70:1101–1108. doi: 10.1016/j.gie.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 14.Iglesias-Garcia J, Larino-Noia J, Abdulkader I, Forteza J, Dominguez-Munoz JE. Quantitative endoscopic ultrasound elastography: an accurate method for the differentiation of solid pancreatic masses. Gastroenterology. 2010;139:1172–1180. doi: 10.1053/j.gastro.2010.06.059. [DOI] [PubMed] [Google Scholar]
- 15.Uchida H, Hirooka Y, Itoh A, Kawashima H, Hara K, Nonogaki K, et al. Feasibility of tissue elastography using transcutaneous ultrasonography for the diagnosis of pancreatic diseases. Pancreas. 2009;38:17–22. doi: 10.1097/MPA.0b013e318184db78. [DOI] [PubMed] [Google Scholar]
- 16.Kawada N, Tanaka S, Uehara H, Takakura R, Katayama K, Fukuda J, et al. Feasibility of second-generation transabdominal ultrasound- elastography to evaluate solid pancreatic tumors: preliminary report of 36 cases. Pancreas. 2012;41:978–980. doi: 10.1097/MPA.0b013e3182499b84. [DOI] [PubMed] [Google Scholar]
- 17.Korc M. Pancreatic cancer associated stroma production. Am J Surg. 2007;194(4 Suppl):s84–s86. doi: 10.1016/j.amjsurg.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhai L, Palmeri ML, Bouchard RR, Nightingale RW, Nightingale KR. An integrated indenter-ARFI imaging system for tissue stiffness quantification. Ultrason Imaging. 2008;30:95–111. doi: 10.1177/016173460803000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palmeri ML, Wang MH, Dahl JJ, Frinkley KD, Nightingale KR. Quantifying hepatic shear modulus in vivo using acoustic radiation force. Ultrasound Med Biol. 2008;34:546–558. doi: 10.1016/j.ultrasmedbio.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lupsor M, Badea R, Horia S, Sparchez Z, Branda H, Serban A, et al. Performance of a new elastographic method (ARFI technology) compared to unidimensional transient elastography in the noninvasive assessment of chronic hepatitis C: preliminary results. J Gastrointestin Liver Dis. 2009;18:303–310. [PubMed] [Google Scholar]
- 21.Itokawa F, Itoi T, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, et al. EUS elastography combined with the strain ratio of tissue elasticity for diagnosis of solid pancreatic masses. J Gastroenterol. 2011;46:843–853. doi: 10.1007/s00535-011-0399-5. [DOI] [PubMed] [Google Scholar]
- 22.Saftoiu A, Vilmann P, Gorunescu F, Janssen J, Hocke M, Larsen M, et al. Accuracy of endoscopic ultrasound elastography used for differential diagnosis of focal pancreatic masses: a multicenter study. Endoscopy. 2011;43:596–603. doi: 10.1055/s-0030-1256314. [DOI] [PubMed] [Google Scholar]
- 23.Nightingale K, Soo MS, Nightingale R, Trahey G. Acoustic radiation force impulse imaging: in vivo demonstration of clinical feasibility. Ultrasound Med Biol. 2002;28:227–235. doi: 10.1016/s0301-5629(01)00499-9. [DOI] [PubMed] [Google Scholar]
- 24.Nightingale KR, Palmeri ML, Nightingale RW, Trahey GE. On the feasibility of remote palpation using acoustic radiation force. J Acoust Soc Am. 2001;110:625–634. doi: 10.1121/1.1378344. [DOI] [PubMed] [Google Scholar]
- 25.Friedrich-Rust M, Wunder K, Kriener S, Sotoudeh F, Richter S, Bojunga J. Liver fibrosis in viral hepatitis: non invasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology. 2009;252:595–604. doi: 10.1148/radiol.2523081928. [DOI] [PubMed] [Google Scholar]
- 26.Mateen MA, Muheet KA, Mohan RJ, Rao PN, Majaz HM, Rao GV, et al. Evaluation of ultrasound based acoustic radiation force impulse (ARFI) and eSie touch sonoelastography for diagnosis of inflammatory pancreatic diseases. JOP. 2012;13:36–44. [PubMed] [Google Scholar]
- 27.Gallotti A, D'Onofrio M, Pozzi Mucelli R. Acoustic Radiation Force Impulse (ARFI) technique in ultrasound with Virtual Touch tissue quantification of the upper abdomen. Radiol Med. 2010;115:889–897. doi: 10.1007/s11547-010-0504-5. [DOI] [PubMed] [Google Scholar]
- 28.D'Onofrio M, Crosara S, De Robertis R, Canestrini S, Demozzi E, Pozzi Mucelli R. Elastography of the pancreas. Eur J Radiol. doi: 10.1016/j.ejrad.2013.04.020. 2013 May 28 [Epub]. http://dx.doi.org/10.1016/j.ejrad.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 29.Yashima Y, Sasahira N, Isayama H, Kogure H, Ikeda H, Hirano K, et al. Acoustic radiation force impulse elastography for noninvasive assessment of chronic pancreatitis. J Gastroenterol. 2012;47:427–432. doi: 10.1007/s00535-011-0491-x. [DOI] [PubMed] [Google Scholar]


