Abstract
Background
One of the first chemoprevention trials conducted in the western hemisphere, the National Surgical Adjuvant Breast and Bowel Project’s (NSABP) Breast Cancer Prevention Trial (BCPT), demonstrated the need to evaluate all aspects of recruitment in real time and to implement strategies to enroll racial and ethnic minority women.
Purpose
The purpose of this report is to review various patient recruitment efforts the NSABP developed to enhance the participation of racial and ethnic minority women in the Study of Tamoxifen and Raloxifene (STAR) trial and to describe the role that the recruitment process played in the implementation and understanding of breast cancer risk assessment in minority communities.
Methods
The NSABP STAR trial was a randomized, double-blinded study comparing the use of tamoxifen 20 mg/day to raloxifene 60 mg/day, for a 5-year period, to reduce the risk of developing invasive breast cancer. Eligible postmenopausal women were required to have a 5-year predicted breast cancer risk of 1.66% based on the modified Gail Model. For the current report, eligibility and enrollment data were tabulated by race/ethnicity for women who submitted STAR risk assessment forms (RAFs).
Results
A total of 184,460 RAFs were received, 145,550 (78.9%) from white women and 38,910 (21.1%) from minority women. Of the latter group, 21,444 (11.6%) were from African Americans/blacks, 7913 (4.5%) from Hispanics/Latinas, and 9553 (5.2%) from other racial or ethnic groups. The percentages of risk-eligible women among African Americans, Hispanics/Latinas, others, and whites were 14.2%, 23.3%, 13.7%, and 57.4%, respectively. Programs targeting minority enrollment submitted large numbers of RAFs, but the eligibility rates of the women referred from those groups tended to be lower than the rates among women referred outside of those programs. The average number of completed risk assessments increased among minority women over the course of the recruitment period compared to those from whites.
Limitations
We have not addressed all identified barriers to the recruitment of minorities in clinical research. Our risk assessments and recruitment results do not reflect the modified Gail Model for African Americans.
Conclusions
Recruitment strategies used in STAR for racial and ethnic minorities contributed to doubling the minority enrollment compared to that in the BCPT and increased the awareness of breast cancer risk assessment in minority communities. Incorporation of new information into models to improve the risk estimation of diverse populations should prove beneficial.
Introduction
The Breast Cancer Prevention Trial (BCPT), the first chemoprevention trial to use a breast cancer risk prediction score as an eligibility criterion for trial participation, was completed in 1998 [1]. Conducted by the National Surgical Adjuvant Breast and Bowel Project (NSABP), this trial compared the effectiveness of tamoxifen with that of placebo in preventing the development of breast cancer in 13,388 healthy women at increased risk for the future development of the disease. The results of the BCPT demonstrated that tamoxifen reduces the risk of developing breast cancer by close to 50% and led to the Federal Drug Administration’s (FDA) approval of the drug for that use.
The principles of evidence-based medicine are increasingly being used to improve the practice of medicine, particularly in oncology. Randomized controlled clinical trials are considered the most reliable source of practice-changing information. It is important for such studies to include minority participants and to attempt to improve rates of minority enrollment and to reduce rates of racial and ethnic disparities. Race is a known risk factor for breast cancer, and there are different incidence rates of the disease in different populations. The incidence rates of breast cancer in Hispanic women and postmenopausal African-American women are substantially lower than those of white women. In contrast, African-American women have a higher incidence rate before the age of 45 years and are more likely to die from breast cancer at every age [2,3].
The NSABP explored and implemented strategies to recruit and retain patients from minority and underserved populations. Disappointingly, only 3.5% of the participants in the BCPT study were from racial or ethnic minorities. Published reports of experiences in recruiting minorities to cancer prevention clinical trials with drug interventions were nonexistent at the time [4]. The BCPT demonstrated the need to evaluate the recruitment of minority women in real time and to implement strategies to recruit these patients. Our goals in this article are (1) to review the recruitment efforts developed by the NSABP to enhance the participation of minority women in the second NSABP Breast Cancer Prevention Trial, The Study of Tamoxifen and Raloxifene (STAR), and (2) to describe the role that the recruitment process played in educating the minority community about breast cancer risk assessment. The racial and ethnic classifications tracked during the conduct of the STAR trial included the following: white, Hispanic/Latina, African American/black, and other.
Methods
Design of the study
The STAR trial was a randomized, double-blinded study that compared the use of tamoxifen 20 mg/day to raloxifene 60 mg/day, over a 5-year period, for reducing the risk of developing invasive breast cancer [5]. To be eligible for participation, a woman was required to have a 5-year predicted breast cancer risk of at least 1.66% based on the modified Gail Model, to be at least 35 years of age, and to be postmenopausal [6]. Those 35 years or older with a history of lobular carcinoma in situ (LCIS) treated by local excision only were also eligible. To document the results of the STAR minority recruitment efforts, risk assessment form (RAF) submissions, eligibility, and enrollment were tabulated by race and ethnicity. In addition, characteristics of eligible and enrolled patients were tabulated, as were participant enrollment and Gail Model Score by time.
Clinical considerations for differential risk assessment for minorities
Before the National Cancer Institute’s (NCI) peer-review approval of STAR, data became available about the risks and benefits of tamoxifen in minority populations that affected the planning for recruitment onto STAR. In July 1998, the NCI-sponsored Chantilly Workshop Working Group convened to discuss and develop information for women and health-care providers to use in assessing the risks and benefits of using tamoxifen. Among the topics discussed by experts in cancer-related fields, patients, and advocates were the accuracy and availability of baseline incidence rates for cardiovascular events such as stroke and thromboembolic disease for minority women. Data for these events were deemed critically important for minorities, who have higher incidence rates of cardiovascular diseases that could influence risk/benefit indices for tamoxifen use. The 1999 JNCI article, ‘Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer’ was a product of the Chantilly Working Group [7]. Incidence rates for hip fractures, stroke, and pulmonary emboli (PE) among black women were calculated by multiplying rates in whites (using studies of the predominantly white population of Rochester, MN) by black/white incidence ratios. The incidence ratios were taken from stroke (ICD code nos 430–438.9) mortality ratios computed from Tables 1 to 27 in Vital Statistics of the United States, 1992 [8]. The mortality ratios for pulmonary circulatory failure (ICD code nos 415–417.9), which is caused mainly by PE, were used for pulmonary embolism and deep vein thrombosis (DVT). Endometrial cancer and invasive breast cancer rates were determined from SEER 1991–1995 incidence rates [9]. Cataract rates were estimated from results obtained from women in the placebo arm of the BCPT and total mortality from 1990 US rates. For all other races and ethnicities, incidence rates for white women were used.
A STAR Working Group led by the NCI staff met in May 1999 in Bethesda, Maryland, to review base-line data for PE, stroke, and DVT for black women. Members of the working group included leaders from the NSABP and the Women’s Health Initiative (WHI), practicing oncologists, and experts in cardiovascular disease and risk modeling. The cases of stroke, PE, and DVT in the risk profiles were based on the average rates for white women of the same age group as the minority women. This decision was based on data made available to NSABP from the WHI, and a disclosure of the race and ethnicity rates and risk prediction was noted on the risk profiles. SEER incidence rates for breast cancer in Hispanic/ Latina women were incorporated into the risk prediction tool used for STAR and into the NCI’s web-based NCI Breast Cancer Risk Assessment Tool based upon SEER’s expansion to include more Hispanics [10].
In response to queries related to the efficacy and adverse events from tamoxifen treatment in minority women, the NSABP performed a meta-analysis of 13 adjuvant breast cancer treatment trials to compare the effects of tamoxifen on risk of contralateral breast cancer and thromboembolic events in black and in white women with a history of breast cancer [11]. This study demonstrated no differences between these two groups in the incidence of invasive breast cancer in the contralateral breast or in thromboembolic phenomena in women treated with tamoxifen in the adjuvant setting.
Site selection
The goal in selecting participating sites for the STAR trial was to have a population of women representative of those in the United States, Canada, and Puerto Rico, who were at increased risk for the future development of breast cancer. To participate in STAR, each clinical center was required to submit a competitive application. In addition to describing its experience conducting treatment and prevention trials, each site was required to submit a detailed plan describing recruitment efforts directed at minority and underserved populations.
After review by NSABP and NCI staff, 198 clinical centers and 300 satellite centers were selected. There were centers in all 50 states, most of the Canadian provinces, the District of Columbia, and Puerto Rico. Almost all of the Community Clinical Oncology Program (CCOP) and Minority-Based Community Clinical Oncology Program (MBCCOP) sites were selected. Sites that were not members of the NSABP but that had access to minority populations were encouraged to apply. In addition, an advertisement was placed in the Cancer Letter to recruit sites to STAR. Given the wide geographic distribution of the sites and mixture of urban, suburban, and rural locations, there was substantial access to African-American, Hispanic/Latina, Native American, and Asian populations.
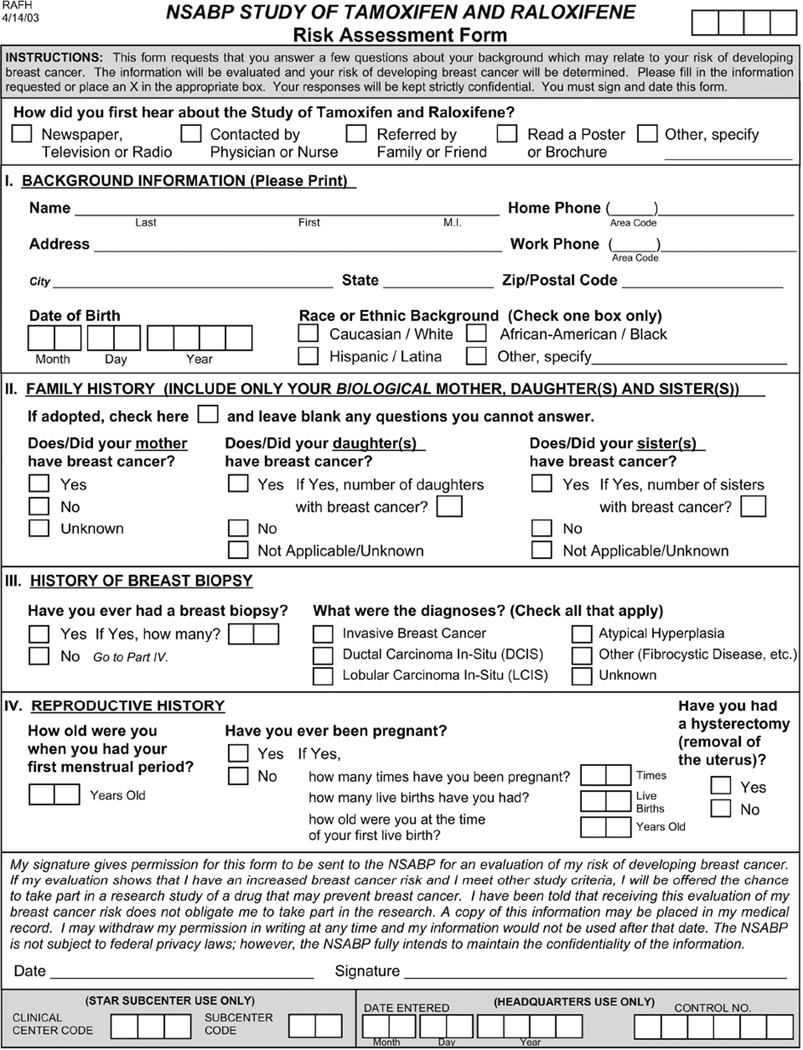
Breast cancer risk assessment
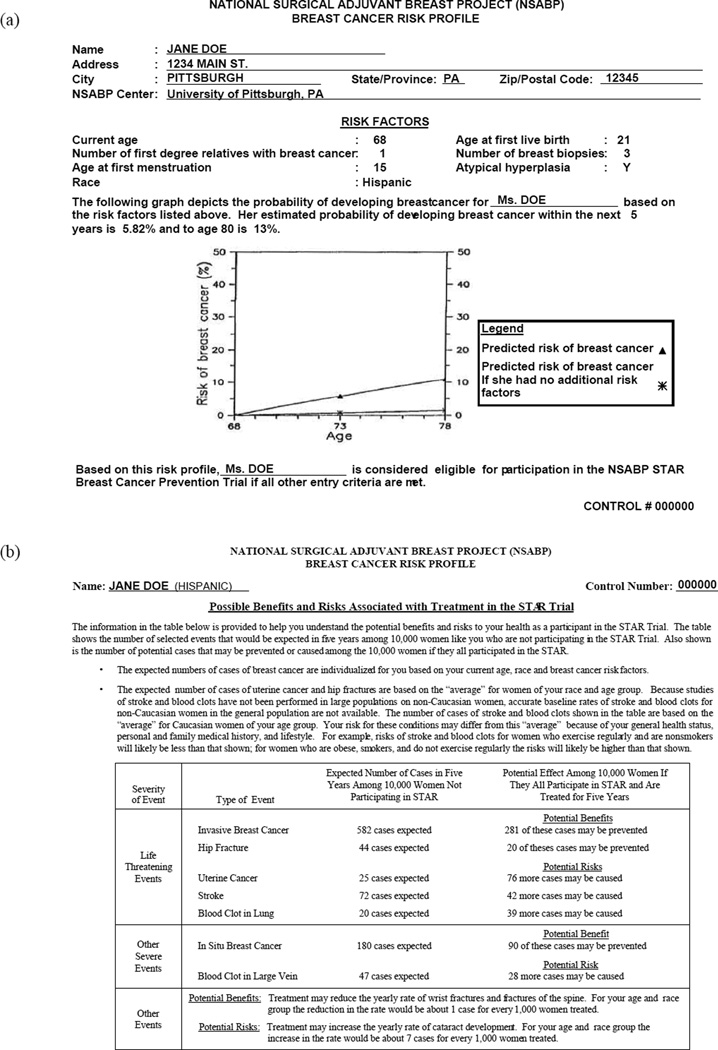
To estimate a woman’s risk of developing breast cancer and to determine whether that risk was sufficient to meet the eligibility requirements to enter STAR, each potential participant was asked to complete a RAF (Figure 1). Included on the form were questions addressing the information necessary to calculate a Gail Model Score: age, race, number of first-degree female relatives with breast cancer, age at first menstrual period, nulliparity or age at first live birth, number of previous benign breast biopsies, and whether any biopsies demonstrated atypical hyperplasia (AH). Completed RAFs were submitted to the NSABP Biostatistical Center, and a Risk Assessment Profile (RAP) was generated and returned to the originating sites within 24–48 h (Figure 2(a)). The RAP information included the woman’s Gail Model Score estimating her risk of developing invasive breast cancer over the next 5 years. Whenever that 5-year risk was 1.66% or greater, she was risk eligible to enter the trial. Five-year and lifetime risk estimates (to the age of 80 years) with a comparison to women of the same age and race but with no additional risk factors were provided for the potential participant.
Figure 1.
RAF.
RAF: risk assessment form.
Figure 2.
(a) Sample RAP and (b) RAP-based on self-identified race/ethnicity.
RAP: Risk Assessment Profile.
The second page of the RAP contained a summary of benefits and risks potentially associated with the treatments in STAR (Figure 2(b)). The information was presented in a format developed at the Chantilly Working Group [4]. The approach used for the benefit/risk assessment was to determine, for each of the events that might be affected by treatment, the number of cases expected to occur over 5 years in a hypothetical population of 10,000 women of the same age, race, and projected breast cancer risk as the individual being evaluated for STAR.
All risk-eligible women who submitted RAFs were offered counseling by health providers (nurses, advanced practice clinicians, and physicians). The NSABP Coordinating Committee for STAR held training sessions for the counselors.
Planned minority recruitment activities during the accrual phase
Minority recruitment activities were directed at NSABP member sites, the general medical community, breast cancer advocates, and the general public. Multiple minority recruitment strategies were implemented at both the national and local levels.
STAR Community Outreach Programs for Education
The STAR Community Outreach Program for Education (SCOPE) was an extension of a pilot program conducted at five centers in the STAR trial to increase minority enrollment. Twenty-four sites were selected from applicants based on their track records in the BCPT and on their access to populations of African Americans, Latinas, Native Americans, or Asians. The objectives of SCOPE were (1) to increase the enrollment of racial and ethnic minority women in STAR, (2) to educate racial and ethnic minority women about breast cancer and breast cancer risk factors, (3) to identify effective minority recruitment strategies for STAR, and (4) to disseminate those strategies to all NSABP member institutions. The SCOPE sites hired full-time community outreach coordinators (COCs) to undertake these tasks. At most sites, the COCs were members of the targeted racial or ethnic minority groups and resided in the communities where they worked. One NSABP CCOP member institution located in Atlanta collaborated with a minority surgeon whose practice was 70% minority. The member institution shared a COC with that physician, which permitted discussion and recruitment to be conducted in the presence of a doctor with whom the patients had developed a trusting relationship. This partnership was successful as an outreach to a community physician not actively engaged in breast cancer prevention and could be replicated in other communities as a successful strategy for enrolling minority women at high risk of breast cancer into prevention trials.
A full-time SCOPE COC at the NSABP Operations Center oversaw the efforts of the individual SCOPE sites and supported minority recruitment efforts at all STAR sites. Materials developed to assist recruitment included STAR brochures; posters; consent forms in English, Spanish, and French; and STAR website postings. The STAR Procedures Manual and Information Handbook addressed all aspects of trial conduct and included an extensive section on enhancing minority accrual.
NSABP member-directed activities
NSABP group meetings were held twice a year and included 2-day STAR workshops at which the importance of minority accrual was addressed. Minority recruitment activities included panel discussions, lectures, breakout sessions, and cultural competency training for investigators.
The NSABP Diversity Strategic Planning Working Group (DSPWG) is composed of health professionals representing racially and ethnically under represented populations in urban, rural, and suburban areas. The DSPWG focuses on enhancing minority participation in NSABP trials and in NSABP membership. The DSPWG developed the ‘Racial and Ethnic Diversity in NSABP Clinical Trials’ and the ‘Cancer Treatment Resources for Minorities Populations’ links on the NSABP website and conducted special training sessions with nationally recognized diversity experts speaking on minority recruitment.
The STAR Participant Advisory Board (PAB) consisted of 18 women of diverse races and ethnicities, economic status, and breast cancer risks, and included cancer survivors and BCPT participants. The PAB met at each NSABP group meeting to discuss general trial issues and to strategize about ways to communicate with different populations about STAR through local and national media and in local recruitment efforts.
Minority enrollment-related issues were incorporated into discussions during the principal investigators’, STAR Steering, Coordinators’, and Administrators’ Committees to reinforce the importance of diversity in the trial. STAR strategy sessions provided unique opportunities to share strategies between sites with and without large minorities. This approach was especially important for sharing ways to educate different populations about breast cancer risk and to provide a forum in which to address protocol and clinical issues raised for women at high risk for breast cancer.
STAR sites received monthly summaries of their overall and minority accrual and number of RAFs submitted. Monthly SCOPE site teleconferences were held during which minority accrual was discussed and best practices shared. STAR newsletters were published during the study and regularly included articles related to minority accrual.
Activities directed at general and minority communities and advocates
A national press release ‘kicked off’ STAR and targeted minority health organizations, medical professionals, and the minority media. In addition to the press conference and national press release at the start of the trial, press releases were developed for Minority Cancer Awareness Week each April. Local press releases also were developed at the time of each national release to highlight local investigators. Numerous STAR investigators made guest appearances on local TV and radio programs to promote the study and to emphasize its importance to all women at risk for the disease but particularly minority women. Articles about STAR and the need for minority women to participate were published in Ebony, Newsweek, and numerous local newspapers.
The STAR protocol chair, protocol officer, and the NCI program director for STAR addressed more than 200 national, regional, and local medical organizations, highlighting the trial and the importance of minority recruitment. The 2000 American Society of Clinical Oncology annual meeting selected the NSABP’s abstract that summarized findings demonstrating no differences in reduction of contralateral breast cancer or thromboembolic events between black and white women to be highlighted for media coverage [8]. The Susan G. Komen for the Cure sponsored a 1.5-day training workshop for SCOPE COCs. Representatives from a dozen minority health organizations also attended the workshop, which was designed to initiate partnerships and to increase awareness of STAR among the organization’s members. The Komen Project Clinical Research Affiliates Funding Trials (CRAFTs) supported several COCs at STAR sites and provided travel funds for attendance at NSABP STAR workshops.
Initiatives developed during STAR
During the 5-year STAR accrual period, total and minority accrual were monitored carefully. Several new recruitment programs designed to enhance minority accrual were developed during STAR.
Native American outreach
One of the SCOPE sites hired a Native American COC with the hope that STAR accrual from that site’s population could be increased substantially. Multiple barriers initially prevented the activation of the STAR trial at this site. In an effort to address these issues, representatives of the SCOPE site, the NSABP, and the NCI met with tribal leaders and the tribal Institutional Review Board (IRB); the NCI staff facilitated the processes for protocol approval between the Indian Health Services and the local tribal IRB. An important component of the discussions with the Indian Health Services was the establishment of a process by which Native American participants would have access to treatment whenever cancer or other outcomes requiring medical attention occurred during or after the trial. Previous non-NCI research studies conducted with this group had created a sense of mistrust. To respect the wishes and culture of the tribe, the NSABP agreed not to identify either the specific participation of this Indian Nation or its geographical location in future publications. In addition, the submission of blood and tumor blocks was not required because this was prohibited by the customs of that tribe. These compromises allowed the activation of the trial at that site. Independently, STAR also was endorsed by the Arizona Inter-Tribal Council without restriction with regard to the conduct of the trial. This endorsement obviated the need to seek approval from each individual tribe to promote STAR. A recruitment primer based on a Native American woman’s experiences and reflections on the future of her grandchildren was developed to help educate Native American women about breast cancer [12].
The National Medical Association
The NSABP obtained support for STAR from the National Medical Association (NMA), the oldest and largest organization representing African-American physicians. This support included the following:
STAR discussions at several NMA annual convention and scientific assemblies;
Articles about STAR published in the NMA news-letter and the Journal of the NMA; and
STAR information provided for Project IMPACT, a federally funded program designed to increase awareness of clinical trials among the NMA membership (http://impact.nmanet.org/about-i-m-p-a-c-t).
In collaboration with NMA Region II in the Philadelphia area and the Eastern Cooperative Oncology Group (ECOG), a pilot program was established to assist primary care NMA members to participate in STAR. Representatives from NSABP, ECOG, and the NCI met with NMA Region II officials and their principal investigator for STAR (an African-American medical oncologist from a nearby cancer center) on a regular basis to promote the study and to address any difficulties. These representatives also made visits to practitioners’ offices to meet with staff and to promote the study. NMA members routinely attended STAR workshops during the study.
Corporate collaborations
In 2000, the NSABP began a collaboration with General Motors Corporation (GM), the largest private employer of African Americans in the United States. Twenty-five percent of GM’s workforce is made up of minorities. This collaboration enabled the NSABP to provide a special GM/STAR brochure to be mailed to more than 133,000 active and retired GM employees and their spouses. GM’s leadership estimated that more than 150,000 (18%) of the 1.2 million individuals covered by their health plan had been treated for cancer. Recipients of GM’s health plan constituted a potential participant pool for STAR; GM personnel actively led a dialogue about health-care awareness. GM’s newsletter, LifeSteps, and a biennial health status survey administered to employees resulted in an audience primed for prevention initiatives.
The STAR brochures were mailed with a letter from the GM medical director encouraging women to become informed about their individual risks of breast cancer. The GM medical director also was a featured speaker at the NSABP’s Group Meeting in 2000. GM was provided with information about participating STAR sites along with assurance that procedures associated with participating in the trial would be covered financially.
Similar corporate collaborations were developed with the Ford Motor Company, the New York City Health and Hospitals Corporation, and the Mary Kay Corporation. These corporate collaborations were sought because of their significant minority work forces and programs in place to increase awareness of good health practices among employees. Other corporations permitted articles promoting the STAR trial to be included in their company newsletters and employee websites.
Results
RAFs
Entry into the STAR trial was a multistep process, and among the first steps to establish participant eligibility was the submission of an RAF (Figure 1). The RAF process began on 21 April 1999 and was discontinued on 31 May 2004. A total of 184,460 RAFs were received during that 60-month period. Among the women who completed RAFs, 145,550 (78.9%) identified themselves as white/Caucasian.
RAFs were submitted by 38,910 minority women (21.1% of the total received): 21,444 (11.6%) African Americans, 7913 (4.3%) Hispanics/Latinas, and 9553 (5.2%) women belonging to ‘other’ racial or ethnic groups. Approximately 5000 women (2.7%) in the ‘other’ category were Native Americans (Table 1). Although the total number of RAFs submitted annually increased from 1999 through 2001 and decreased during 2002 through 2004, the percentage of RAFs submitted by minority women increased during the course of the study from 10.8% in 1999 to 30.8% in 2003, the last full year of recruitment (Table 2). Sites with infrastructure in place (e.g., patient databases) and patients with known breast cancer risk calculations generated a higher percentage of risk-eligible women per RAF submitted.
Table 1.
NSABP STAR recruitment by race/ethnicity
| Completed RAFs | Eligible per completed RAF | Enrolled per eligible RAF | |
|---|---|---|---|
| Whitea | 145,550 (78.9%) | 83,576 (57.4%) | 18,451 (22.1%) |
| African American/blacka | 21,444 (11.6%) | 3035 (14.2%) | 490 (16.1%) |
| Hispanic/Latinaa | 7913 (4.3%) | 1685 (21.3%) | 393 (23.3%) |
| Othera,b | 9553 (5.2%) | 3029 (31.7%) | 413 (13.6%) |
| Total | 184,460 (100.0%) | 91,325 (49.5%) | 19,747 (21.6%) |
RAF: risk assessment form; NSABP: National Surgical Adjuvant Breast and Bowel Project; STAR: Study of Tamoxifen and Raloxifene.
Self-identified.
Approximately 5000 (2.7%) self-identified as Native Americans.
Table 2.
Percent minority RAFs submitted in NSABP STAR trial over timea
| Total RAFs | Minority RAFs | Minority as percent of total | |
|---|---|---|---|
| 1999 | 28,015 | 3013 | 10.8 |
| 2000 | 35,352 | 6989 | 19.8 |
| 2001 | 40,157 | 6622 | 16.5 |
| 2002 | 37,906 | 9708 | 25.6 |
| 2003 | 31,069 | 9580 | 30.8 |
| 2004 | 11,961 | 2998 | 25.1 |
| Total | 184,460 | 38,910 | 21.1 |
RAF: risk assessment form; NSABP: National Surgical Adjuvant Breast and Bowel Project; STAR: Study of Tamoxifen and Raloxifene.
Based on date of entry. Recruitment in 1999 began in July and ended in November 2004.
Risk-eligible women
Of the 184,460 women who submitted RAFs, 91,325 (49.5%) had a modified 5-year Gail Model Score of.1.66% and were considered to be risk eligible to enter the trial. Other eligibility requirements have been published [1]. Only 14.2% of African-American women who submitted RAFs were risk eligible, compared to 57.4% of white women (Table 1).
Risk-eligible women who entered the trial
Of the 91,325 risk-eligible women, 19,747 (21.6% overall, 23.3% Hispanic/Latina, 14.2% African Americans/blacks, 13.7% ‘others’, and 57.4% whites) signed informed consent documents and were assigned randomly to tamoxifen or raloxifene. The percentages of risk-eligible minority women by race who entered the trial varied from a high of 23.3% among Hispanic/Latina women to a low of 13.7% for the ‘other’ category (Table 1).
Participant characteristics of the risk-eligible women and those who entered the trial are shown in Table 3. A higher percentage of white women with biopsy-proven LCIS or AH entered the trial than did minority women in the same groups (LCIS: 49% and 38%, respectively; AH: 42% and 34%, respectively).
Table 3.
Characteristics for risk-eligible and enrolled participants in the NSABP STAR trial
| Minority | White | |||||||
|---|---|---|---|---|---|---|---|---|
| Risk eligible, n = 7749 |
Percentagea | Enrolled, n = 1296 |
Percentageb | Risk eligible, n = 83,576 |
Percentagea | Enrolled, n = 18,451 |
Percentageb | |
| Number of first-degree relatives with breast cancer | ||||||||
| 0 | 2310 | 29.8 | 412 | 17.8 | 29,885 | 35.8 | 5281 | 17.7 |
| 1 | 3761 | 48.5 | 558 | 14.8 | 43,110 | 51.6 | 9766 | 22.7 |
| 2 | 1373 | 17.7 | 256 | 18.6 | 9076 | 10.9 | 2877 | 31.7 |
| >3 | 305 | 3.9 | 70 | 23.0 | 1505 | 1.8 | 527 | 35.0 |
| History of LCIS | ||||||||
| No | 7374 | 95.2 | 1155 | 15.7 | 80,244 | 96.0 | 16,812 | 21.0 |
| Yes | 375 | 4.8 | 141 | 37.6 | 3332 | 4.0 | 1639 | 49.2 |
| History of breast atypical hyperplasia | ||||||||
| No | 6669 | 86.1 | 932 | 14.0 | 73,848 | 88.4 | 14,358 | 19.4 |
| Yes | 1080 | 13.9 | 364 | 33.7 | 9728 | 11.6 | 4093 | 42.1 |
LCIS: lobular carcinoma in situ; NSABP: National Surgical Adjuvant Breast and Bowel Project; STAR: Study of Tamoxifen and Raloxifene.
Percent of total risk-eligible women with the specified characteristic.
Percent of risk-eligible women with specified characteristic who enrolled.
Table 4 shows the numbers of RAFs and risk-eligible women from programs engaged in minority recruitment (MBCCOP without SCOPE; NMA) and new STAR sites that had access to large minority communities (SCOPE). Despite large numbers of submitted RFAs, eligibility at these sites tended to be lower than the overall minority eligibility rates at sites that were not targeted toward minority institutions or programs (Table 4).
Table 4.
Within each program: RAFs completed, women at risk of breast cancer considered eligible, and women at risk of breast cancer enrolled (percentages are based on row totals)
| Race and ethnicity | SCOPE program |
percentage | Non- SCOPE MBCCOPs |
percentage | NMA | percentage | Not in one of these programs |
percentage | total | percentage |
|---|---|---|---|---|---|---|---|---|---|---|
| White | ||||||||||
| RAF completed | 22,062 | 15.2 | 1123 | 0.8 | 27 | 0.0 | 122,338 | 84.0 | 145,550 | 100.0 |
| Eligible | 10,990 | 13.2 | 790 | 1.0 | 13 | 0.0 | 71,783 | 85.9 | 83,576 | 100.0 |
| Enrolled | 2031 | 11.0 | 224 | 1.2 | 0 | 0.0 | 16,196 | 87.8 | 18,451 | 100.0 |
| African American/ black | ||||||||||
| RAF completed | 6860 | 32.0 | 2263 | 10.6 | 1075 | 5.0 | 11,246 | 52.4 | 21,444 | 100.0 |
| Eligible | 768 | 25.3 | 287 | 9.5 | 86 | 2.8 | 1894 | 62.4 | 3035 | 100.0 |
| Enrolled | 109 | 22.2 | 22 | 4.5 | 5 | 1.0 | 354 | 72.2 | 490 | 100.0 |
| Hispanic/Latina | ||||||||||
| RAF completed | 2220 | 28.1 | 863 | 10.9 | 13 | 0.2 | 4817 | 60.9 | 7913 | 100.0 |
| Eligible | 259 | 15.4 | 350 | 20.8 | 2 | 0.1 | 1074 | 63.7 | 1685 | 100.0 |
| Enrolled | 57 | 14.5 | 86 | 21.9 | 0 | 0.0 | 250 | 63.6 | 393 | 100.0 |
| Other | ||||||||||
| RAF completed | 5599 | 58.6 | 597 | 6.2 | 12 | 0.1 | 3345 | 35.0 | 9553 | 100.0 |
| Eligible | 1042 | 34.4 | 481 | 15.9 | 2 | 0.1 | 1504 | 49.6 | 3029 | 100.0 |
| Enrolled | 52 | 12.6 | 118 | 28.6 | 0 | 0.0 | 243 | 58.8 | 413 | 100.0 |
| Total | ||||||||||
| RAF completed | 36,741 | 19.9 | 4846 | 2.6 | 1127 | 0.6 | 141,746 | 76.8 | 184,460 | 100.0 |
| Eligible | 13,059 | 14.3 | 1908 | 2.1 | 103 | 0.1 | 76,255 | 83.5 | 91,325 | 100.0 |
| Enrolled | 2249 | 11.4 | 450 | 2.3 | 5 | 0.0 | 17,043 | 86.3 | 19,747 | 100.0 |
RAF: risk assessment form; SCOPE: STAR Community Outreach Programs for Education; MBCCOP: Minority-Based Community Clinical Oncology Program; NMA: National Medical Association.
Discussion
Various planned and adapted minority recruitment efforts in the STAR trial increased minority accrual from 3.5% in the BCPT to 6.5% in STAR. The 38,910 RAFs submitted from minority women demonstrate the success of the outreach and recruitment program overall. The continued submission of RAFs from minority women, even after overall recruitment began to wane, shows that STAR investigators and sites successfully attracted the attention of minority women and recognized the importance of minority accrual (Table 2). An extended enrollment period would have increased enrollment among all minority groups because of the increased minority accrual as the trial progressed (Table 2). The large number of RAFs from non-SCOPE and non-MBCCOP sites (Table 4) emphasizes the need for improved education of providers about breast cancer risks, especially in communities where high-risk clinics are less common and where adequate and sustainable infrastructure for risk counseling and adherence are needed. Recruitment efforts from several new initiatives and minority-serving institutions contributed large numbers of RAFs but yielded lower accrual for multiple reasons including low risk scores.
Over the past several decades, NSABP adjuvant therapy trials in both breast and bowel cancer have included individuals, including racial minorities, who are at risk of recurrent disease. Between 2000 and 2009, the minority enrollment in NSABP treatment trials ranged from 13% to 18%. Cancer prevention trials present different challenges in order to assure that the trial population reflects the total at-risk population, in this case, women at increased risk for breast cancer in North America. It is unclear whether 6.5% is an adequate representation of the minority women who are at increased risk of breast cancer. Breast cancer incidence rates in postmenopausal minority women, particularly those in African-American women, are lower than those in white women. The NSABP used data from a study by Freedman et al. [13] to calculate target accrual numbers and to estimate the number of postmenopausal women who would be eligible for chemoprevention. Among 42 million white and 6 million black women aged 40–79 years, 2.4 million (5.8%) white and 32,000 (0.5%) black women would have been risk eligible and likely to benefit from tamoxifen based on the 1999 risk/benefit index. In addition to their breast cancer risks, potential participants were given risk/benefit estimates for entering the trial. The facts that tamoxifen increases the risk of blood clots, strokes, and endometrial cancers, and that minority populations have a higher rate of hypertension, diabetes, and obesity, may have influenced the decision of minority women who did not enter the trial [14,15].
Despite the low numbers of risk-eligible African-American women who attempted to enroll in STAR (only one in seven of these women received an ‘eligible’ response), research staff persevered and continued to recruit. Each of the 7749 (19.9%) risk-eligible minority women who chose to enter the study received an individualized assessment of her breast cancer risk, information about breast cancer, and the importance of breast cancer screening studies. Breast cancer risk assessment is a dynamic process, and one for which an immediate decision is not required to reduce potential risk. Future research should consider interventions to evaluate the contribution of cultural, socioeconomic, and behavioral factors that influence the choices made by minority women who are risk eligible for chemoprevention.
Compared with the Selenium and Vitamin E Cancer Prevention Trial (SELECT) (prostate cancer prevention trial), STAR had significant eligibility differences that influenced minority recruitment (e.g., age and risk factors) [16,17]. SELECT used study supplements with little-known toxicities at the time of recruitment; the drugs used in the STAR had known toxicities that often were perceived by minority women and providers to be more prevalent among minorities.
It is important to monitor minority accrual both nationally and at local centers and to adapt recruitment programs as needed. Success in terms of minority accrual of the individual programs in the STAR trial varied; no single program offered the sole solution to minority accrual. Overall, SCOPE sites had higher minority accrual than did non-SCOPE sites, but SCOPE sites were selected predominantly for their access to large minority populations. Importantly, the SCOPE sites were successful in engaging communities that had not previously participated in clinical research. It is noteworthy, however, that non-SCOPE, nonminority-based CCOP sites also had substantial minority accrual.
Collectively, corporate recruitment efforts did not result in large accrual numbers, but the concept holds substantial promise for enhancing minority enrollment in future trials, especially with the endorsement of cancer risk reduction by employers. However, the receipt of 9539 RAFs from a mailing of 133,000 represents a very successful return (7%) from direct mailing of a survey [18]. A lesson learned from this initiative is that a community informed of the importance of overall health may be more receptive to efforts to prevent cancer.
To our knowledge, the enrollment of 92 Native American women is the largest enrollment from this group to a cancer trial. Future enrollment of Native Americans will require considerable time and planning, particularly because of the increasing importance of biospecimens in cancer studies.
The differential risk eligibility between white and black women as calculated from the Gail Model was a significant barrier to enrollment in the STAR study. Grann et al. [19] has argued that until large cohorts of minorities are available to validate the Gail Model, race and ethnicity should not be a variable in the model. The CARE Model was developed in 2007 using data from 1600 African-American women in the Women’s Contraceptive and Reproductive Experiences Study to validate the Gail Model for predicting risk of breast cancer among African-American women [20]. Relative and absolute risks were calculated and then validated using the STAR eligibility criteria. The 5-year risk was higher with the CARE Model for 90.3% of women screened. If the current Gail Model, which has incorporated the CARE data, had been used, 30.3% of African-American women would have been risk eligible for the STAR trial, instead of 14.5%. Similar findings have been reported from large at-risk African-American populations [21].
Because the RAFs for STAR were the property of the participating sites, further data participant contact and data collection by NSABP would be difficult or impossible. In particular, data related to factors that may have been important in the decision-making process are not available. NSABP is now conducting a study that uses an anthropological approach to understanding the reasons that decisions are made for choosing chemoprevention for breast cancer risk reduction.
Future trials that incorporate biomarker evaluations and risk stratification must ensure that women from all racial/ethnic and socioeconomic groups are included. It is important to sustain the efforts of assessing breast cancer risk at sites such as the ones that participated in STAR, provide recognition and compensation for the increased time and labor involved in informing women of their risks, and support the entire recruitment process. Although our efforts were successful in more than doubling our minority accrual compared with accrual in the BCPT and in raising awareness of breast cancer risks, there remains room for improvement. The NSABP plans to continue these minority recruitment efforts and others in ongoing and future studies.
Acknowledgments
The authors thank Barbara C. Good, PhD, for editorial assistance. We also thank the members of the NSABP’s Diversity Strategic Planning Working Group for their advice and efforts in the planning and execution of the STAR trial.
Funding
This study was supported by Public Health Service grants U10-CA-37377, U10-CA-69974, U10-CA-12027, and U10-CA-69651 from the National Cancer Institute, National Institutes of Health, Department of Health and Human Services, AstraZeneca, and Eli Lilly.
Footnotes
Conflict of interest
The authors report no potential conflicts of interest.
References
- 1.Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: Report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371–1388. doi: 10.1093/jnci/90.18.1371. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer Facts & Figures for African Americans 2009–2010. Atlanta, GA: American Cancer Society; 2009. [accessed 13 October 2011]. Available at: http://www.cancer.org/acs/groups/content/@nho/documents/document/f861009final90809pdf.pdf. [Google Scholar]
- 3.Howlader N, Noone AM, Krapcho M, et al., editors. Bethesda, MD: National Cancer Institute; 2011. [accessed 17 October 2011]. SEER Cancer Statistics Review, 1975–2008. Available at: http://seer.cancer.gov/csr/1975_2008/ (based on November 2010 SEER data submission, posted to the SEER web site) [Google Scholar]
- 4.Ford JG, Howerton MW, Lai GY, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer. 2008;112:228–242. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- 5.Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: The NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727–2741. doi: 10.1001/jama.295.23.joc60074. (Erratum in: JAMA 2006; 296(24): 2926; JAMA 2007; 298: 973) [DOI] [PubMed] [Google Scholar]
- 6.Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879–1886. doi: 10.1093/jnci/81.24.1879. [DOI] [PubMed] [Google Scholar]
- 7.Gail MH, Costantino JP, Bryant J, et al. Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer. J Natl Cancer Inst. 1999;91:1829–1846. doi: 10.1093/jnci/91.21.1829. (Erratum in: J Natl Cancer Inst 2000; 92: 275) [DOI] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. Vital Statistics of the United States, 1992, vol. II, Mortality, Part A. Washington, DC: Public Health Service; 1996. (DHHS Publ No. (PHS) 96–1101, Tables 1–27) [Google Scholar]
- 9. [accessed 13 October 2011]; http://seer.gov/data.
- 10. [accessed 13 October 2011]; http://www.cancer.gov/bcrisktool/
- 11.McCaskill-Stevens W, Wilson J, Bryant J, et al. Contralateral breast cancer and thromboembolic events in Afri- can American women treated with tamoxifen. J Natl Cancer Inst. 2004;96:1762–1769. doi: 10.1093/jnci/djh321. [DOI] [PubMed] [Google Scholar]
- 12.Boesch M. National Indian Child Welfare Association’s Best Practices Magazine. Portland, OR: National Indian Child Welfare Association (NICWA); 2001. Jul, Nana’s Lesson. [Google Scholar]
- 13.Freedman AN, Graubard BI, Rao SR, et al. Estimates of the number of U.S. women who could benefit from tamoxifen for breast cancer chemoprevention. J Natl Cancer Inst. 2003;95:526–532. doi: 10.1093/jnci/95.7.526. [DOI] [PubMed] [Google Scholar]
- 14.Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30:736–743. doi: 10.1161/01.str.30.4.736. [DOI] [PubMed] [Google Scholar]
- 15.Kittner SJ, White LR, Losonezy KG, Wolf PA, Hebel JR. Black-white differences in stroke incidence in a national sample. The contribution of hypertension and diabetes mellitus. JAMA. 1990;264:1267–1270. [PubMed] [Google Scholar]
- 16.Lippman SM, Klein EA, Goodman PJ, et al. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: The Selenium and Vitamin E Cancer Prevention Trial (SELECT) JAMA. 2009;301:39–51. doi: 10.1001/jama.2008.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cook ED, Moody-Thomas S, Anderson KB, et al. Minority recruitment to the Selenium and Vitamin E Cancer Prevention Trial (SELECT) Clin Trials. 2005;2:436–442. doi: 10.1191/1740774505cn111oa. [DOI] [PubMed] [Google Scholar]
- 18.Spilker B, Cramer J. Patient Recruitment in Clinical Trials. New York: Raven Press; 1992. pp. 83–86. [Google Scholar]
- 19.Grann VR, Jacobson JS, Troxel AB, et al. Barriers to minority participation in breast carcinoma prevention trials. Cancer. 2005;104:374–379. doi: 10.1002/cncr.21164. [DOI] [PubMed] [Google Scholar]
- 20.Gail MH, Costantino JP, Pee D, et al. Projecting individualized absolute invasive breast cancer risk in African American women. J Natl Cancer Inst. 2007;99:1782–92. doi: 10.1093/jnci/djm223. (Erratum in: J Natl Cancer Inst 2008; 100(15): 1118; J Natl Cancer Inst 2008; 100(5): 373) [DOI] [PubMed] [Google Scholar]
- 21.Adams-Campbell LL, Makambi KH, Frederick WA, et al. Breast cancer risk assessment comparing Gail and CARE Models in African-American women. Breast J. 2009;15(Suppl. 1):S72–S75. doi: 10.1111/j.1524-4741.2009.00824.x. [DOI] [PMC free article] [PubMed] [Google Scholar]