Summary
Objectives
We evaluated the design of three novel visualization techniques for integrated health information with health care providers in older adult care. Through focus groups, we identified generalizable themes related to the visualization and interpretation of health information. Using these themes we address challenges with visualizing integrated health information and provide recommendations for designers.
Methods
We recruited ten health care providers to participate in three focus groups. We applied a qualitative descriptive approach to code and extract themes related to the visualization of graphical displays.
Results
We identified a set of four common themes across focus groups related to: 1) Trust in data for decision-making; 2) Perceived level of detail for visualization (subthemes: holistic, individual components); 3) Cognitive issues (subthemes: training and experience; cognitive overload; contrast); and 4) Application of visual displays. Furthermore, recommendations are provided as part of the iterative design process for the visualizations.
Conclusions
Data visualization of health information is an important component of care, impacting both the accuracy and speed of decision making. There are both functional and cognitive elements to consider during the development of appropriate visualizations that integrate different components of health.
Keywords: Aged, health services, consumer health information, data display
1. Introduction
Health data collected from multiple sources and over longer periods can be a challenge to present efficiently in order to convey the appropriate messages. In addition, there are many stakeholders interested in the data, including health care providers (HCPs), patients, and family members. With the advancement of technologies, pervasive computing applications enable data capture of various physical parameters and other variables of health monitoring. The question becomes, how can we appropriately present large and complex health related data sets in a meaningful manner? It is important to make a distinction between data and information; the former exists as a raw collection of values while the latter is that same collection organized and processed for knowledge.
Data visualization is a concept that generalizes across all disciplines. Visual displays can have a profound influence on decision-making, influencing not only how quickly one can interpret information, but also how the information is interpreted [1–4]. There exists a broad range of literature describing the importance of visual displays within the context of health care and decision-making. In one study, Hoeke et al. presented lab results in four different formats, asking laboratory technicians and physicians to assess abnormal results [5]. The authors found a significant relationship between the speed of decision-making and the method of visual display. Feldman-Stewart et al. examined the impact of visual displays on treatment decisions, both in terms of determining the direction and scale of a treatment effect [6, 7]. The authors found differences in accuracy and speed of processing across displays of pie charts, vertical bars, horizontal bars, numbers, systematic ovals and random ovals. They recommend the vertical bar chart with scales as an optimal visual display for older adult’s assessment of risk [7].
One goal of using visual displays is to reduce the cognitive load of information, allowing users to easily interpret and assess large amounts of data. Tufte has elegantly described how the brain functions similarly among individuals at deep core levels to process data and that these steps in brain function should guide visual displays of data [8]. Researchers have proposed different theories on cognitive processes involved in interpreting graphical information. These include theories on decomposition of graphical displays into elementary perceptual tasks [9], mapping of visual relationships [10], and processing of displays [11]. Though these theories provide a broad perspective on cognitive design principles of visual displays, to our knowledge, there has been limited work identifying the cognitive processes of data visualization involved within the context of health information used by HCPs for gerontological care.
In this qualitative descriptive study [12], we used focus groups to evaluate HCPs perceptions of three types of visual displays of integrated health information. These focus groups provided insights into the functional and cognitive elements important for designing visual displays for HCPs. The results of our study provide a set of common identified themes and design recommendations to guide further design iterations.
2. Background
2.1 Data Visualization for Gerontological Care
Health care providers involved in gerontological care have limited time and resources for evaluating health information. A 2003 report from the National Academy on an Aging Society identified a geriatric labor force that is unable to meet current demands, let alone respond to the predicted growth of the older adult population [13]. In addition, the adoption of electronic health records (EHR) has only increased the availability of information. There is recognition that, though EHRs have the potential to aggregate large amounts of data, many providers face the challenge of effectively visualizing the information [14, 15], given limited time availability. Work on data visualization for EHRs has focused on providing information at both high level overview and granular detail [16]. An additional challenge lies in the multi-modal nature of EHR data [17]. It is therefore critical to develop effective data visualization tools to support the work of gerontological HCPs.
In order to support older adults who want to maintain their independence, it is important to address their health care needs in a comprehensive manner. In a pilot study, we used commercially available health monitoring technologies to gather a wide range of health information at an older adult independent and assisted living facility [18]. We collected a wide range of data over an eight-week period. Both HCPs and older adults expressed interest in receiving the collected data; however, it was a challenging task to efficiently present the information, given the amount of the resulting raw data and the various information needs and expectations of stakeholders. We therefore chose to develop new visual displays in an attempt to overcome these challenges. We applied Dunn’s wellness model as a theoretical foundation for the aggregation of health monitoring data into the four categories of wellness: cognitive (i.e. specific tasks like planning), social (i.e. social support), physical (i.e. physiological measurements and activities of daily living) and spiritual (i.e. self-reported spiritual perspective) [19]. This model presents wellness at a high level while recognizing the interaction of components that contribute to wellness overall. Dunn’s model has been operationalized and validated within health research [20–22].
2.2 Design of Visual Displays
We created three novel types of visual displays of wellness using integrated data from a technology assessment pilot study with older adults [18, 23]. The visual display types were developed using principles derived from cognitive theories concerning how people map visual relationships using spatial location, magnitude, and groupings [10], and how they identify positions along common and non-aligned scales, length and angle, area, volume, and shading [9]. Existing work on data visualization within the clinical context focuses on integration within the laboratory setting or intensive care units with displays of specific physiological measurements [24, 25]. To our knowledge, there has been limited work on visualizations of holistic wellness to support gerontological care. Our visual display types represent wellness in the four different parameters described by Dunn (Figure 1). We calculated an aggregate score for each category and normalized using t-scores on a scale from 0 to 100, with a score of 50 being average relative to the general older adult population. For each of the three visual display types, two different example graphs were generated using different data sets. One graph presents two data points from the baseline and exit of the eight-week period pilot study [18, 23], while the other graph presents a longitudinal view of simulated data for a twelvemonth period.
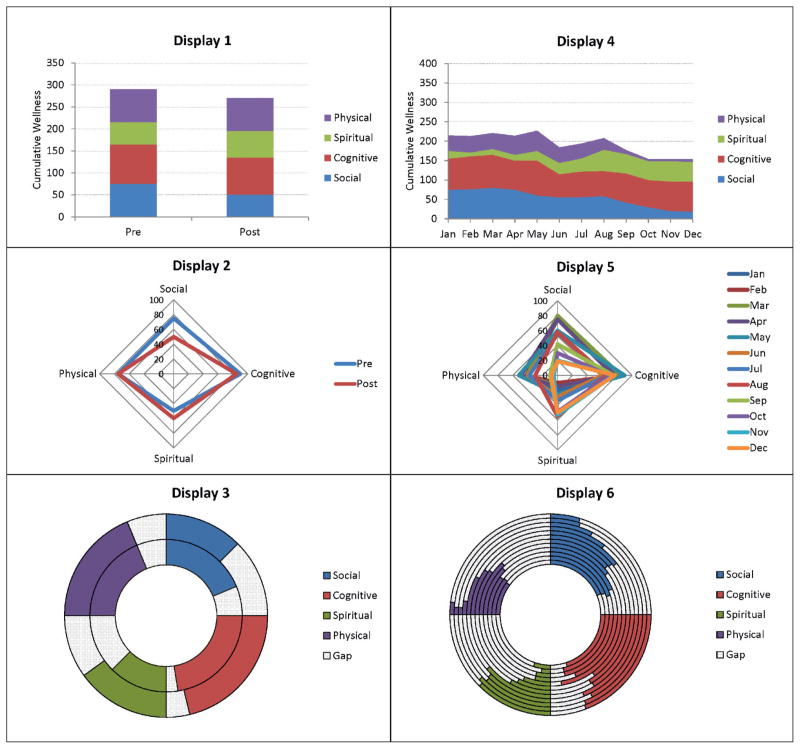
Figure 1.
Three sets of visual displays for comparisons between baseline and exit data, along with comparison of longitudinal data. The visualizations represent the same dataset for evaluation within focus groups.
We based the first set of displays on traditional bar graphs, however stacked with each of the four categories of wellness (Display 1 and 4). We presented the stacked bar charts with the goal of reducing cognitive load through a comparison of measures along vertical scales while also providing a familiar format of visual display. The second set of visual displays was a “Wellness polygon” (Display 2 and 5). Each vertex of the polygon was along one of four axes, representing the wellness categories. The vertices were connected to form a quadrilateral, with the goal of providing an overall area-based representation of wellness. Changing shapes potentially provide quicker assessment of wellness while skewness allows providers to assess specific areas of decline. We also created a donut display of visual health information (Display 3 and 6). We segregated wellness categories into quadrants within a circular ring, with a fully filled quadrant representing full score. Rings expand outward to represent newer data. We developed this display as an alternative with a focus on changing subcomponents within an overall wellness score. A further elaboration on the cognitive design principles involved within these visualizations can be found in prior work by Le et al. [26].
Since visual displays can affect how HCPs make decisions [5, 27] it is important to assess how HCPs perceive novel visualizations of complex constructs such as wellness. Therefore, the aim of this study was to assess the visualization of data rather than the specific content of data examples. The baseline/exit visualizations all represented the same dataset. This was also true of the longitudinal visual displays. Since the designs are early prototypes, we chose to evaluate the visualizations only to HCPs. Other stakeholders are part of our future work after design reiterations.
3. Methods
3.1 Participants and Setting
We recruited subjects through gerontological/geriatric health care provider e-mail lists of professionals practicing in a larger metropolitan area in the Pacific Northwest. A member of our research team invited interested participants to contact the researchers to learn more about a focus group study examining visualization of wellness data for older adults. Inclusion criteria were training and experience as a health care provider, experience working with older adults, and willingness to participate in the study. Exclusion criteria included unwillingness to be audio-recorded. All participants provided informed consent prior to study enrollment. The Institutional Review Board (IRB) of the University of Washington approved all procedures.
3.2 Data Collection
We conducted focus groups [28] to explore how HCPs who work with older adults in community settings perceive novel visualizations of wellness. We developed the focus group guide with the aim of exploring the way HCPs perceive novel visual displays. The guide was constructed using wellness data from the older adult pilot technology study [18, 23] and cognitive theory as guiding principles [9, 10]. The cognitive theories guided our original development of the visual displays; they provided further focus for our focus group scripts. It included questions about how HCPs perceive and use visual displays of integrated health monitoring information, for example whether an individual is drawn to higher level analysis of a display or more granular components. In addition, we asked participants to describe the cognitive processes involved in analyzing a visual display. The guide was pilot tested with members of our research group that includes clinicians and was modified twice before engaging the study participants.
We conducted focus groups during the period of September–October 2011. Focus groups were moderated by a team of two researchers who alternated in the roles of moderator and assistant moderator [28]. Both researchers were experienced with qualitative research and facilitation of focus groups. After participants provided informed consent, the moderator presented an overview of the study. This included an introduction to Dunn’s wellness model as context for presentation of the visual displays. The moderator led the focus group, presenting visual displays with a projector and using the focus group guide to direct the discussion, while the assistant moderator took notes for follow-up questions. The moderator presented to participants each visual and asked about their perceptions, specifically what elements of the display helped enhance or detract from the visualization of information. Participants also compared visual displays. Each focus group session was recorded using a digital audio-recorder and later transcribed verbatim for data analysis.
3.3 Data Analysis
Two researchers analyzed focus group transcripts with the goal of answering the following questions: 1) how do HCPs process and interpret visual health information, and 2) how do HCPs apply visual data to support older adult care? Analysis focused on the “what” of participant perceptions versus the “how” of participant interactions [29]. Development of codes was an evolutionary process, using inductive and thematic analysis [30, 31] to systematically read, analyze, and derive content from the focus group transcripts [32].
After each researcher independently read the transcripts and developed a preliminary codebook, two researchers checked the codebook for content validity. All transcripts were independently double-coded by both researchers and codes were further refined. Mismatches were discussed until both researchers came to a full agreement. We used the codes to describe emergent themes. Each focus group provided differing insights into themes and concepts, which we then compared to existing definitions. By refining our codes with successive iterations of coding sessions, we continuously renamed, reorganized and redefined themes [30]. We compared coded results within and between focus groups to synthesize agreement and disagreement of participant perceptions.
4. Results
Ten participants participated in the focus group sessions (1 male, 9 female). Each session lasted between 60–75 minutes. The first session included two participants, the second five and the third three participants. Though participants ranged in level of experience, all were licensed care providers within a gerontology setting.
4.1 Concepts and Themes
The results of our qualitative analysis identified a set of common themes associated with visualization of integrated health information (Table 1). These themes are generalizable across the different visual displays and emerged from the discussions within the focus groups. We identified four major themes related to participant perceptions of displays. These themes are: 1) Trust in data for decision-making; 2) Perceived level of detail for visualization (sub-themes: holistic, individual components); 3) Cognitive issues (subthemes: training and experience; cognitive overload; contrast); and 4) Application of visual displays.
Table 1.
Summary of primary themes identified from qualitative descriptive analysis of focus groups
| Theme | Definition | Example |
|---|---|---|
| 1. Trust in data for decision making | This theme includes issues associated with the source of data for visual displays and what types of health information would be useful when visualized. | “Oh interesting, would have thought it would have been longer and or be closer in gap because at eight weeks it seems as though now people think they don’t feel as well then, interesting, eight weeks hmm.” |
| 2A. Visualization of health – perceived as focused view (individual components) | This theme deals with visual displays that are perceived primarily as displaying individual components of wellness through different features of the visual display. | “I really appreciate that it’s a square and I feel like the different angles tell me something too. “ |
| 2B. Visualization of health – perceived as summary view (holistic) | This theme deals with visual displays that are perceived primarily as displaying summary views of wellness. | “I feel like I can glance at it and we can, tell there is more area inside the blue polygon then the red…” |
| 3A. Cognitive issues – Cognitive overload | Theme associated with an overload of information from the visual displays resulting in difficulty interpreting the information. | “I can see this being pretty confusing for a family member though. If I’m trying to show them that they are going to be, whoa, what is that?” |
| 3B. Cognitive issues – Contrast issues | Use of visual displays to impact cognitive load for comparisons of health information within display. | “I think it’s subtle but you can tell what the differences are but they’re not, it’s not drastic enough to make a point.” |
| 3C. Cognitive issues – Training and experience | Theme focused on the learning curve involved with interpreting and using visual displays and how this might negatively impact uptake of visual displays. | “… the reason I think it looks confusing and overwhelming at first is because I have never seen it represented in that way before.” |
| 4A. Use of visual displays – Decision making | Theme related to how visual displays can impact the decision making process amongst health care providers, older adults, and family and friends. This theme also includes shared-decision-making. | “And if you know one aspect of wellness has diminished if something else has compensated for that, I think that would be maybe acceptable to somebody, some family member, the actual individual themselves.” |
| 4B. Use of visual displays – Identifying health deficits | This theme deals with how visualizations might support detection of health deficits, or sudden changes and decline in health. | “I feel like I would know that the deficits based on this graph for the pre and the post data say that they needed more assistance with their spiritual needs…” |
| 4C. Use of visual displays – Intervention | Theme related to how visual displays could be used by a health care provider or family member to become involved in older adult care. | “And it’s also a way to figure out your resource allocation. Do you send an MD, a nurse practitioner, or do you send the therapies out?” |
| 4D. Use of visual displays – Monitoring long term trends | Use of visual displays as a tool to detect longitudinal trends in health. | “So if, that’s what I would look at this image, and say I am concerned about your cognitive needs. Why is it declining, right?” |
4.1.1 Trust in Data for Decision-making
Issues associated with trust in displayed data influenced how participants interpreted visual information. Participants raised concerns about data origins, validity, and appropriateness of Dunn’s model of wellness. Discussions of trust issues were sporadic and types of issues raised were not uniform across focus groups. However, these issues created pause for HCPs in assessing the utility of the displays.
4.1.2 Perceived Level of Detail for Visualization
HCPs interpreted visual displays with a focus on both holistic wellness and individual components of wellness. Participants described holistic views of visual displays often as a cursory glance to acquire broad levels of information. However, there was also a challenge in balancing this with providing component levels of health information, as highlighted by a participant: “When I look at this I am able to see general wellness, like the change from pre to post, but it’s harder for me to look at the difference between each individual piece because they’re stacked together.” Participants who focused on components of a visual display were concerned with how different wellness categories interacted with each other to contribute to overall health. An individual’s level of perception for a visual display can vary depending on which particular display is chosen, and how the individual intends to use the data. As one participant noted, this can interact together in a complementary manner:
“That is one thing I really like about having them all together, is it’s not, it doesn’t fragment out the parts of health because I really think you can’t forget how important that side of it is, so I think that it’s very effective in showing that when your social goes down, your overall health goes down because it all hooks up.”
4.1.3 Cognitive Issues
We identified cognitive processing issues under three subthemes that affected ease of interpreting visual displays. These sub-themes were training and experience, cognitive overload, and contrast of elements.
Training and experience played a role in how participants interpreted displays. Participants made comments about confusion related to first time viewing of novel displays and the need for context and labels with first time viewing but not with subsequent views. For the longitudinal donut visualization (Display 6), there was general agreement that there was a tendency to “read” the display from left to right as opposed to an inner to outer ring of data. Participants also highlighted the need for training to interpret visual displays to increase adoption and usefulness.
“I feel like if you were going to use the polygon, maybe [providers] that are older and are not as familiar with technology, not as familiar with the graph would require more guidance and may not be able to interpret and may not find it useful and may not use it at all.”
Cognitive overload was often associated with responses of confusion and uncertainty, especially when participants had multiple visual cues to focus on in the visual displays (Table 1). Participants expressed this sense of cognitive overload primarily in the longitudinal Wellness polygon visualization (Display 5). Too many overlaid polygons contributed to challenges in assessing depth of polygons and interpreting overall wellness.
Contrast of elements was an issue when participants were unable to easily distinguish elements within displays, such as the heights of bars and colors of lines, from each other. This was most prevalent for the stacked bar plot (Display 1) with contrast issues stemming from the stacking of individual components and subtle differences between them. The longitudinal extension of the stacked bar chart (Display 2) also had contrast issues related to comparisons of components within the display. For Display 3, some participants pointed out the dissonance in area comparisons in the donut plot. As rings expand outwards, the overall area increases even if score stays the same based on an angular comparison. This can misconstrue interpretations.
4.1.4 Application of Visual Displays
We found that visual displays differed in how the information was interpreted for use. Use of visual information for intervention refers to instances when a participant describes how the visual information could directly impact care of older adults. In particular, this theme arose when the focus group members discussed involving the older adult or a family member directly within older adult care in response to a sudden change in visual display of wellness. As one participant described:
“…that’s what I would look at this image, and say well, I am concerned about your cognitive needs. Why is it declining, right? So I want to know, before it was better and now it’s worse. So what is changed?”
The use of visual information display for intervention ties closely with detection of longitudinal trends. Health care providers noted the importance of identifying longitudinal trends in health from the visual displays. For example, participants noted sudden drops in overall health with concern and further described the processes involved in analyzing the visual displays to identify sources of the decline. The visual displays also provide a resource to initiate conversation with older adults. This was categorized under use of visual displays for decision making where both HCPs and older adults benefit from the shared information of the visual displays. For example, one participant described how the visualizations could facilitate planning of events for older adults within a community center. Another participant described the information as:
“… sort of a jumping off point and then you as the clinician still have to figure out what is actually going on, but I guess this data for me would give me a place to start, but it’s really going to be, the patient’s going to determine where I go next.”
Though the focus groups were from the perspective of HCPs, an additional application of visual displays relates to its ability to support older adult self-efficacy. Respondents had mixed perspectives on this issue; with some participants highlighting the ability of visualization data to encourage pro-active monitoring of health for older adults. However, others cited negative impacts of visual display on self-efficacy. In particular, if health were declining, some felt that displaying such results might only cause further discouragement. As one participant stated, “I think you rise to the level of expectations”.
4.2 Design Preferences and Recommendations
Participants provided valuable insight towards the design of visual displays. Researchers can use concrete recommendations and constructive feedback from users as part of an iterative design process to further refine visual displays.
4.2.1 General Recommendations
Participants were in favor of the conceptual framework for wellness, citing the need for cognitive, social, physical, and spiritual measures. There was disagreement on the extent to which each visual display should emphasize components of wellness; however, a common recommendation across focus groups was the further separation of visual displays to better compare individual components. A general recommendation made by most participants emphasized the need for simplicity of visual displays while providing for the ability to access more data:
“just tell them what they need to know, don’t fluff it up and so we used to have something beautiful and big for those who like to sit down and read… overall people like to hear the information so that they can process it and then formulate their questions and then come and ask you if they needed more information”.
4.2.2 Recommendations for Stacked Bar Charts (Displays 1 and 4)
A primary criticism of the stacked bar plots is the inability to distinguish between gradient changes within components, prompting one participant to state:
“I think that it’s great for an overview but, cumulative wellness is less… I wonder if there’s a way to just lay it where it’s more clear that really the other three of the process haven’t changed much and really just one of them is the one that has sort of diminished.”
Participants also describe a need to separate visualizations into individual categories to more easily identify deficits and apply interventions. One possible modification involves incorporating the suggestions to separate each stack within the bar plot into separate graphs. An alternative is to allow an interactive visual display where the bars are still stacked; however, upon selecting a component of wellness, the stacks will re-align relative to the given component.
4.2.3 Recommendations for Polygon Plots (Displays 2 and 5)
For the polygonal representation of data (Displays 2 and 5), a general criticism lay in its complexity. Participants cited the overwhelming nature of the information and instead preferred to pass towards alternative visualizations. Others cited the difficulty of understanding how to interpret the information, yet also noted that upon explanation, the display provided a level of additional appeal compared to other displays.
“And then once you described it, I like it a lot. Cause I feel like I can kind of just glance at it and we can, I don’t know, just [kind of] tell there is more area inside the blue polygon then the red, so there’s been a change but physical and cognitive, there’s not much of a change and so I think it’s a really interesting way to look at it. Once you explained and it took me you know a couple seconds to kind of get used to what it was saying, I like it.”
The novelty of the display makes it difficult for some participants to grasp intuitively. However, upon explication, some participants noted that this visualization provides both cumulative information through the area of the polygon and component wise information through the length of each axis. When the polygons were stacked on top of each other to display longitudinal changes in wellness, participants unanimously found the display confusing. Problems cited included too much information, a cluttering of visual displays, and an inability to distinguish between depth and color of the polygons. Two participants agreed about the need for data displayed by seasons. The participants suggested simplifying the display into four polygons, representing different seasons. However, even upon reducing the number of polygons, the visual display was challenging to interpret. In this respect, the polygonal display was ineffective at presenting longitudinal information.
4.2.4 Recommendations for Donut Plots (Displays 3 and 6)
The donut plot (Displays 3, 6) generated the most variability in opinions. A common question asked by participants involved the labeling of the rings within the donut. Many were unsure which ring represented the oldest or newest data and suggested explicitly labeling it to prevent confusion. Some participants read the data from inside out, where the oldest data were at the center ring while the newest data were on the outer ring. Others interpreted this graph similar to the rings of a tree where older data are on the outer layer and newer data on the inner layer. The simplicity of the display appealed to some participants; however, others noticed the opposite:
“Well the first thing I did is I looked at the size of the graph and I said, okay well I can see where the changes were and there it was, and then I wondered after I looked at that if they were equal, if they were concentric circles or if they were different, if there was a size. And then I thought, boy that’s a lot of work for such simple data.”
Visually the rings can provide an intuitive comparison based on angular alignment of concentric circles, however there exists cognitive dissonance upon comparisons of area from one ring to the next. Despite scores for a component of wellness being similar, since the outer rings are larger in radius, the area of the component scores differ. One suggestion made by participants was to disregard the angular elements of the donut plot and instead generate bar plots grouped by each component of wellness. In other words, cut the donut plot into its four components, and re-align as bar plots rather than using an angular comparison.
4.2.5 Limitations
Our data set consists of three focus groups with ten participants. A common recommendation for focus group size is a range of 4–10 participants [28]. However, Morgan observes the difficulty of defining a “focus group” beyond that of a group interview and questions who should determine the size of a focus group [29, 33]. Krueger and Casey note that focus group sample size and type must fit the goals of research [28]. For our purposes, efficiencies in interviewing HCPs about visual designs were a driving factor of this study. Accordingly, smaller group interviews fit the goals of this study. Our focus groups ranged in size from 2–5 participants; however, we had targeted group sizes of 5–8 persons. Unfortunately, due to challenges with schedules of health care providers (e.g., unexpected clinic calls, clinic hours run over time, etc.) the ultimate sizes of the groups were smaller since we chose to run focus groups as scheduled with as many available participants at that time. We found that the quality of the data and richness of the discussions did not vary across groups. In addition, we drew our participants from one geographic area of the country. Although we sought representation from disciplines with a gerontological focus, other than medicine and nursing, we did not recruit pharmacist or allied health (physical/occupational therapy) providers into the study. Other HCPs may have differing needs and perspectives of health care information and we should make increased efforts to ensure their inclusion in future studies.
5. Discussion
We sought to provide designers with some initial answers to two questions: 1) how do HCPs process and interpret visual health information and 2) how do HCPs apply visual data to support older adult care? From the data derived within our focus groups, we find that there are two possible interpretations of wellness data; a focus on the holistic overview of wellness and a focus on individual components of wellness. Though a health care provider may find an overall measure of wellness interesting, they place a more significant focus on individual comparisons of wellness. This focus is driven by the needs and motivations of the health care provider:
“I think one of the challenges with that, it’s kind of like, when… I teach about functional assessment and one of the challenges with functional assessment tools that measures functional assessment is that they can give you an overall number but really, as a provider, in terms of it having meaning, you really have to look at the pieces and try to figure out why.”
Our findings indicate that visual focus is closely tied to issues of use and that there exists a distinction when a health care provider uses visual displays internally for clinical decision making compared to when it is shared with older adults. Health care providers expressed a preference for visualization of data as individual components of wellness, allowing for greater information and context to the visual display. It provides an anchor for HCPs to further identify and assess deficits in wellness. That is not to say HCPs ignore holistic views of data; only that they use it for a cursory overview. The true value of visualization efforts for HCPs lies in its ability to narrow down potential causes of changes in health; visual displays provide this through a focus on component level views of data.
However, HCPs shift their focus of visual displays when interacting with older adults, they placed a greater emphasis on holistic views of data. This provides a broader perspective, which HCPs can use to start discussions with older adults and can narrow down if necessary:
“I think it might be more relevant for them [older adults], maybe more concerned about just the overall wellness.”
We attribute a part of this shift in emphasis to the complexity and challenges of explaining visual displays. Participants also described the use of information as a jumping off point for discussions. Health care providers find it fruitful to engage older adults in identifying causes of changes in wellness, and from there, they gather the detailed information that may indirectly be tied to component levels of health data. Health care providers can use the visual displays for holistic views of wellness to facilitate a broad, open discussion for shared decision making with older adults.
6. Conclusion
We applied cognitive design principles to develop three different visual displays of integrated health based on data collected from an eight-week pilot study at an older adult independent and assisted living facility [18, 23]. We evaluated these visual displays with HCPs for three focus groups of size ranging between two and five participants. The purpose of the focus groups was to provide an evaluation of the visual displays and to better understand the processes involved by HCPs during the visualization process. Through a qualitative descriptive analysis of focus group data, we found that HCPs are inquisitive about the source of data for a given visual display. To make displays effective, it is important that HCPs understand where the data is coming from and are comfortable with its integration into the visualization. Without this trust in the data source, HCPs are reluctant to place credence towards a visualization and often find it has limited application. Especially for novel visual displays, not only training but also gaining provider buy-in through piloting and validation are critical prior to implementation. The cognitive challenges associated with our visual displays highlight a need for clarity (labeling, color, granularity and contrast) and reduction of complexity (cognitive overload). This is consistent with many design principles that emphasize a minimalist approach towards data visualization [2]. We can generalize our results for the design of future visual displays of health information using these set of guidelines derived from the focus groups.
The focus groups also provided valuable inputs towards the evaluation of our visual displays. These evaluations allow us to refine our visual designs as part of an iterative process of design. Health care providers found value in both a holistic and component based view of data in the visualizations, but for different reasons. A holistic view allows for quick cursory glances and provides ability to engage older adults with discussions of the health information while a component view allows identifications of trends in overall health and ability to see where further focused assessment is needed.
In addressing the needs of HCPs, designers should consider minimalized visual displays for broad level views of information while still allowing for the display of granular categorized areas of information (e.g., through an interactive visualization). An effective design that synthesizes data will allow clinicians to more easily interpret information, independent of skill level or prior knowledge. For our work, the visualizations are early prototypes and from the feedback received, can be improved by addressing both functional and cognitive issues within the display. We intend to further evaluate the visual designs with older adults as stakeholders of the health information. The information needs of older adults may not align with those of HCPs; as a result, an evaluation with older adults can provide novel insights. Our work can eventually be integrated with existing systems as a tool to share and display health information. This provides a resource for informed decision-making amongst older adults, HCPs, and family members. An understanding of visualization needs can help with the integration of visualizations as an active tool within electronic health records to accommodate for vast and longitudinal patient data [34].
Acknowledgments
This work was supported by the National Library of Medicine (NLM) Training Grant T15LM007442 and by the National Institute of Nursing Research (NINR) Training Grant T32NR007106. We would like to additionally thank all study participants for their valuable contributions.
References
- 1.Bertin J. Graphics and graphic information-processing. de Gruyter; 1981. [Google Scholar]
- 2.Tufte ER. The visual display of quantitative information. Graphics Press; 1983. [Google Scholar]
- 3.Lurie NH, Mason C. Visual Representation: Implications for Decision Making. SSRN eLibrary. (Internet, cited Aug 3, 2012). Available from: http://papers.ssrn.com/sol3/papers.cfm?abstract_id=987295.
- 4.Speier C. The influence of information presentation formats on complex task decision-making performance. International Journal of Human-Computer Studies. 2006;64 (11):1115–1131. [Google Scholar]
- 5.Hoeke JO, Bonke B, Van Strik R, Gelsema ES. Evaluation of techniques for the presentation of laboratory data: support of pattern recognition. Methods Inf Med. 2000;39 (1):88–92. [PubMed] [Google Scholar]
- 6.Feldman-Stewart D, KocReferencesovski N, McConnell BA, Brundage MD, Mackillop WJ. Perception of quantitative information for treatment decisions. Med Decis Making. 2000;20 (2):228–238. doi: 10.1177/0272989X0002000208. [DOI] [PubMed] [Google Scholar]
- 7.Feldman-Stewart D, Brundage MD, Zotov V. Further insight into the perception of quantitative information: judgments of gist in treatment decisions. Med Decis Making. 2007;27 (1):34–43. doi: 10.1177/0272989X06297101. [DOI] [PubMed] [Google Scholar]
- 8.Zachry M, Thralls C. An Interview with Edward R. Tufte Technical Communication Quarterly. 2004;13 (4):447–462. [Google Scholar]
- 9.Cleveland WS, McGill R. Graphical Perception and Graphical Methods for Analyzing Scientific Data. Science. 1985;229 (4716):828–833. doi: 10.1126/science.229.4716.828. [DOI] [PubMed] [Google Scholar]
- 10.Pinker Steven. Artificial intelligence and the future of testing. Erlbaum; 1990. A Theory of Graph Comprehension. [Google Scholar]
- 11.Carpenter PA, Shah P. A model of the perceptual and conceptual processes in graph comprehension. Journal of Experimental Psychology: Applied. 1998;4 (2):75–100. [Google Scholar]
- 12.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23 (4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 13.Hudson R. Emerging Crisis: The Geriatric Care Workforce. National Academy on an Aging Society. 2003;13(2) [Google Scholar]
- 14.Boyd AD, Funk EA, Schwartz SM, Kaplan B, Keenan GM. Top EHR challenges in light of the stimulus. Enabling effective interdisciplinary, intradisciplinary and cross-setting communication. J Healthc Inf Manag. 2010;24 (1):18–24. [PubMed] [Google Scholar]
- 15.Tsiknakis M, Katehakis D, Orphanoudakis S. A health information infrastructure enabling secure access to the life-long multimedia electronic health record. International Congress Series. 2004;1268:289–294. [Google Scholar]
- 16.An J, Wu Z, Chen H, Lu X, Duan H. Level of detail navigation and visualization of electronic health records. 3rd International Conference on Biomedical Engineering and Informatics (BMEI); 2010. pp. 2516–2519. [Google Scholar]
- 17.An J, Lu X, Duan H. Integrated Visualization of Multi-Modal Electronic Health Record Data. The 2nd International Conference on Bioinformatics and Biomedical Engineering, 2008. ICBBE; 2008. pp. 640–643. [Google Scholar]
- 18.Thompson HJ, Demiris G, Rue T, Shatil E, Wilamowska K, Zaslavsky O, et al. A Holistic Approach to Assess Older Adults’ Wellness Using e-Health Technologies. Telemedicine and e-Health. 2011;17 (10):794–800. doi: 10.1089/tmj.2011.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dunn HL. High-Level Wellness for Man and Society. Am J Public Health Nations Health. 1959;49 (6):786–792. doi: 10.2105/ajph.49.6.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adams TB, Bezner JR, Drabbs ME, Zambarano RJ, Steinhardt MA. Conceptualization and measurement of the spiritual and psychological dimensions of wellness in a college population. J Am Coll Health. 2000;48 (4):165–173. doi: 10.1080/07448480009595692. [DOI] [PubMed] [Google Scholar]
- 21.Becker CM, Glascoff MA, Mitchell T, Durham TW, Arnold W. Assessing Perceived Health and Associated Health Promoting Behaviors: An Investigation of Methods Used to Assess Health Status. Journal of Applied Social Psychology. 2007;37 (2):227–242. [Google Scholar]
- 22.Bruhn JG, Cordova FD, Williams JA, Fuentes RG. The wellness process. Journal of Community Health. 1977;2 (3):209–221. doi: 10.1007/BF01349705. [DOI] [PubMed] [Google Scholar]
- 23.Demiris G, Thompson HJ, Reeder B, Wilamowska K, Zaslavsky O. Using informatics to capture older adults’ wellness. Int J Med Inform (Internet) 2011 Apr 7; doi: 10.1016/j.ijmedinf.2011.03.004. (cited May 17, 2011). Available from: http://www.ncbi.nlm.nih.gov/pubmed/21482182. [DOI] [PMC free article] [PubMed]
- 24.Goldschmidt AJ, Luz CJ, Giere W, Lüdecke R, Jonas D. Multi-dimensional visualisation of laboratory findings and functional test results for analysing the clinical course of disease in medicine. Methods Inf Med. 1995;34 (3):302–308. [PubMed] [Google Scholar]
- 25.Horn W, Popow C, Unterasinger L. Support for fast comprehension of ICU data: visualization using metaphor graphics. Methods Inf Med. 2001;40 (5):421–424. [PubMed] [Google Scholar]
- 26.Le T, Wilamowska K, Demiris G, Thompson H. Integrated data visualisation: an approach to capture older adults’ wellness. Int J Electron Healthc. 2012;7 (2):89–104. doi: 10.1504/IJEH.2012.049872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elting LS, Martin CG, Cantor SB, Rubenstein EB. Influence of data display formats on physician investigators’ decisions to stop clinical trials: prospective trial with repeated measures. BMJ. 1999;318 (7197):1527–1531. doi: 10.1136/bmj.318.7197.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. 3. Sage Publications, Inc; 2000. [Google Scholar]
- 29.Morgan DL. Reconsidering the Role of Interaction in Analyzing and Reporting Focus Groups. Qual Health Res. 2010;20 (5):718–722. doi: 10.1177/1049732310364627. [DOI] [PubMed] [Google Scholar]
- 30.Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 31.Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. Thousand Oaks: Sage Publications; 1994. [Google Scholar]
- 32.Krippendorff K. Content analysis: an introduction to its methodology. Sage; 2004. [Google Scholar]
- 33.Morgan DL. Focus Groups As Qualitative Research. SAGE; 1997. [Google Scholar]
- 34.Klimov D, Shahar Y, Taieb-Maimon M. Intelligent interactive visual exploration of temporal associations among multiple time-oriented patient records. Methods Inf Med. 2009;48 (3):254–262. doi: 10.3414/ME9227. [DOI] [PubMed] [Google Scholar]