Summary
Association of dysregulated calcium homeostasis and granulomatous disease is well established. There exist reports in the literature of granulomatous reactions produced by silicones associated with hypercalcemia. In this case series we report four young women that underwent methacrylate injections in gluteus, thighs and calves that developed granulomas with posterior appearance of hypercalcemia. This complication presented as subacute around 6 months after the procedure. The four patients have as common elements the presence of moderate to severe renal insufficiency, suppressed PTH and elevated calcitriol levels for the degree of renal function. In the image studies, two patients presented in the nuclear magnetic resonance of the gluteus hypodense nodular images compatible with granulomas. Two patients had a positron emission tomography performed showing increased metabolic activity in the muscles of the gluteal region compatible with granulomas. Two patients had a partial surgical resection of the gluteal lesions with the finding of methacrylate associated to foreign body granulomas. In these patients hypercalcemia was treated with oral or local injections of corticoids, intravenous bisphosphonates or ketoconazole with good response. Although the prevalence of this complication with methacrylate injection is not common, hypercalcemia secondary to granulomas should be considered in the differential diagnosis of patients with hypercalcemia when there is a history of this procedure, and especially if they have a reduction in their renal function.
Keywords: hypercalcemia, methacrylate, granulomatous disease
Introduction
The association of dysregulated calcium homeostasis and granulomatous disease was established in 1939 by Harrell et Fisher (1). With the advent of automated serum calcium determinations, the presence of mild to severe hypercalcemia had been detected in up to 10% of the patients with sarcoidosis (2). Hypercalcemia has also been detected in other granulomatous diseases as tuberculosis (3), leprosy (4) beriliosis and disseminated candidiasis (5).
In physiological conditions, the calcium serum concentration is regulated mainly by parathyroid hormone (PTH) and 1,25-(OH)2 vitamin D through interactions with the kidney, bone and gut. In granulomatous disease hypercalcemia is produced because of the presence of 1α-hydroxylase enzyme in macrophages (6) and giant cells that form part of the granuloma. In the granuloma the 25 (OH) vitamin D is converted to 1,25-(OH)2 vitamin D without any type of homeostatic control. The increase in 1,25-(OH)2 vitamin D causes hypercalcemia with PTH suppression. Thus, the presence of hypercalcemia with suppressed PTH and inappropriately elevated 1,25-(OH)2 vitamin D suggests the diagnosis of granulomatous disease.
In this case report series we describe the history of four females with severe hypercalcemia secondary to granuloma formation in the gluteus after methacrylate injection for esthetic reasons.
Case 1
Fifty three year old female who had a history of mammary prosthesis insertion in year 2006 without complications. In August 2009, having a normal serum creatinine (1 mg/dl), she underwent esthetic surgery of the gluteus with methacrylate injection. She became asthenic and in December 2009 she was found hypercalcemia (13.8 mg/dl) associated with decreased renal function and proteinuria for which she had a renal biopsy performed. She was treated with pulse steroids and oral methylprednisone as maintenance therapy. Serum creatinine decreased to 1.4 mg/dl and proteinuria became negative.
In March 2011, because of worsening renal function she had a second renal biopsy performed. She was diagnosed as having pauci-immune diffuse glomerulonephritis with crescents. She received 3 pulses of cyclofosfamide and steroids. Hypercalcemia was persistent: 11.3 (08/04/11), 12.4 (01/08/11) and 15.2 mg/dl (21/11/11), with very low iPTH (3.5 pg/ml), and 1,25-(OH)2D of 55.5 pg/ml, with normal serum phosphate and magnesium. Thinking in the presence of a granulomatous disease, we tried to remove the material from the gluteus, but it was difficult to do it completely as it was fragmented and encapsulated. The analysis of the surgically extracted material showed on top of the presence of methacrylate, silicon material associated with a foreign body granulomatous reaction.
In 2012 she is admitted to the hospital for persistent hypercalcemia and CRF. Hypercalcemia was treated with hydration, diuretics and calcitonin. She had a third renal biopsy performed (16/01/12) that was informed as moderate chronic tubule interstitial nephritis with mild mesangial glomerulonephritis. She was given corticosteroids in decreasing doses, blockage of the renin angiotensin system and treatment of her hypercalcemia with calcitonin and steroids.
Due to her persistent hypercalcemia associated with severe pruritus she was given ketoconazol 200 mg every 8 hours. With this treatment serum calcium normalized and pruritus disappeared.
Case 2
Twenty nine year old female who had mammary prosthesis insertion in year 2001. In July 2006 she had a renal biopsy performed with the diagnosis tubulo-interstitial nephritis that was attributed to auto medication with anti-inflammatory agents and diuretics. After treatment she remained with chronic renal failure stage III.
In March 2011 she had a serum creatinine of 1.9 mg/dl and in April she had esthetic surgery with transference of abdominal fat to the gluteus, thighs and buttocks associated with injection of methacrylate. In the analysis previous to that procedure her serum calcium was normal.
In November 2011 she was hospitalized for cholecistitis. Cholecystectomy was performed associated with severe deterioration of her renal function. She developed hypercalcemia without evidence of hyperparathyroidism. She was treated with intravenous pamidronate with improvement of serum calcium and renal function. Her laboratory showed a serum creatinine of 3.65 mg/dl and a renal sonography showed both kidneys with reduced size and hyperecogenic.
In May 2012 she had anemia, hypoalbuminemia, with a serum creatinine of 5.62 mg/dl (eGFR MDRD 9 ml/min) with a serum calcium of 12 mg/dl, 25(OH)D was 31.2 ng/ml, serum iPTH 11.6 pg/ml and calcitriol 88.3 pg/ml. Her serum converting enzyme determination was 91 ug/l (normal value up to 40 ug/l). An ecography of the mammary glands showed bilateral prosthesis with regular contours without signs of intra or extra capsular rupture. Nuclear magnetic resonance of the pelvis with focus in the bladder without contrast showed the presence of multiple nodular hypointense images in the subcutaneous tissue and in both gluteus with altered signal intensity in the muscle mass of both gluteus. Because of this, a biopsy was performed in the gluteal region looking for granulomas but the sample was insufficient.
A positron emission tomography with Fluor-desoxyglucose combined with helicoidal tomography with fusion of congruent cuts was performed showing evidence of metabolic activity at the gluteus muscle, isquiotibial quadriceps and internal gemellus of both legs. This was associated with a subtle density increment of the muscle tissue with dense striations, increased uptake in the subcutaneous tissue of both gluteal regions and anteromedial face of both thighs and calves.
The patient was treated with parenteral hydration, calcitonin and denosumab, with transient normalization of serum calcium. A renal function did not recover she began chronic hemodialysis.
Case 3
Fifty year old female who consulted in March 2012 because of decreasing renal function and hypercalcemia. In her laboratory analysis 8 months before, renal function was normal (serum creatinine 0.8–0.9 mg/dl). She had a history of left nephrectomy 20 years ago because of a renal tumor, for which she had received radiotherapy. She had performed multiple esthetic surgeries with implants and fillings. In September 2011 she had received methacrylate fillings in her legs.
Her laboratory analysis showed a serum creatinine of 2.2 mg/dl (creatinine clearance of 23 ml/min), total serum calcium 13.2 mg%, iPTH 15 pg/ml and calcitriol of 53.6 pg/ml. Repeated analysis confirmed her hypercalcemia with decreased renal function similar to previous values. Proteinogram was normal without light chains in the urine. X rays of the skull and both hands the same as a bone centelleogram were normal. Axial computed tomography of the thorax, abdomen and pelvis were normal. A magnetic resonance of both thighs showed nodular images at the subcutaneous tissue compatible with granulomas. She was treated with methyl prednisone 8 mg per day.
Case 4
Thirty nine year old female HIV+ for 18 years treated with antiretroviral therapy without any marker disease with viral load and CD4 in expected ranges. She presented a virological failure for which her medication was changed to tenofovir, atazanavir and ritonavir. She had performed multiple esthetic surgeries with implants and fillings with methacrylate in the lower extremities in 2009.
She consulted to the hospital in March 2010 because of severe reduction on renal function (creatinine clearance 19 ml/min) without changes after interruption of her medications. She had normal blood pressure; urine sediment was negative for hematuria, and a non-selective proteinuria of 0.6g/24hs. Laboratory workup showed hypercalcemia of 12mg/dl, 24-hr urinary calcium of 672mg, iPTHi 16 pg/ml, 25OHD 9 ng/ml; calcitriol 94 pg/ml (Normal: 18 a 60) and serum Cross laps 1492 pg/ml.
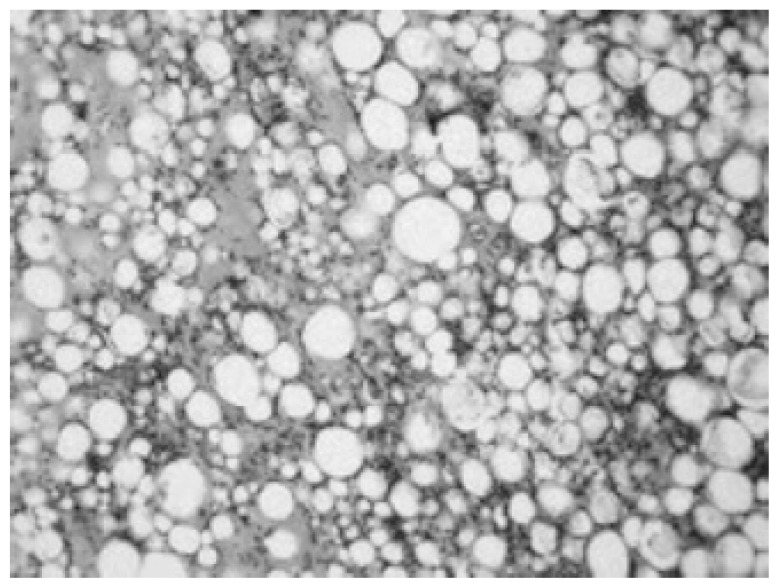
She had several complemmentary studies performed: 1) a percutaneous kidney biopsy that was informed as compatible with tenofovir toxicity associated with calcium deposition in glomerular capillaries and tubules 2) a bone densitometry that was normal. A positron emission tomography with Fluor desoxyglucose was performed that showed increased activity at the gluteus and thighs between muscles fibers suggesting infiltrates around methacrylate deposits (Figure 1). She had a muscle biopsy performed that showed granulomas around methacrylate deposits (Figure 2).
Figure 1.
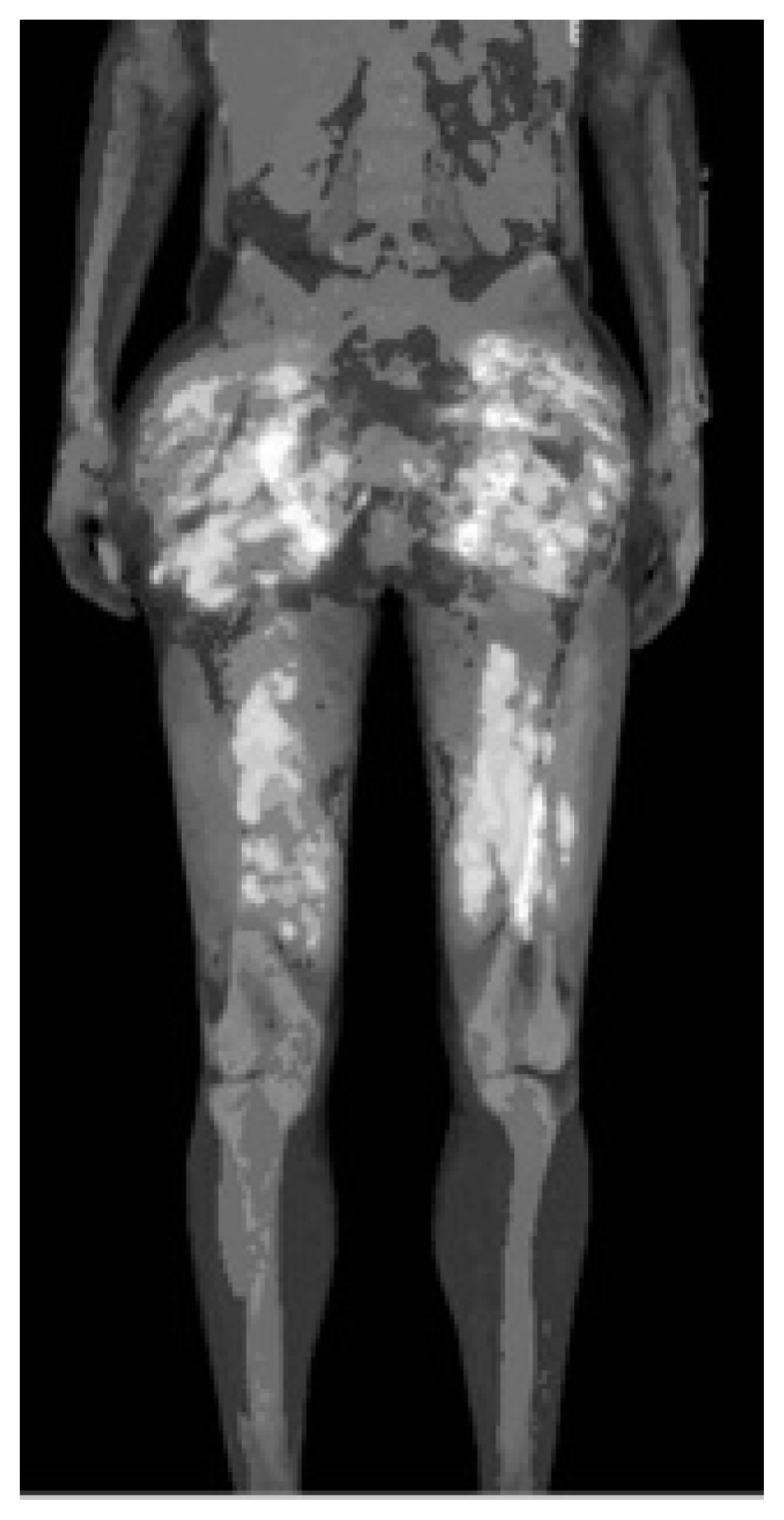
Positron Emission Tomography in case no 4.
Figure 2.
Muscle biopsy in patient no 4 showing the presence of methacrylate associated to the granuloma.
She began treatment with methyl prednisone with poor compliance with the medication. She had several readmissions to the hospital because of severe hypercalcemia and hypertension (170/100 mmHg) with decreased renal function (serum creatinine 2 mg/dl; eGFR MDRD 27ml/min). Due to the extension of the granulomatous infiltration it could not be completely removed surgically. She was treated with intralesional injections of triamcinolone 30 mg every 3 days for 9 days having a sustained response during 3 months with correction of her serum calcium (9.2 mg%) with a decrease in 1,25 (OH)2 vitamin D levels (61 pg/ml) decrease in serum Crosslaps (570 pg/ml) and improvement in renal function (creatinine clearance 50 ml/min).
At the present moment she has poor adherence to her diet and treatment, having readmission to the hospital because of hypercalcemia that are controlled local triamcinolone injections.
Discussion
In this case series we describe for the first time the production of severe hypercalcemia secondary to granulomatous reactions to methacrylate injections used in filling procedures.
Several substances are used in filling or infiltrative procedure with the purpose of increasing volume in certain areas of the body or face: polymetacrilate (Metacril®, Artecoll®), hyaluronic acid (for temporary fillings) and hyaluronic acid compounds (Juvederm®, Surgederm®) and silicones (7). Granulomatous reactions secondary to the filling materials are rare complications, most frequently found with permanent materials such as silicones (8), methacrylate and paraffin, and less frequently with biodegradable o resorbable materials. In a 10 year experience with silicone injections, 92 patients (9) developed granulomas subsequently in 13 injection site. The greatest part of the cases occurred in the first 12 months, but in some cases it took several years to appear and in one case it appeared 7 years after.
During the past 15 years, polymethyl methacrylate has been used as another synthetic permanent filling element to increase soft tissues volume. Salles et al. (10) reported 32 cases of complications, the greatest part in young females (mean age 43.6 years). In 10 of these cases they observed granulomas that usually presented as subacute complications 6 to 12 months after the procedure, although they can occur after a longer period of time (11). Other reports in the literature, show that this complication occurs independent of the site where the methacrylate is implanted (12, 13). The problem with this complication is that although is rare, it is frequently permanent as the granulomatous lesions are very difficult to remove surgically. Sometimes granulomas can be removed by the local intra lesional injection of corticoids (14). There exist reports in the literature of granulomatous reactions produced by silicones associated with hypercalcemia (8, 15–17) but as far as we know there are no registered cases of hypercalcemia induced by granulomas produced by methacrylate injection.
In this case series we report four young women that underwent methacrylate injections in gluteus, thighs and calves that developed granulomas with posterior appearance of hypercalcemia. This complication presented as subacute around 6 months after the procedure. The four patients have as common elements the presence of moderate to severe renal insufficiency, suppressed PTH and elevated calcitriol levels for the degree of renal function (Table 1). In the image studies, two patients presented in the nuclear magnetic resonance of the gluteus hypodense nodular images compatible with granulomas. Two patients had a PET performed showing increased metabolic activity in the muscles of the gluteal region compatible with granulomas (Figure 1). Two patients had a partial surgical resection of the gluteal lesions with the finding of methacrylate associated to foreign body granulomas (Figure 2). Hypercalcemia in these patients was treated with oral or intra lesional corticoids or with intravenous bisphosphonates with good response.
Table 1.
Demography and laboratory of the patients.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age (years) | 53 | 29 | 50 | 39 |
| Sex | female | female | female | female |
| Hypercalcemia | yes | yes | yes | yes |
| iPTH (pg/ml) | 3.5 | 11.6 | 15 | 16 |
| Calcitriol (pg/ml) | 55.5 | 88.3 | 53.6 | 94/61 |
| Creatinine mg% | 3.4 | 5.62 | 1.86 | 2.0 |
| eCCr (ml/min;MDRD) | 14 | 9 | 29 | 28 |
Although excessive intestinal absorption is a less frequent cause of hyperkalemia compared to that produced by excessive osteoclastic bone resorption, it plays an important role in the case of vitamin D intoxication, lymphomas or granulomas. The presence of extra renal 1 Alfa-hydroxylase in macrophages explains the elevated levels of calcitriol observed in our patients with granulomas, despite the important reduction in renal function (18, 19). It is probable that there is also a resorptive component in these patients as there is in patients with sarcoidosis in which the urinary excretion of calcium was seen to exceed the daily ingestion of calcium (20). Either the primary cause of hypercalcemia is excessive intestinal absorption of calcium, or accelerated bone resorption or both, the kidney is the primary defense mechanism against serum calcium increment, through an increase in urinary calcium elimination. As in the case of our patients, when the capacity of the kidney to excrete calcium is compromised, the patients become hypercalcemic.
Corticoids remain as the principal therapeutic option for hypercalcemia produced by excessive production of 1,25-(OH)2 D3 by the macrophages present in the sarcoid granulomas (21). Systemic corticoids inhibit the production of calcitriol as they suppress pro-inflammatory cytokines and quemokine production. The problem is that treatment frequently has to be continued for a long term to maintain normocalcemia, with associated side effects. Ketoconazole is an imidazole antifungal that inhibits the 1 alfa-hydroxylase from the macrophage and has been used to treat hypercalcemia associated to primary hyperparathyroidism (22), tumors, sarcoidosis (23, 24) and even tuberculosis (25). Chloroquin y hydroxichloroquin, on top of ketoconazol are drugs that can be used if the patient fails to respond or develops dangerous secondary effects due to therapy with steroids (26).
Although the prevalence of this complication with methacrylate injection is not common, hypercalcemia secondary to granulomatosis should be considered in the differential diagnosis of patients with hypercalcemia when there is a history of this procedure, and especially if they have an important reduction in their renal function.
References
- 1.Harrell GT, Fisher S. Blood chemical changes in Boeck’s sarcoid with particular reference to protein, calcium and phosphorus values. J Clin Invest. 1939;18:687–693. doi: 10.1172/JCI101084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Studdy PR, Bird R, Neville E, James DG. Biochemical findings in sarcoidosis. J Clin Pathol. 1980;33:528–693. doi: 10.1136/jcp.33.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gkonos PJ, London R, Hendler ED. Hypercalcemia and elevated 1,25-dihidroxyvitamin D levels in a patient with end-stage renal disease and active tuberculosis. N Engl J Med. 1984;311:1683–1685. doi: 10.1056/NEJM198412273112607. [DOI] [PubMed] [Google Scholar]
- 4.Hoffman VH, Horzeniowski OM. Leprosy, hypercalcemia and elevated serum calcitriol levels. Ann Inter Med. 1986;105:890–891. doi: 10.7326/0003-4819-105-6-890. [DOI] [PubMed] [Google Scholar]
- 5.Kantarijian HM, Saad MF, Estey EH, Samaan NA. Hypercalcemia in disseminated candidiasis. Am J Med. 1983;74:721–724. doi: 10.1016/0002-9343(83)91033-1. [DOI] [PubMed] [Google Scholar]
- 6.Adams JS, Singer FR, Gacad MA, et al. Isolation and structural identification of 1,25dihydroxyvitamin D3 produced by cultured alveolar macrophages in sarcoidosis. J Clin Endocrinol Metab. 1985;60:960–966. doi: 10.1210/jcem-60-5-960. [DOI] [PubMed] [Google Scholar]
- 7.Sturm LP, Cooter RD, Mutimer KL, Graham JC, Maddern GJ. A systematic review of dermal fillers for age-related lines and wrinkles. ANZ J Surg. 2011;81(1–2):9–17. doi: 10.1111/j.1445-2197.2010.05351.x. [DOI] [PubMed] [Google Scholar]
- 8.Kozeny GA, Barbato AL, Bansal VK, Vertuno LL, Hano JE. Hypercalcemia associated with silicone-induced granulomas. N Engl J Med. 1984;311(17):1103–5. doi: 10.1056/NEJM198410253111707. [DOI] [PubMed] [Google Scholar]
- 9.Wilkie TF. Late development of granuloma after liquid silicone injections. Plast Reconstr Surg. 1977;60(2):179–88. doi: 10.1097/00006534-197708000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Salles AG, Lotierzo PH, Gemperli R, Besteiro JM, Ishida LC, Gimenez RP, Menezes J, Ferreira MC. Complications after polymethylmethacrylate injections: report of 32 cases. Plast Reconstr Surg. 2008;121(5):1811–20. doi: 10.1097/PRS.0b013e31816b1385. [DOI] [PubMed] [Google Scholar]
- 11.Alcalay J, Alkalay R, Gat A, Yorav S. Late-onset granulomatous reaction to Artecoll. Dermatol Surg. 2003;29(8):859–62. doi: 10.1046/j.1524-4725.2003.29233.x. [DOI] [PubMed] [Google Scholar]
- 12.Kim KJ, Lee HW, Lee MW, Choi JH, Moon KC, Koh JK. Artecoll granuloma: a rare adverse reaction induced by microimplant in the treatment of neck wrinkles. Dermatol Surg. 2004;30:545–7. doi: 10.1111/j.1524-4725.2004.30174.x. [DOI] [PubMed] [Google Scholar]
- 13.Martínez-Bistrain R, Robles García V, Cornejo-Morales I. Granuloma de tórax secundario a metilmetacrilato. Acta Ortopédica Mexicana. 2010;24(1):28–32. [PubMed] [Google Scholar]
- 14.Conejo-Mir J, Sanz Guirado S, Muñoz A. Adverse Granulomatous Reaction to Artecoll Treated by Intralesional 5-Fluorouracil and Triamcinolone Injections. Dermatol Surg. 2006;32:1079–1082. doi: 10.1111/j.1524-4725.2006.32117.x. [DOI] [PubMed] [Google Scholar]
- 15.Altmann P, Dodd S, Williams A, Marsh F, Cunningham J. Silicone-induced hypercalcaemia in haemodialysis patients. Nephrol Dial Transplant. 1987;2(1):26–9. [PubMed] [Google Scholar]
- 16.Loke SC, Leow MK. Calcinosis cutis with siliconomas complicated by hypercalcemia. Endocr Pract. 2005;11(5):341–5. doi: 10.4158/EP.11.5.341. [DOI] [PubMed] [Google Scholar]
- 17.Schanz J, Flux K, Kircher C, Tsioga M, Hartschuh W, Nawroth PP, Rudofsky G. Mirror, mirror on the wall: hypercalcemia as a consequence of modern cosmetic treatment with liquid silicone. Med Sci Monit. 2012;18(2):CS5–7. doi: 10.12659/MSM.882450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zehnder D, Bland R, Williams MC, McNinch RW, Howie AJ, Stewart PM, Hewison M. Extrarenal expression of 25-hydroxyvitamin d(3)-1 alpha-hydroxylase. J Clin Endocrinol Metab. 2001;86(2):888–94. doi: 10.1210/jcem.86.2.7220. [DOI] [PubMed] [Google Scholar]
- 19.Hewison M, Burke F, Evans KN, Lammas DA, Sansom DM, Liu P, Modlin RL, Adams JS. Extra-renal 25-hydroxyvitamin D3-1 alpha-hydroxylase in human health and disease. J Steroid Biochem Mol Biol. 2007;103(3–5):316–21. doi: 10.1016/j.jsbmb.2006.12.078. [DOI] [PubMed] [Google Scholar]
- 20.Fallon MD, Perry HM, Teitelbaum SL. Skeletal sarcoidosis with osteopenia. Metab Bone Dis Res. 1981;3:171–174. doi: 10.1016/0221-8747(81)90004-7. [DOI] [PubMed] [Google Scholar]
- 21.Grutters JC, van den Bosch JM. Corticosteroid treatment in sarcoidosis. Eur Respir J. 2006;28(3):627–36. doi: 10.1183/09031936.06.00105805. [DOI] [PubMed] [Google Scholar]
- 22.Glass AR, Eil C. Ketoconazole-induced reduction in serum 1,25-dihydroxyvitamin D and total serum calcium in hypercalcemic patients. J Clin Endocrinol Metab. 1988;66(5):934–8. doi: 10.1210/jcem-66-5-934. [DOI] [PubMed] [Google Scholar]
- 23.Conron M, Beynon HL. Ketoconazole for the treatment of refractory hypercalcemic sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2000;17(3):277–80. [PubMed] [Google Scholar]
- 24.Bia MJ, Insogna K. Treatment of sarcoidosis-associated hypercalcemia with ketoconazole. Am J Kidney Dis. 1991;18(6):702–5. doi: 10.1016/s0272-6386(12)80613-5. [DOI] [PubMed] [Google Scholar]
- 25.Saggese G, Bertelloni S, Baroncelli GI, Di Nero G. Ketoconazole decreases the serum ionized calcium and 1,25-dihydroxyvitamin D levels in tuberculosis-associated hypercalcemia. Am J Dis Child. 1993;147(3):270–3. doi: 10.1001/archpedi.1993.02160270032013. [DOI] [PubMed] [Google Scholar]
- 26.Sharma OP. Hypercalcemia in granulomatous disorders: a clinical review. Curr Opin Pulm Med. 2000;6(5):442–7. doi: 10.1097/00063198-200009000-00010. [DOI] [PubMed] [Google Scholar]