Figure 1.
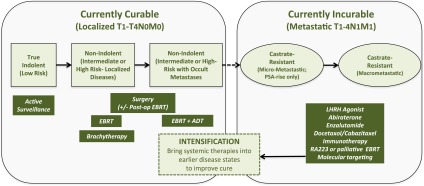
Curative and non-curative states in prostate cancer. Localized prostate cancers (CaPs) can be divided into low-, intermediate- and high-risk (including locally advanced) groups using T-category, pre-treatment prostate-specific antigen (PSA) level and the pathologic Gleason score. These groups have increasing probability of CaP-specific mortality. Low-risk tumours can be aggressively followed using active surveillance. By contrast, intermediate-risk tumours are treated with surgery, external beam radiotherapy (EBRT) or brachytherapy. In cases where a local recurrence occurs after surgery, patients can be treated with post-operative EBRT and convert a local failure into a cure. In high-risk CaP, there is an increased probability for occult systemic metastases, therefore systemic androgen deprivation [androgen-deprivation therapy (ADT)] is used in combination with EBRT. Palliative systemic therapy is the mainstay for patients with castrate-resistant disease in the micrometastatic or macrometastatic stages to increase progression-free survival by months. These therapies include additional ADT (including the use of newer agents, such as abiraterone and enzalutamide), chemotherapy, immunotherapy, systemic radionucleotides (RA233) and use of bespoke molecular-targeted agents. It is argued that an understanding of the genomic and microenvironmental factors that lead to occult metastases could drive intensification protocols using systemic agents in the localized CaP setting to improve the cure rates with radiotherapy and surgery. LHRH, luteinizing hormone-releasing hormone; Post-op, post-operative; RA223, radium-223.
