Abstract
Background:
In the skeletally immature population, the incidence of anterior cruciate ligament (ACL) injuries and ACL reconstructions appears to be increasing. Differences in surgical techniques, physiology, and emotional maturity may alter the rehabilitation progression and impact the outcomes when compared with adults. Reports of objective strength recovery and performance-based outcome measures after pediatric ACL reconstruction (ACLR) are limited.
Study Design:
Retrospective case series.
Level of Evidence:
Level 4.
Methods:
All patients that underwent all-epiphyseal ACLR from January 2008 to August 2010 were identified. Isokinetic peak quadriceps/hamstring torque values and functional performance measures in unilateral hopping tasks were extracted and compared with the noninjured limb. A limb symmetry index (LSI) of ≥90% was considered satisfactory.
Results:
Complete data were available for 16 patients (mean age, 12.28 years; range, 8.51-14.88 years). By a mean 7 months (range, 3.02-12.56 years) postoperatively, only 9 of 16 (56%) were able to achieve a satisfactory LSI for quadriceps strength. For hamstring strength, 15 of 16 (94%) were able to achieve satisfactory LSI. By a mean of 12 months (range, 5.39-24.39 months) postoperatively, only 6 of 16 subjects (38%) were able to achieve satisfactory performance on all functional hop tests. At a mean 15.42 months (range, 8.58-24.39 months) postsurgery, only 4 of 16 (25%) subjects were able to achieve an LSI of ≥90% on all testing parameters.
Conclusion:
For some pediatric patients, significant strength and functional deficits may be present at greater than 1 year after ACLR. This population may require more prolonged rehabilitation programs to allow for adequate recovery of strength and function because of unique characteristics of normal growth and development.
Keywords: knee, pediatric, anterior cruciate ligament, strength, functional hop test
Anterior cruciate ligament (ACL) injuries seem to be increasing in the skeletally immature population.8,21 Currently, there is no consensus in the literature regarding optimal management of these patients,11,12 as both early and delayed reconstruction pose inherent risks to the pediatric knee. However, the risks associated with delaying treatment and recent surgical advances have influenced many surgeons to favor earlier reconstruction within this population.5,11,18,21
The increase in surgical procedures performed within this population has led to a natural increase in the need for postoperative rehabilitation. Rehabilitation progression, functional performance measures, and outcomes after ACL reconstruction (ACLR) rehabilitation are well defined within the adult or skeletally mature population.3,6,9,20 However, at this time, there is a lack of performance-related measurements for skeletally immature individuals. The purpose of this study was to report the rate of strength recovery, degree of strength symmetry achieved, and limb symmetry in functional performance measures in a group of skeletally immature patients after an all-epiphyseal ACLR.
Methods
Institutional review board approval was obtained. A retrospective chart review was conducted to identify all patients 7 to 15 years old who underwent an all-epiphyseal ACLR between the dates of January 2007 and September 2010. All patients were treated by a single, board-certified pediatric sports medicine orthopaedic surgeon (TJG) specially trained in performing all-epiphyseal ACLR. Information pertaining to patient demographics, concomitant injury, surgical information, strength, and functional rehabilitation progression was gathered. Strength recovery and functional performance were expressed as a limb symmetry index (LSI) comparing operated and nonoperated limbs for isokinetic data and functional hop scores, respectively. If multiple tests were available for an individual, the test that indicated the best performance at the earliest time point was utilized for analysis.
Isokinetic Strength Testing
Peak torque isokinetic testing (Biodex System 3 isokinetic dynamometer; Biodex Medical Systems, Shirley, New York) data for knee flexion and extension were collected in a seated position at a testing speed of 180 deg/s. Quadriceps and hamstring isokinetic strength data were expressed as a ratio by dividing the peak torque value of the involved leg by the peak torque value of the uninvolved leg, then multiplying by 100. Calculation of an LSI is representative of common practice in reporting strength symmetry after ACLR.6
Functional Hop Test Battery
Functional knee braces were utilized during testing when prescribed by the physician. For each portion of the testing battery (Figure 1), practice trials were permitted prior to the test to allow for task learning and patient confidence. For statistical analysis purposes, an average of each of the 4 functional test ratios was calculated, with 90% or higher being indicative of a “passing” score, as this percentage is representative of criteria utilized to assess for readiness for progressive return to unrestricted sport activities after ACLR.1,9
Figure 1.
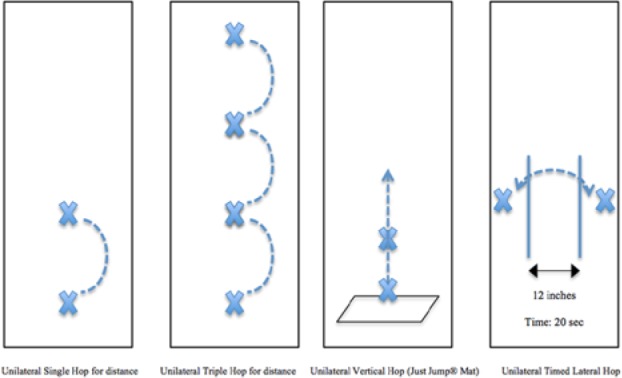
Schematic of the functional hop testing protocol.
Single Hop for Distance4
The results of 3 hops were averaged, and side-to-side comparisons are expressed as a ratio of distance hopped in the surgical to the nonsurgical limb.
Triple Hop for Distance13
The results of 3 hops were then averaged, and side-to-side comparisons are expressed as a ratio of distance hopped in the surgical to the nonsurgical limb.
Unilateral Vertical Jump
A Just Jump (Probotic Inc, Huntsville, Alabama) was utilized to measure vertical jump height. The results of 3 hops were then averaged, and side-to-side comparisons are expressed as a ratio of vertical distance hopped in the surgical to the nonsurgical limb.
Unilateral Timed Lateral Hop
Two lines were placed on the floor 12 inches apart. The subject was allotted 20 seconds to perform a maximal number of 1-legged lateral hops over this distance. The subject must fully clear the entire 12-inch distance. If the subject touched a line at any point, that hop within the test was not counted and it was considered an error. The subject was tested 1 time per side, allowing adequate rest time between testing of limbs to allow for recovery. The lateral timed hop is expressed in the amount of contacts performed minus the amount of errors recorded by the examiner. Side-to-side comparisons are expressed as a ratio of corrected contacts performed on the surgical to the nonsurgical limb.
Results
Of the 47 patients eligible for inclusion, complete data were available for 16 patients (mean age, 12.28 years; range, 8.51-14.88 years) (Appendix 1, available at http://sph.sagepub.com/content/suppl). All subjects’ physical maturity levels were Tanner Stage 2 or under. An autologous hamstring graft was utilized for all subjects included in this series.
To assess strength recovery, isokinetic strength was evaluated at a mean 7.1 months (range, 3.02-12.56 months) postsurgery (Appendix 2, available at http://sph.sagepub.com/content/suppl). At that time, only 9 of 16 (56.25%) patients were able to achieve a satisfactory LSI for quadriceps strength (Figure 2). Over the same time interval, 15 of 16 (94%) patients demonstrated satisfactory hamstring strength. At a mean 12.8 months (range, 5.39-24.39 months) postsurgery, only 6 of 16 subjects (38%) were able to achieve satisfactory performance of ≥90% on all functional tests (Appendices 3 and 4, available at http://sph.sagepub.com/content/suppl). Overall, at an average of 15.42 months (range, 8.58-24.39 months) postsurgery, only 4 of 16 (25%) subjects were able to achieve an LSI of ≥90% on all testing parameters (strength and functional tests).
Figure 2.
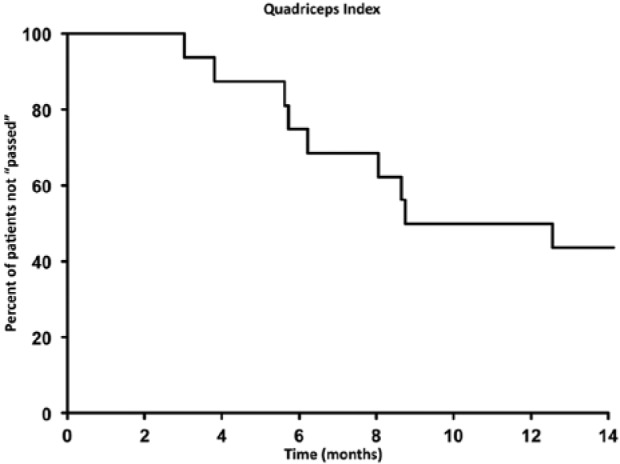
Kaplan-Meier curves for not passing limb symmetry index (LSI) criteria of at least 90% on quadriceps isokinetic strength test.
Discussion
The results from this study demonstrate that significant quadriceps strength and overall lower extremity functional performance deficits may exist within this pediatric population after ACLR. These data suggest that it is more difficult to restore quadriceps strength symmetry than hamstring symmetry within this population. This observation is intriguing, as some studies have noted that utilizing an autologous hamstring graft, as was done with all subjects included in this study, may delay strength recovery of the hamstrings muscle group.22 While we are unable to firmly establish the cause of this delay in quadriceps strength recovery, physiological and psychological characteristics of the preadolescent patient likely contribute. Given the importance of full functional recovery prior to return to sports, these noted continued strength and functional deficits have significant implications for a safe return to play and subsequent potential reinjury in this population.
Impaired quadriceps strength is a significant deficit that occurs early after ACLR, and restoration is important to maximize functional ability.7,16 Early strength gains after ACLR are related to decreased muscular inhibition and improved motor unit functioning, while later strength gains are more related to true muscle hypertrophy.1 Prepubescent children lack circulating androgens. The majority of strength gains within this population are because of improved motor unit activation and coordination as opposed to true muscle hypertrophy.14,15 Only 56.25% (9 of 16) of the subjects were able to achieve the 90% quadriceps strength symmetry goal by a mean of 7 months postoperatively. These results are similar to those found by Wells et al19 in teenagers (mean age, 15.93 years) where 59% were able to achieve a threshold of 85% quadriceps LSI in less than 6 months. Strength recovery after ACLR in a group of adults showed that 55% and 78% were able to achieve at least 90% quadriceps strength symmetry as early as 3 and 6 months postoperatively, respectively.6
Psychological factors may also play a role in the recovery of pediatric patients after ACLR. Pediatric patients often exhibit significant anxiety, both pre- and postoperatively, which may limit their motivation or ability to work through some painful situations during the rehabilitation process. In addition, the recovery from ACLR is a long and arduous process. While many pediatric athletes are used to extended sports seasons, they often have difficulty maintaining the sustained effort over the complete postoperative period required to achieve a full functional recovery. Insurance limitations necessitating transition to an unsupervised rehabilitative home exercise program can also delay the final phases of recovery.
Finally, differences in the postoperative protocol for skeletally immature patients may also impact the time frame for strength recovery after ACLR. The current postoperative protocol (Appendix 5, available at http://sph.sagepub.com/content/suppl) involves a period of limited weightbearing for the first 4 to 6 weeks postoperatively to allow for bony accommodation within the epiphysis from the tunnels. This delay in weightbearing may limit functional activation of the quadriceps muscle and lead to delayed recovery of muscular function after surgery.
Many have advocated for the use of isokinetic strength and unilateral hop testing LSI of at least 85% to 90% to return to sports after ACLR.2,9 Our results indicate that only 25% (4 of 16) of patients were able to meet passing criteria by 15 months postoperative. These results were compared with a prior study in a group of adults using the Fisher exact test. Significant differences (P < 0.001) existed between these 2 age groups, with 73% of the adult group achieving ≥90% performance on strength and similar functional measures at 12 months postoperatively.6 In addition, 10 of 16 (63%) subjects in this study failed to pass return-to-sport criteria because of inadequate performance on the functional hop test conglomerate. This result strengthens the standpoint that multiple modes of testing are necessary to determine the true functional ability and readiness to return to sports after ACLR.
The results of the current investigation suggest that a more prolonged postoperative rehabilitation course may be warranted in the skeletally immature population after ACLR to achieve satisfactory criteria for return to unrestricted activity.
Although the factors related to ACL rerupture are not fully understood, incomplete rehabilitation resulting in decreased limb function may predispose athletes to reinjury.2 Utilizing only self-reported scales as a sole determinant for functional activity progression without assessing strength deficits and abnormal movement patterns may place the athlete at greater risk of reinjury. With the significant delay in functional recovery after ACLR noted in this pediatric population, extended times for return to play should be expected. Early return to unrestricted activity without adequate recovery of muscular function and performance may be 1 factor contributing to the higher retear rate in younger patients.10,17
There are several limitations within our study. Because of the retrospective nature of this investigation, the rehabilitation that each patient received was not ideally controlled. Though the same surgeon treated each patient and a copy of a postoperative protocol (Appendix 5) was issued to each treating therapist, the degree in which the recommended treatment outline was adhered to remains unknown. In addition, because of the tertiary referral nature of the practice and insurance issues, 31 of 47 patients who underwent all-epiphyseal ACLR within the given time frame were not included in the analysis because of inconsistent physician follow-up and/or incomplete strength and functional testing data. Likewise, postsurgical strength and functional testing was not standardized in relation to time from surgery, which could have allowed for a more thorough and more precise time-based analysis.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
Institutional review board approval was obtained for all aspects of this study.
References
- 1. Adams D, Logerstedt DS, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42:601-614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697-1705 [DOI] [PubMed] [Google Scholar]
- 3. Barber SD, Noyes FR, Mangine R, DeMaio M. Rehabilitation after ACL reconstruction: function testing. Orthopedics. 1992;15:969-974 [DOI] [PubMed] [Google Scholar]
- 4. Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop Relat Res. 1990;(255):204-214 [PubMed] [Google Scholar]
- 5. Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja RK. Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 1992;8:229-233 [DOI] [PubMed] [Google Scholar]
- 6. Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40:141-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim KM, Croy T, Hertel J, Saliba S. Effects of neuromuscular electrical stimulation after anterior cruciate ligament reconstruction on quadriceps strength, function, and patient-oriented outcomes: a systematic review. J Orthop Sports Phys Ther. 2010;40:383-391 [DOI] [PubMed] [Google Scholar]
- 8. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582-2587 [DOI] [PubMed] [Google Scholar]
- 9. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ; Orthopaedic Section of the American Physical Therapist Association. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40:A1-A37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526-531 [DOI] [PubMed] [Google Scholar]
- 11. Milewski MD, Beck NA, Lawrence JT, Ganley TJ. Anterior cruciate ligament reconstruction in the young athlete: a treatment algorithm for the skeletally immature. Clin Sports Med. 2011;30:801-810 [DOI] [PubMed] [Google Scholar]
- 12. Mohtadi N, Grant J. Managing anterior cruciate ligament deficiency in the skeletally immature individual: a systematic review of the literature. Clin J Sport Med. 2006;16:457-464 [DOI] [PubMed] [Google Scholar]
- 13. Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513-518 [DOI] [PubMed] [Google Scholar]
- 14. Ozmun JC, Mikesky AE, Surburg PR. Neuromuscular adaptations following prepubescent strength training. Med Sci Sports Exerc. 1994;26:510-514 [PubMed] [Google Scholar]
- 15. Ramsay JA, Blimkie CJ, Smith K, Garner S, MacDougall JD, Sale DG. Strength training effects in prepubescent boys. Med Sci Sports Exerc. 1990;22:605-614 [DOI] [PubMed] [Google Scholar]
- 16. Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42:750-759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246-251 [DOI] [PubMed] [Google Scholar]
- 18. Vavken P, Murray MM. Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy. 2011;27:704-716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wells L, Dyke JA, Albaugh J, Ganley T. Adolescent anterior cruciate ligament reconstruction: a retrospective analysis of quadriceps strength recovery and return to full activity after surgery. J Pediatr Orthop. 2009;29:486-489 [DOI] [PubMed] [Google Scholar]
- 20. Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20:60-73 [DOI] [PubMed] [Google Scholar]
- 21. Wojtys EM, Brower AM. Anterior cruciate ligament injuries in the prepubescent and adolescent athlete: clinical and research considerations. J Athl Train. 2010;45:509-512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Xergia SA, McClelland JA, Kvist J, Vasiliadis HS, Georgoulis AD. The influence of graft choice on isokinetic muscle strength 4-24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:768-780 [DOI] [PubMed] [Google Scholar]


