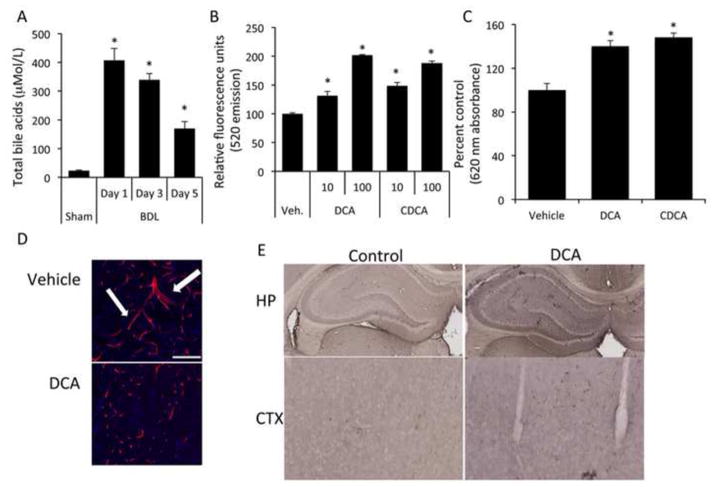
Figure 2.
Bile acids are increased in the circulation of bile duct ligated rats and have the capacity to permeabilize the blood brain barrier both in vitro as well as in vivo. (A) Circulating bile acids were measured with a colorimetric assay in sham and bile duct ligated rats 5 days post-surgery. BDL rats have ~7 fold higher circulating bile acids than sham rats. (* denotes p<0.05, n=3) (B) Confluent monolayers were treated with vehicle or chenodeoxycholic acid, or deoxycholic acid (10μM or 100μM) for 24 hours and permeability was measured via fluorescein isothiocyanate-dextran flux. (* denotes p<0.001, n=6) (C) Permeability was measured in vivo via Evan’s blue assay in rats tail vein-injected with either vehicle, chenodeoxycholic acid or deoxycholic acid for 5 days. chenodeoxycholic acid- or deoxycholic acid-treated rats have a significant increase in blood brain barrier permeability as measured by Evan’s blue concentration compared to vehicle treated rats. (* denotes p<0.05, an n of at least 3 was used) (D) Brain slices were stained with a SMI-71 antibody (red) and counterstained with DAPI (blue) in vehicle- and deoxycholic acid-treated rats to visualize cerebral microvessels. Similar to sham rats, vehicle-treated rats have long continuous staining with several bifurcations (white arrows) compared to deoxycholic acid-treated rats that have discontinuous staining. Scale bar represents 100μm. (E) Albumin immunohistochemistry was performed on rats injected with vehicle or deoxycholic acid for 5 days. Rats treated with deoxycholic acid show a higher degree of albumin immunoreactivity in brain slices, in particular the hippocampus and cortex regions, indicating a disruption of the BBB. (BDL; bile duct ligation, DCA; deoxycholic acid, CDCA; chenodeoxycholic acid, UDCA; ursodeoxycholic acid HP; hippocampus, CTX, cortex)