Abstract
Pyogenic liver abscesses usually occur in association with a variety of diseases. Rarely, liver abscess has been reported as the presenting manifestation of colonic tubulovillous adenoma. We report two cases of pyogenic liver abscess without hepatobiliary disease or other obvious etiologies except that one had a history of diabetes mellitus (DM). The pathogen in the patient with DM was Klebsiella pneumonia (KP). In both of the patients, ileus developed about two to three weeks after the diagnosis of liver abscess. Colonoscopy revealed large polypoid tumors with pathological findings of tubulovillous adenoma in both cases. Two lessons were learned from these two cases: (1) an underlying cause should be aggressively investigated in patients with cryptogenic liver abscess; (2) DM could be one of the etiologies but not necessarily the only cause of KP liver abscess.
Keywords: Pyogenic liver abscess, Klebsiella pneumonia, Colonic tubulovillous adenoma
INTRODUCTION
Pyogenic liver abscess is usually related to hepatobiliary tract disease or intra-abdominal infections including cholecystitis, suppurative cholangitis, suppurative pylephlebitis, appendicitis, diverticulitis and peritonitis[1-3]. Recently, colorectal cancer without obvious infection was considered as one of the uncommon etiologies of liver abscess[4,5]. Furthermore, liver abscess was reported as the presenting manifestation of colonic tubulovillous adenoma[6]. However, there are a growing number of reports suggesting a relationship between diabetes mellitus (DM) and Klebsiella pneumonia (KP) liver abscess which indicate that a deficiency in the hosts’ defense mechanism could be the etiology of this liver infection[7-9]. We hereby report two cases of pyogenic liver abscess both of which were found to have colonic tubulovillous adenoma two to three weeks later after the diagnosis of liver abscess. The association of pyogenic liver abscess and colonic tubulovillous adenoma and the implications of these two cases are discussed.
CASE REPORT
CASE 1
A 67-year-old man, who was referred from a local hospital, was admitted to our hospital because of fever, chill, and right upper abdominal pain for seven days. On physical examination, his initial body temperature was 37.9oC and blood pressure was 124/67 mmHg. Light palpation of the abdomen revealed tenderness and mild rebounding pain on epigastric and right upper areas, but no abdominal mass was felt. Significant laboratory data included a leukocyte count of 26,330/μL (normal range = 4000-10,400/μL ), a hemoglobin of 9.5 gm/dL (normal range = 12-16 gm/dL), an aspartate aminotransferase (AST) of 73 IU/L (normal range = 5-34 IU/L), an alanine aminotranferase (ALT) of 79 IU/L (normal range = 0-40 IU/L), a fasting blood sugar of 118 mg/dl (normal range = 70-110 mg/dL), a total bilirubin of 1.03 mg/dL (normal range = 0.2-1.3 mg/dL), a C-Reactive Protein (CRP) of 17.02 mg/dL (normal <0.8 mg/dL), and a carcinoembryonic antigen (CEA) level of 0.33 ng/dL (normal <5 ng/dL).
Abdominal ultrasonography (US) and computed tomography (CT) showed a 4-cm liver abscess in left lobe of liver (Figure 1A). After three sets of blood cultures were completed and broad-spectrum antimicrobial therapy was initiated, CT-guided percutaneous drainage of the liver abscess was performed and pus liked material was aspirated and sent for bacterial culture. However, blood and pus were all negative for bacterial growth. As antimicrobial treatment was continued, the patient’s clinical condition improved rapidly and fever subsided four days later. Then the drainage catheters were removed and the patient was discharged on the 14th d of hospitalization.
Figure 1.
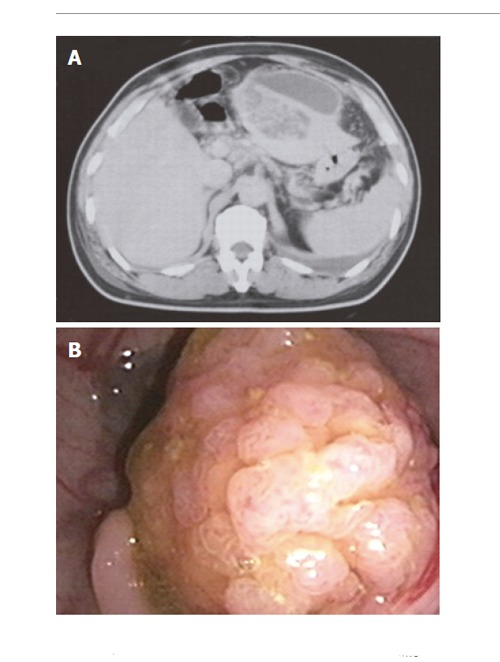
Case 1. A: Enhancement abdominal computed tomography (CT) showed a 4-cm liver abscess in left lobe of the liver; B: Colonofibroscopy showed a 3-cm pedunculated polyp in the sigmoid colon.
One week later, he was admitted again with a chief complaint of abdominal fullness. Physical examination showed a distended abdomen with hypertympanic abdominal sounds on percussion. Plain films of the abdomen disclosed evidence of a paralytic ileus with a suspected obstruction at the level of the sigmoid colon. Colonoscopy was performed which showed a 3-cm pedunculated polyp in the sigmoid colon (Figure 1B). Polypectomy was performed and pathological examination revealed tubulovillous adenoma with mild dysplasia. The patient continued to do well during a follow-up period of 6 mo.
CASE 2
An 84-year-old woman with a history of DM using no regular medication for several years was admitted to the hospital because of fever and right upper abdominal dull pain which was followed by a change of consciousness for the two days preceding admission. On physical examination, her initial body temperature was 37.7oC and blood pressure was 79/30 mmHg. Mild tenderness in the right upper abdomen was noted during performance of light palpation, but no abdominal mass was felt. Significant laboratory data included a leukocyte count of 17,870/μL, a hemoglobin of 12.7 mg/dL, an AST of 59 IU/L, an ALT of 58 IU/L, a fasting blood sugar of 348 mg/dL, a total bilirubin of 2.31 mg/dL, a CRP level of 32.82 mg/dL, and a CEA level of 6.72 ng/dL. Abdominal US and CT showed a 5-cm liver abscess in right lobe of the liver (Figure 2A).
Figure 2.
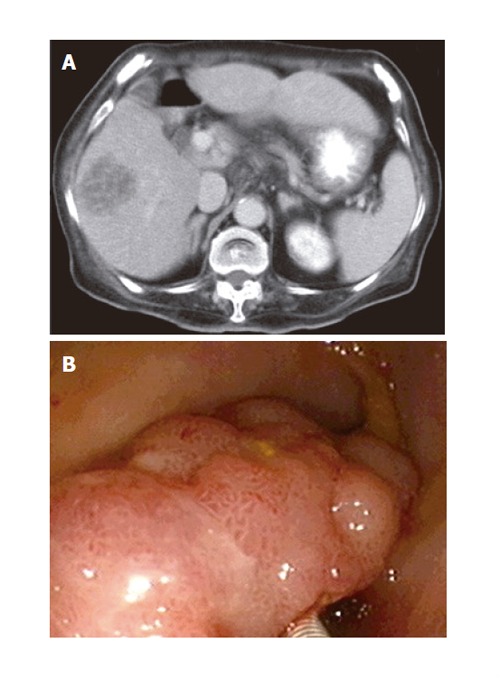
Case 2. A: Enhancement abdominal computed tomography showed a 5-cm liver abscess in right lobe of the liver; B: Colonofibroscopy showed a 3-cm polypoid tumor in the sigmoid colon.
Since the patient could not cooperate for US or CT-guided aspiration, broad-spectrum antimicrobial treatment was started after three sets of blood cultures were performed. The results of blood cultures were positive for Klebsiella pneumonia (KP), which was sensitive to the formerly prescribed antibiotics. The patient’s clinical condition improved gradually and fever subsided 10 d later. On the 14th d of hospitalization, abdominal fullness developed and the plain film of abdomen showed evidence of ileus with a suspected obstruction at the level of the distal colon. Colonoscopy was performed and showed a 3-cm polypoid tumor in the sigmoid colon (Figure 2B). Polypectomy was not done because of technical difficulty. A biopsy was performed and eight pieces of tissue were taken for pathological examination. The pathological findings were consistent with tubulovillous adenoma. Since ileus resolved spontaneously and the patient’s general physical condition was not good, the patient’s family refused to have further treatment. Her general condition was stable during a follow-up period of two months.
DISCUSSION
The etiologies and pathogenesis of liver abscesses have changed significantly over the past several decades[1-3,10-11]. Recent reports suggest that pyogenic liver abscess might be a warning indicator of silent colonic cancer[4,5,12-14], therefore, patients with liver abscess but without apparent etiologies, as in Case 1 of this report, should have further examination. In addition, non-growth in cultures of blood samples and abscess aspirate in Case 1 could be due to the following two possibilities: (1) the patient had been partially treated at an outside hospital; (2) the pathogen of the liver abscess might be an anaerobe that was most probably originated from the colon. Therefore, although a rapid improvement was noted, a complete evaluation of the GI tract should be performed in Case 1 as per the suggestion of Cohen et al[4].
Nevertheless, colonoscopy was performed because of ileus and the examination revealed a large colonic tubulovillous adenoma in the sigmoid colon instead of a “silent colonic cancer”. Whether colonic adenoma could be an etiology of pyogenic liver abscess remains to be elucidated. In addition to our report, there is only one other report of pyogenic liver abscess as the presentation of colonic villous adenoma[6]. The mechanism for explaining colonic adenoma as an etiology of liver abscess may be the same as that of the colonic cancer, i.e., there are mucosal defects present on the colonic lesions (cancers or adenomas) that allow a route for bacteria invasion into the portal system with subsequent hematogenous spread to the liver.
In recent years, pyogenic liver abscesses have occurred more frequently in immunodeficient patients, including those receiving intensive chemotherapy for hematological or solid malignancies, patients with immunosuppressive therapy after organ transplantation[15] and, especially, patients with DM[8-9]. Case 2 was a DM patient who had a solitary liver abscess caused by KP. As previous reports showed, KP liver abscesses tend to occur in DM patients who did not have any predisposing factors for the development of liver abscess, therefore, the diagnostic procedures and management in Case 2 seemed reasonable. However, the unexpected occurrence of ileus due to a large colonic villous adenoma indicated that the presence of DM could not completely exclude other possible etiologies of liver abscess.
In conclusion, for patients with cryptogenic liver abscess, an underlying cause should be aggressively searched for. DM could be one of the etiologies but not necessarily the only cause of KP liver abscess.
Footnotes
S- Editor Pravda J and Guo SY L- Editor Elsevier HK E- Editor Liu WF
References
- 1.Sherman JD, Robbins SL. Changing trends in the casuistics of hepatic abscess. Am J Med. 1960;28:943–950. doi: 10.1016/0002-9343(60)90203-5. [DOI] [PubMed] [Google Scholar]
- 2.Miedema BW, Dineen P. The diagnosis and treatment of pyogenic liver abscesses. Ann Surg. 1984;200:328–335. doi: 10.1097/00000658-198409000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stain SC, Yellin AE, Donovan AJ, Brien HW. Pyogenic liver abscess. Modern treatment. Arch Surg. 1991;126:991–996. doi: 10.1001/archsurg.1991.01410320077010. [DOI] [PubMed] [Google Scholar]
- 4.Cohen JL, Martin FM, Rossi RL, Schoetz DJ Jr. Liver abscess. The need for complete gastrointestinal evaluation. Arch Surg. 1989;124:561–564. doi: 10.1001/archsurg.1989.01410050051009. [DOI] [PubMed] [Google Scholar]
- 5.Lonardo A, Grisendi A, Pulvirenti M, Della Casa G, Melini L, Di Gregorio C, Nasi G, Sarti M, Tamborrino E, Lonardo F. Right colon adenocarcinoma presenting as Bacteroides fragilis liver abscesses. J Clin Gastroenterol. 1992;14:335–338. doi: 10.1097/00004836-199206000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Leiba A, Apter S, Avni I, Osherov A, Thaler M, Grossman E. [Pyogenic liver abscess--an unusual presentation of colonic villous adenoma] Harefuah. 2003;142:336–337, 399. [PubMed] [Google Scholar]
- 7.Rayfield EJ, Ault MJ, Keusch GT, Brothers MJ, Nechemias C, Smith H. Infection and diabetes: the case for glucose control. Am J Med. 1982;72:439–450. doi: 10.1016/0002-9343(82)90511-3. [DOI] [PubMed] [Google Scholar]
- 8.Wang JH, Liu YC, Lee SS, Yen MY, Chen YS, Wang JH, Wann SR, Lin HH. Primary liver abscess due to Klebsiella pneumoniae in Taiwan. Clin Infect Dis. 1998;26:1434–1438. doi: 10.1086/516369. [DOI] [PubMed] [Google Scholar]
- 9.Yang CC, Yen CH, Ho MW, Wang JH. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol Immunol Infect. 2004;37:176–184. [PubMed] [Google Scholar]
- 10.Gyorffy EJ, Frey CF, Silva J Jr, McGahan J. Pyogenic liver abscess. Diagnostic and therapeutic strategies. Ann Surg. 1987;206:699–705. doi: 10.1097/00000658-198712000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Branum GD, Tyson GS, Branum MA, Meyers WC. Hepatic abscess. Changes in etiology, diagnosis, and management. Ann Surg. 1990;212:655–662. doi: 10.1097/00000658-199012000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teitz S, Guidetti-Sharon A, Manor H, Halevy A. Pyogenic liver abscess: warning indicator of silent colonic cancer. Report of a case and review of the literature. Dis Colon Rectum. 1995;38:1220–1223. doi: 10.1007/BF02048342. [DOI] [PubMed] [Google Scholar]
- 13.Tzur T, Liberman S, Felzenstein I, Cohen R, Rivkind AI, Almogy G. Liver abscesses caused by Streptococcus milleri: an uncommon presenting sign of silent colonic cancer. Isr Med Assoc J. 2003;5:206–207. [PubMed] [Google Scholar]
- 14.Matsushita M, Hajiro K, Okazaki K, Takakuwa H, Nishio A. Endophthalmitis with brain, lung, and liver abscesses associated with an occult colon cancer. Am J Gastroenterol. 2000;95:3664–3665. doi: 10.1111/j.1572-0241.2000.03405.x. [DOI] [PubMed] [Google Scholar]
- 15.Marcus SG, Walsh TJ, Pizzo PA, Danforth DN Jr. Hepatic abscess in cancer patients. Characterization and management. Arch Surg. 1993;128:1358–1364; discussion 1364. doi: 10.1001/archsurg.1993.01420240066012. [DOI] [PubMed] [Google Scholar]


