To the Editor
I read with interest the recent review article by Brenner1 published in the British Journal of Radiology entitled “What we know and what we don't know about cancer risks associated with radiation doses from radiological imaging”. I am concerned that the references Brenner used to claim the carcinogenicity of low-dose radiation were outdated, discredited, incomplete or irrelevant, resulting in painting a misleading picture of the current state of knowledge on the health effects of low-dose radiation. For example, in referring to increased cancer risks in low-dose cohorts of atomic bomb survivors, Brenner used publications from 20072 and 2011,3 when newer updated data on the survivors had been published in 2012 by Ozasa et al.4 The newer data, with improved statistics, display a significant non-linearity (curvature) in the dose–response curve arising from lower than expected cancer mortality rates for the doses near 50 cGy, as indicated by the following statements in the article: “the curvature over the 0–2 Gy range … has become significant with longer observation” on p. 234 and “the apparent upward curvature appears to be related to relatively lower than expected risks in the dose range 0.3–0.7 Gy, a finding without a current explanation” on p. 238. Although the linear no-threshold model used by Ozasa et al4 can provide no explanation for the reduction of cancers in this dose region, an analysis has shown that the data are consistent with the concept of radiation hormesis,5 implying a reduction of cancer risk for low radiation doses. In addition, although Ozasa et al4 claimed zero dose to be the best estimate of the threshold dose for cancer risk from radiation, such a conclusion resulted from their use of a restricted functional form for dose–response in performing the dose-threshold analysis. An analysis with a more general functional form has shown that the presence of a dose threshold cannot be excluded.5 A recently published analysis of the atomic bomb survivor data using artificial neural networks has also shown the presence of a threshold dose that varies with the type of cancer and the reduction of some cancers at low doses.6
Another reference Brenner used for justifying low-dose radiation cancer concerns is the 15-country study of radiation workers.7 Although the study showed slightly increased cancer risk among the radiation workers exposed to low-dose radiation, the conclusion relied heavily on the higher cancer risk observed in the Canadian data.8 A report on the reanalysis of the Canadian data published more than 2 years ago stated that the data had been found to be defective and was being withdrawn.9 Without the Canadian data, the 15-country study would not show an increased risk of cancer from low-dose radiation.10
A third data set Brenner used was the Oxford study11 of childhood cancers, a case–control study that showed increased risk of childhood cancers following prenatal radiation. Major deficiencies have been identified in this study, and publications have raised doubts about a causal link between prenatal radiation and childhood leukaemias observed in such studies, since cohort studies involving much higher radiation doses in atomic bomb survivors have failed to show the increased risk of childhood leukaemias.12 Other large cohort studies have also failed to show any increased risk of cancers.13 Since cohort studies are considered to be higher in the hierarchy of evidence than case–control studies, Brenner's exclusive reference to the Oxford study11 of childhood cancers without discussion of the cohort data presented a misleading picture on the current state of knowledge for the carcinogenic risks of prenatal diagnostic radiation.
A fourth type of data that Brenner referred to was from the studies of childhood cancers in children who had undergone CT scans.14,15 Major issues have been identified in these studies, including features of the study design.16,17 One major problem with such studies is that there is a potential for confounding by reverse causation. As described by Walsh et al,16 the early appearance of solid cancers after the first CT scan, the absence of excess breast cancers (expected to occur owing to the high radiosensitivity of the breast) and the significant excesses of melanoma and Hodgkin's lymphoma (which have not been observed in larger radiation studies) indicate reverse causation could be the reason for the observed increased cancer risk in the Mathews et al14 study. One major deficiency of the Pearce et al15 study is that they did not have a control group.17 A comparison of leukaemia rates reported in the general paediatric population in the UK with the rates observed in the Pearce et al15 study indicates that the children who had undergone CT scans did not have a higher incidence of leukaemias.17
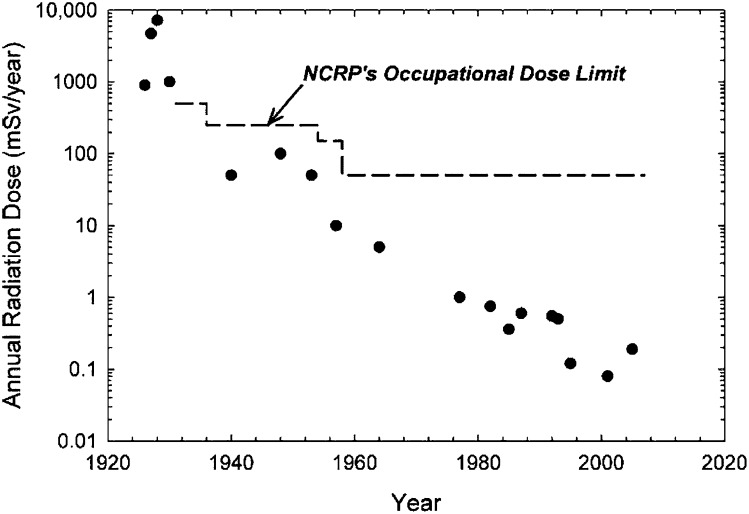
Regarding very low doses of radiation, i.e.<1 mGy, Brenner has used irrelevant data (i.e. data from much higher exposures, as discussed below) to infer that the effects of such radiation doses are unknown. While referring to cancer risks from such doses, Brenner lamented the absence of data at these doses and said that this has led to uncertainty and controversy regarding the health effects at very low doses. Brenner then stated “As an example, three studies of historical mortality risks in radiologists concluded that there was a statistically significant increase in risk, a statistically significant decrease in risk or that there was no significance difference compared with other physicians”. These studies, however, correspond to different time periods with different levels of average annual radiation doses to the radiologists (Figure 1).18 The studies of radiologists entering into service when the average dose to radiologists was 0.9–9 Sv per year showed increased cancer mortality, while studies with radiologists averaging initial annual doses of 5–10 cSv showed reduced cancer mortality and studies, with cohorts having initial annual doses of approximately 1 mSv showed no effect on cancer mortality. Hence, the statement Brenner made referring to these data “This diversity is not surprising given the limited power of such studies, and interpretation of all results at very low doses, whether in vitro or in vivo, should be undertaken with much caution” does not have any validity. On the other hand, these data illustrate the cancer preventive effect of radiation for annual doses of approximately 5 cSv, carcinogenic effect of annual doses greater than approximately 1 Sv and no effect on cancers from annual doses of approximately 1 mSv.
Figure 1.
Average annual occupational effective radiation dose estimates and time trends of average annual doses in radiologists. The National Council on Radiation Protection and Measurements (NCRP) recommendations for whole-body doses are shown for comparison with the reported radiation doses. Reproduced from Linet et al18 with permission from the Radiation Research Society.
Brenner concludes that there is a small risk of cancer from higher dose examinations, such as CT scans, does not have any credible supporting evidence. Nor is there uncertainty of cancer risk from very low doses, as claimed by Brenner. On the other hand, considerable amounts of evidence exist for the cancer preventive effect of the radiation doses corresponding to several CT scans in a year (using a nominal dose of 1 cSv per CT scan), with the risk of cancer increasing only for doses corresponding to hundreds of CT scans in a year. Hence, his recommendation to use the lowest possible doses for radiological examinations does not have any justification either, since the reduced image quality from such efforts may adversely affect the diagnostic utility of the studies, potentially harming the patient while not reducing the risk of cancer.
Unjustified carcinogenic concerns raised in articles by Brenner19 and others20,21 over the past few decades have led to a tremendous expenditure of resources towards dose-monitoring and dose-reduction efforts in diagnostic imaging. The carcinogenic concerns regarding diagnostic imaging may well have harmed patients' health because of their refusal to undergo indicated diagnostic imaging studies or owing to physicians prescribing diagnostic studies using suboptimal imaging modalities. Readers are advised to scrutinize such articles critically and challenge their conclusions. Professionals and professional organizations in the field of diagnostic imaging should affirm the safety of diagnostic imaging when such unjustified claims are made and assure the public confidently that the radiation doses from diagnostic imaging are safe and do not cause any cancers.
REFERENCES
- 1.Brenner DJ. What we know and what we don't know about cancer risks associated with radiation doses from radiological imaging. Br J Radiol 2014; 43 doi: 10.1259/bjr.20130629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Preston DL, Ron E, Tokuoka S, Funamoto S, Nishi N, Soda M, et al. Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat Res 2007; 168: 1–64. doi: 10.1667/RR0763.1 [DOI] [PubMed] [Google Scholar]
- 3.Preston DL. From epidemiology to risk factors. Proceeding of the Third MELODI Workshop; November 2–4 2011; Rome, Italy. Available from: www.melodi-online.eu/doc/preston.pdf. [Google Scholar]
- 4.Ozasa K, Shimizu Y, Suyama A, Kasagi F, Soda M, Grant EJ, et al. Studies of the mortality of atomic bomb survivors, report 14, 1950–2003: an overview of cancer and noncancer diseases. Radiat Res 2012; 177: 229–43. [DOI] [PubMed] [Google Scholar]
- 5.Doss M. Linear no-threshold model vs. radiation hormesis. Dose Response 2013; 11: 480–97. doi: 10.2203/dose-response.13-005.Doss [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sasaki MS, Tachibana A, Takeda S. Cancer risk at low doses of ionizing radiation: artificial neural networks inference from atomic bomb survivors. J Radiat Res Dec 2013. Epub ahead of print. doi: 10.1093/jrr/rrt133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, et al. The 15-country collaborative study of cancer risk among radiation workers in the nuclear industry: estimates of radiation-related cancer risks. Radiat Res 2007; 167: 396–416. doi: 10.1667/RR0553.1 [DOI] [PubMed] [Google Scholar]
- 8.Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, et al. Risk of cancer after low doses of ionising radiation: retrospective cohort study in 15 countries. BMJ 2005; 331(7508): 77. doi: 10.1136/bmj.38499.599861.E0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CNSC. INFO-0811. Verifying Canadian nuclear energy worker radiation risk: a reanalysis of cancer mortality in Canadian nuclear energy workers (1957–1994) summary report, Canadian Nuclear Safety Commission; 2011 [updated June 2011; cited 1 September 2013]. Available from: http://nuclearsafety.gc.ca/pubs_catalogue/uploads/INFO-0811-Verifying-Canadian-Nuclear-Energy-Worker-Radiation-Risk-A-Reanalysis-of-Cancer-Mortality-in-Canadian-Nuclear-Energy-Workers-1957-1994_e.pdf.
- 10.Zablotska LB, Lane RS, Thompson PA. A reanalysis of cancer mortality in Canadian nuclear workers (1956–1994) based on revised exposure and cohort data. Br J Cancer 2014; 110: 214–23. doi: 10.1038/bjc.2013.592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Streffer C, Shore R, Konermann G, Meadows A, Uma Devi P, Preston Withers J, et al. Biological effects after prenatal irradiation (embryo and fetus). A report of the International Commission on Radiological Protection. Ann ICRP 2003; 33: 5–206. [PubMed] [Google Scholar]
- 12.Belson M, Kingsley B, Holmes A. Risk factors for acute leukemia in children: a review. Environ Health Perspect 2007; 115: 138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brent RL. Carcinogenic risks of prenatal ionizing radiation. Semin Fetal Neonatal Med Dec 2013. Epub ahead of print. doi: 10.1016/j.siny.2013.11.009 [DOI] [PubMed] [Google Scholar]
- 14.Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 2013; 346: f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pearce MS, Salotti JA, Howe NL, McHugh K, Kim KP, Lee C, et al. CT scans in young people in great Britain: temporal and descriptive patterns, 1993–2002. Radiol Res Pract 2012; 2012: 594278. doi: 10.1155/2012/594278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walsh L, Shore R, Auvinen A, Jung T, Wakeford R, Mathews JD, Forsthye AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680, 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 2013; 346: f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen M. Cancer risks from CT radiation: is there a dose threshold? J Am Coll Radiol 2013; 10: 817–19. doi: 10.1016/j.jacr.2013.03.029 [DOI] [PubMed] [Google Scholar]
- 18.Linet MS, Kim KP, Miller DL, Kleinerman RA, Simon SL, Berrington de Gonzalez A. Historical review of occupational exposures and cancer risks in medical radiation workers. Radiat Res 2010; 174: 793–808. doi: 10.1667/RR2014.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brenner DJ, Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med 2007; 357(22): 2277–84. doi: 10.1056/NEJMra072149 [DOI] [PubMed] [Google Scholar]
- 20.Berrington de Gonzalez A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med 2009; 169(22): 2071–7. doi: 10.1001/archinternmed.2009.440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berrington de Gonzalez A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 2004; 363(9406): 345–51. doi: 10.1016/S0140-6736(04)15433-0 [DOI] [PubMed] [Google Scholar]