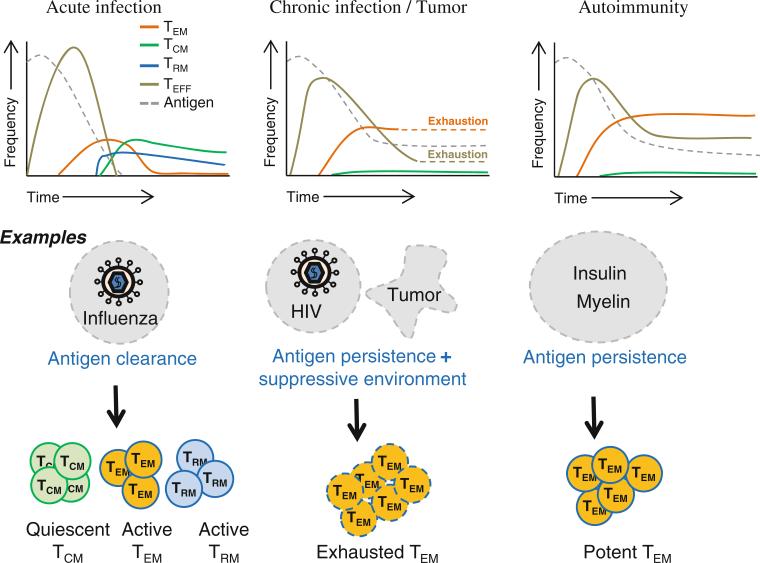
Fig. 1.
Predominant subsets of memory T cells in infections, tumors and autoimmune diseases. (1) Persistence of antigens in chronic infections, tumor microenvironment and autoimmune disease settings leads to the increased formation of the effector memory T (TEM) cell subset. (2) TEM cells are exhausted in settings of chronic infections and tumors. (3) In autoimmune diseases, TEM cells are not exhausted, making them highly pathogenic. Their longevity and active functionality perpetuate autoimmune damage. (4) Persistence of antigens in chronic infections, tumors and autoimmune disease settings diminishes the formation of the central memory T (TCM) cells and possibly the tissue-resident memory T (TRM) cell subsets. (5) Immune control genes such as CTLA4 are highly polymorphic, and the polymorphisms that may promote TEM cells are well preserved in human populations despite their deleterious potential in causing autoimmune diseases. These genetic variations suggest that the differentiation of autoimmune TEM cells may have evolved for their beneficial potential in clearing unhealthy cells in chronic infections or boosting anti-tumor immunity. Further studies are needed to bridge the genetic discoveries to immunobiology and pathophysiology