Abstract
Objective
The objective of this study was to characterise the incidence rates of herpes zoster (HZ), also known as shingles, and risk of complications across the world.
Design
We systematically reviewed studies examining the incidence rates of HZ, temporal trends of HZ, the risk of complications including postherpetic neuralgia (PHN) and HZ-associated hospitalisation and mortality rates in the general population. The literature search was conducted using PubMed, EMBASE and the WHO library up to December 2013.
Results
We included 130 studies conducted in 26 countries. The incidence rate of HZ ranged between 3 and 5/1000 person-years in North America, Europe and Asia-Pacific, based on studies using prospective surveillance, electronic medical record data or administrative data with medical record review. A temporal increase in the incidence of HZ was reported in the past several decades across seven countries, often occurring before the introduction of varicella vaccination programmes. The risk of developing PHN varied from 5% to more than 30%, depending on the type of study design, age distribution of study populations and definition. More than 30% of patients with PHN experienced persistent pain for more than 1 year. The risk of recurrence of HZ ranged from 1% to 6%, with long-term follow-up studies showing higher risk (5–6%). Hospitalisation rates ranged from 2 to 25/100 000 person-years, with higher rates among elderly populations.
Conclusions
HZ is a significant global health burden that is expected to increase as the population ages. Future research with rigorous methods is important.
Keywords: EPIDEMIOLOGY, VIROLOGY
Strengths and limitations of this study.
We comprehensively reviewed the global burden of herpes zoster.
We found a similar age-specific incidence of herpes zoster in North America, Europe and Asia-Pacific; however, there is a scarcity of research from other regions.
Because the quality of the study, study design and study population varied widely across studies, we could not synthesise the data quantitatively.
Introduction
Herpes zoster (HZ), also known as shingles, is typically characterised by painful, blistering dermatomal rash.1 2 The estimated lifetime risk of HZ in the general population is approximately 30%, with the risk increasing sharply after 50 years of age.3 After conducting a careful long-term observational study in the 1960s, Hope-Simpson4 showed that HZ results from reactivation of the varicella-zoster virus (VZV) in sensory ganglia after a long latency period following primary infection from varicella (chickenpox). In some patients particularly in the elderly, the pain continues to persist after the rash heals and develops into postherpetic neuralgia (PHN), which is the most common complication. PHN causes physical disability, emotional distress and interference with daily activities and sleep.5 HZ also causes neurological sequelae, HZ ophthalmicus (HZO) with eye involvement or disseminated disease. Severe cases of these complications often require hospitalisation.
A live-attenuated VZV vaccine (ZOSTAVAX by Merck) has been demonstrated to significantly reduce the incidences of HZ and PHN in addition to the severity and duration of pain associated with HZ.6 Public health interventions that promote healthy ageing are increasingly becoming more important, as the elderly population is growing rapidly worldwide. Over the next half century, the proportion of people ≥60 years of age is projected to double, reaching more than 20% of the total population in all regions of the world.7 Moreover, the prevalence of disability in the elderly populations is increasing across the world.8
It is essential for healthcare practitioners and health policymakers to be informed by the best available and up-to-date evidence on the HZ burden of disease. In a previous review by Thomas and Hall9, there were limited population-based studies on HZ incidence. Since then, many studies have been conducted across countries to examine the incidence rates and temporal trends of HZ. Other reviews have been restricted to specific geographic regions.10 11 Moreover, to the best of our knowledge, there has been no systematic review of studies examining the risk of complications and hospitalisation. The objective of this study is to characterise the incidence rates of HZ and risk of complications across the world. We systematically reviewed studies examining the incidence rates of HZ, temporal trends of HZ, risk of HZ complications including PHN and HZ-associated hospitalisation and mortality rates in the general population.
Methods
Literature search
We performed a literature search in PubMed, EMBASE, and the WHO's Global Health Library Regional Index up to December 2013. For PubMed, we used Medical Subject Headings (MeSH) and the title terms ‘herpes zoster’, ‘zoster’ or ‘shingles’ in combination with the term ‘incidence’. We also searched eligible articles using MeSH and the title terms ‘postherpetic neuralgia’ or ‘post-herpetic neuralgia’. We used the same search strategy with text terms in EMBASE and the WHO library. We manually searched the references cited by the retrieved articles and review articles for additional references. Two investigators (KK and BG) independently conducted a systematic review of the literature, assessed study eligibility and extracted data. Discrepancies were settled through discussion with a third investigator (CJA).
Inclusion and exclusion criteria
We included studies examining the incidence of HZ, risk of PHN, risk of a recurrent episode of HZ, risk of HZO, HZ-associated hospitalisation or HZ-associated mortality. For studies examining the efficacy or effectiveness of vaccination against HZ, we included estimates of incidence rates among unvaccinated individuals. We did not apply language restrictions. We did not include studies limited to children, immunocompromised populations (eg, HIV, cancer and chronic kidney disease) or patients on immunosuppressive therapy (eg, corticosteroids). We also excluded review articles and case reports.
Data extraction
We developed a standard abstraction form for data extraction. We extracted information regarding authors, publication year, journal, country, study design, study year(s), population, number of cases, number at risk, case definition, case ascertainment, incidence rates of HZ (per 1000 person-years), risk of PHN and other complications, HZ-associated hospitalisation rates and HZ-associated mortality rates. For studies on incidence that did not report 95% CI, we computed exact 95% CI.
Results
After conducting a literature search, we included 130 studies conducted in 26 countries in this review (figure 1). There were 63 studies on the incidence of HZ from 22 countries3 4 6 12–71; 25 studies on trends of HZ from 7 countries3 12 15–19 23–25 27 28 49 53 65 68 72–80; 60 studies on PHN from 19 countries3 4 6 12 18 33–36 38 40 42 43 46 54 56 60–63 69 81–118; 9 studies on HZ recurrence from 5 countries4 12 13 57 60 119–122; 12 studies on HZO from 5 countries12 35 43 61 123–130; 28 studies on hospitalisation rates from 14 countries24 26 27 30 37 41 44 46 48 52 55 56 58 62–64 72 73 76 77 131–137 and 10 studies on mortality rates from 10 countries.26 30 37 41 44 48 58 62 134 138
Figure 1.
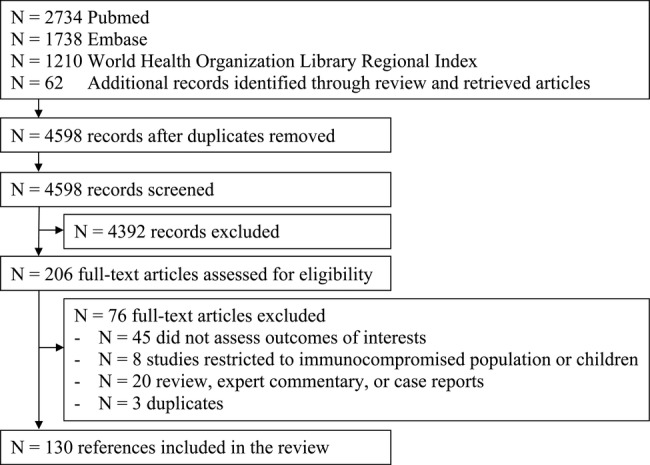
Study selection.
Incidence rates of HZ
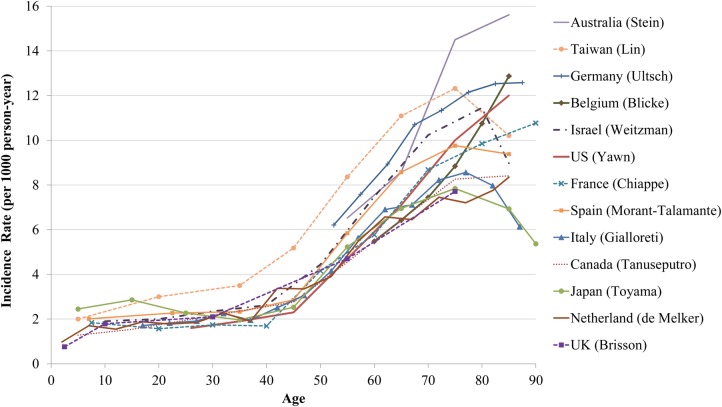
Studies examining the incidence rates of HZ were conducted in countries from North America (N=18), Europe (N=33), Asia (N=7), South America (N=3) and the Middle East (N=2; table 1). The incidence rate of HZ ranged between 3 and 5/1000 person-years in North America, Europe and Asia-Pacific, based on studies using prospective surveillance, electronic medical record data or administrative data with medical record review. The age-specific incidence rates of HZ were similar across countries, with a steep rise after 50 years of age (figure 2). The incidence rate was about 6–8/1000 person-years at 60 years of age and 8–12/1000 person-years at 80 years of age. We observed an increase in the reported incidence rate over time within a country. For example, studies conducted more than 20 years ago in the USA by Ragozzino et al12 and Donahue et al13 showed lower rates compared with studies conducted in recent years. It is noteworthy that prospective population-based studies that identified relatively small numbers of patients with HZ (eg, by Scott et al,33 Paul and Thiel,39 Di Legami et al55 and Lionis et al59) estimated lower incidence compared with other studies.
Table 1.
Incidence of HZ
| Country | Author | Study design and population | Case ascertainment | Year | HZ cases | Age | Incidence 1000 person- years | 95% CI |
|---|---|---|---|---|---|---|---|---|
| USA | Ragozzino | Medical records database in Minnesota | ICD-9 confirmed by medical records | 1945–1959 | 590 | All ages | 1.31 | 1.15 to 1.35* |
| USA | Donahue | Health maintenance organisation claims database in Massachusetts | ICD-9 confirmed by medical records | 1990–1992 | 1075 | All ages | 2.15 | 2.02 to 2.28* |
| USA | Insinga | MarketScan claims database in the USA | ICD-9 | 2000–2001 | 9152 | All ages | 3.20 | 3.10 to 3.20 |
| USA | Mullooly | Kaiser Northwest health maintenance organisation claims database | ICD-9 multiplied by positive predictive value | 1997–2002 | 9895 | All ages | 3.69 | 3.58 to 3.82 |
| USA | Yih | Annual random-digit telephone survey in Massachusetts | Survey from patients | 1999–2003 | 194 | All ages | 4.33 | 3.72 to 4.93* |
| USA | Jumaan | Health maintenance organisation claims database in Washington | ICD-9 | 1992–2002 | 357 | All ages | 3.71 | |
| USA | Oxman | Zostavax trial in the control group | Notified by physicians and PCR/culture confirmation | 1998–2001 | 642 | ≥60 years | 11.12 | |
| USA | Yawn | Retrospective population-based study confirmed by medical records in Minnesota | ICD-9 confirmed by medical records | 1996–2001 | 1669 | ≥22 years | 3.60 | 3.40 to 3.70 |
| USA | Rimland | National Veterans Affairs claims database | ICD-9 | 2000–2007† | 28 710 | All ages | 5.22 | |
| USA | Leung | MarketScan claims database | ICD-9 | 1993–2006† | 48 000 | All ages | 4.40 | 4.30 to 4.40 |
| USA | Tseng | Kaiser Southern California health maintenance organisation claims database in the unvaccinated group | ICD-9 | 2007–2009 | 4606 | ≥60 years | 13.0 | 12.6 to 13.3 |
| USA | Langan | Medicare claims database in the unvaccinated group | ICD-9 | 2007–2009 | 19 385 | ≥65 years | 15.1 | 14.9 to 15.3 |
| USA | Chen | Commercial, Medicare and Medicaid MarketScan claims database | ICD-9 | 2005–2009 | 435 378 | ≥18 years | 4.82 | 4.81 to 4.84 |
| USA | Hales | Medicare claims database | ICD-9 | 1992–2010† | 281 317 | ≥65 years | 14.2 | 14.0 to 14.5 |
| Canada | Brisson | Administrative claims database in Manitoba | ICD-9 | 1979–1997† | NA | All ages | 3.48 | |
| Canada | Russell | Health insurance claims database in Alberta | ICD-9/ICD-10 | 1986–2002† | NA | All ages | 4.30 | |
| Canada | Edgar | Administrative claims database in British Columbia | ICD-9 | 1994–2003 | 114 596 | All ages | 2.89 | |
| Canada | Tanuseputro | Administrative claims database in Ontario | ICD-9 | 1992–2010 | 686 763 | All ages | 3.23 | |
| Canada | Russell | Health insurance claims database in Alberta | ICD-9/ICD-10 | 1994–2010† | 213 265 | All ages | 4.50 | |
| UK | Hope-Simpson | Prospective population-based study in Cirencester | Medical records by GP | 1947–1962 | 192 | All ages | 3.39 | |
| UK | Ross | Prospective population-based study in Glasgow | Notified by 10 GPs | 1972–1973 | 87 | All ages | 2.40 | |
| UK | Brisson | RCGP database in England and Wales | ICD-9 medical records by GPs | 1979–1997† | NA | All ages | 3.82 | |
| UK | Brisson | RCGP database in England and Wales | ICD-9 medical records by 69 GPs | 1991–2000 | NA | All ages | 3.73 | |
| UK | Fleming | RCGP database in England and Wales | ICD-9 medical records by GPs | 1994–2001† | 14 532 | All ages | 3.90 | |
| UK | Chapman | RCGP database in England and Wales | ICD-9 medical records by GPs | 1994–2001 | NA | ≥15 years | 3.95 | |
| UK | Scott | Prospective population-based study in East London | Notified by 18 GPs and PCR confirmation | NA | 186 | All ages | 1.85 | |
| UK | Gauthier | GPRD in UK | Medical records by 603 GPs | 2000–2006 | 27 225 | ≥50 years | 5.23 | 5.17 to 5.29 |
| France | Chidiac | Prospective sentinel surveillance | Notified by 4635 GPs and 513 dermatologists | 1997–1998 | 8103 | All ages | 4.80 | |
| France | Czernichow | Retrospective population-based study | Survey from 744 GPs | 1998 | 605 | All ages | 3.20 | 3.00 to 3.40 |
| France | Gonzalez- Chiappe | Prospective sentinel surveillance | Notified by 1200 GPs | 2005–2008 | 2375 | All ages | 3.82 | 3.64 to 4.05 |
| France | Mick | Retrospective population-based study | Survey from 231 GPs, 41 dermatologists and 15 neurologists | 2005 | 777 | ≥50 years | 8.99 | 8.34 to 9.64 |
| Germany | Paul | Prospective population-based study in Ansbach | Notified by GPs, dermatologists and others | 1992–1993 | 152 | All ages | 2.26 | |
| Germany | Schiffner-Rohe | National Statutory Health Insurance claims database | ICD-10 | 2004 | 1170 | ≥50 years | 9.80 | 9.20 to 10.40 |
| Germany | Ultsch | National Statutory Health Insurance claims database | ICD-10 | 2007–2008 | 374 645 | ≥50 years | 9.60 | 9.56 to 9.63 |
| Germany | Ultsch | National Statutory Health Insurance claims database | ICD-10 | 2004–2009 | 5384 | All ages | 5.79 | 5.64 to 5.93 |
| The Netherlands | Opstelten | Huisartsen Netwerk Utrecht database in six locations | Medical records from 22 GPs | 1994–1999 | 837 | All ages | 3.40 | 2.90 to 3.90 |
| The Netherlands | de Melker | Prospective sentinel surveillance | Notified by 43 GPs | 1998–2001 | NA | All ages | 3.25 | |
| The Netherlands | Opstelten | National survey of physicians | Medical records from 104 GPs | 2001 | 1080 | All ages | 3.22 | 3.00 to 3.40 |
| The Netherlands | Pierik | Retrospective population-based study in Almere | Medical records from 22 GPs | 2004–2008 | 3371 | All ages | 4.75 | 4.06 to 5.44 |
| Switzerland | Richard | Prospective sentinel surveillance | Notified by 250 physicians | 1998–2001 | 2236 | All ages | 2.36 | |
| Belgium | Bilcke | Retrospective population-based study | Notified by 150 GPs | 2000–2007 | NA | All ages | 3.78 | |
| Spain | Pérez-Farinós | Prospective sentinel surveillance in Madrid | Notified by GPs | 1997–2004† | 1798 | All ages | 3.59 | 3.22 to 3.97 |
| Spain | García Cenoz | Primary care database in Navarre | Medical records from GPs | 2005–2006 | 4959 | All ages | 4.15 | |
| Spain | Cebrián-Cuenca | Prospective population-based study in Valencia | Notified by 25 GPs | 2006–2007 | 146 | ≥14 years | 4.10 | 3.40 to 4.70 |
| Spain | Morant-Talamante | Electronic medical record database in Valencia | ICD-9 | 2007–2010 | 85 586 | All ages | 4.60 | 4.57 to 4.63 |
| Spain | Esteban-Vasallo | Electronic medical record in the Madrid regional public health system | ICPC | 2005–2012† | 211 650 | All ages | 4.82 | |
| Italy | di Luzio Paparatti | Retrospective population-based study | Survey from 71 GPs | 1995 | 408 | ≥15 years | 4.14 | 3.75 to 4.56 |
| Italy | Di Legami | Prospective population-based study in Piedmont | Notified by 24 GPs | 2004 | 46 | ≥14 years | 1.74 | 1.28 to 2.32 |
| Italy | Gialloreti | National primary-care database (Societa Italiana Medici Generici) | Medical records from 342 GPs | 2003–2005 | 5675 | All ages | 4.31 | 4.11 to 4.52 |
| Iceland | Helgason | Prospective population-based study | Notified by 62 GPs | 1990–1995 | 462 | All ages | 2.00 | 1.80 to 2.20 |
| Sweden | Studahl | Swedish National Pharmacy register | Prescriptions for antiviral medications | 2006–2010 | 127 832 | All ages | 2.70 | |
| Greece | Lionis | Prospective population-based study in rural Crete | Notified by 19 GPs | 2007–2009 | 58 | All ages | 1.60 | |
| Israel | Weitzman | Maccabi Healthcare Services claims database | ICD-9 | 2006–2010 | 28 977 | All ages | 3.46 | |
| Saudi Arabia | Alakloby | Medical records from the dermatology clinic | Medical charts from the dermatologist | 1988–2006 | 141 | All ages | 6.20 | 5.18 to 7.22* |
| Australia | Stein | National GP database (Bettering the Evaluation of Care and Health) | Medical records of GPs | 2000–2006 | 379 | ≥50 years | 9.67 | 8.66 to 10.68 |
| Taiwan | Jih | Taiwan National Health Insurance claims database | ICD-9 | 2000–2006 | 34 280 | All ages | 4.89 | 4.76 to 5.04* |
| Taiwan | Lin | Taiwan National Health Insurance claims database | ICD-9 | 2000–2005 | 672 782 | All ages | 4.97 | 4.96 to 4.98 |
| Taiwan | Chao | Taiwan National Health Insurance claims database | ICD-9 | 2000–2008 | 11 908 | All ages | 5.67 | |
| South Korea | Park | NA | NA | 1999–2003 | 1089 | All ages | 2.98 | |
| South Korea | Choi | Health Insurance claims database (estimated prevalence) | ICD-10 | 2003–2007 | 2 431 744 | All ages | 9.97 | |
| Japan | Toyama | Prospective population-based study in Miyazaki | Notified by 46 dermatology clinics | 1997–2006 | 48 388 | All ages | 4.15 | 4.12 to 4.19* |
| Argentina | Vujacich | Medical records from the ID reference centre | Medical charts from IDs | 2000–2005 | 302 | All ages | 3.57 | 3.17 to 3.97* |
| Brazil | Castro | Medical records from the dermatology clinic | Medical charts from the dermatologist | 1987–1989 | 469 | All ages | 5.62* | |
| Colombia | Gaitan | Medical records from the oncology, radiology and nuclear medicine centre | Medical charts from patients without cancer | NA | 75 | NA | 6.50* |
*We computed the overall estimate or 95% CI based on the study results.
†The estimate from the latest study year.
GP, general practitioner; GPRD, general practice research database; HZ, herpes zoster; ICD, International Classification of Diseases; ICPC, International Classification For Primary Care; RCGP, Royal College of GPs.
Figure 2.
Age-specific incidence rate of herpes zoster in North America, Europe and Asia-Pacific.
Trends of HZ incidence
In the USA, studies conducted during the postvaricella vaccination era showed inconsistent results, with some showing no change in incidence but others reporting an increase in HZ incidence, suggesting a potential impact of varicella vaccination (table 2). However, Leung et al,19 Hales et al23 and Yawn et al75 examined trends over a longer period and found that incidence rates increased continuously across all age groups before the introduction of the varicella vaccination programme and continued to increase throughout the postvaccination era. These studies concluded that the increase was not due to the varicella vaccination programme. Most studies conducted in Canada, the UK, Spain, Taiwan and Japan reported an increase in the incidence of HZ over the past decade often occurring in the absence of the national varicella vaccination programmes.24 25 49 65 68 Several studies in Australia suggested increasing trends in HZ outpatient visits or hospitalisation during prevaricella and postvaricella vaccination eras.76 77 79
Table 2.
Temporal trends of herpes zoster
| Country | Author | Study periods | Varicella vaccination era | Trends |
|---|---|---|---|---|
| USA | Ragozzino | 1945–1959 | Pre | Incidence increased from 1.1 to 1.5/1000 person-years between 1945–1949 and 1955–1959 |
| USA | Jumaan | 1992–2002 | Pre and post (1996–) | Incidence did not change between 1992 and 2002 |
| USA | Yih | 1998–2003 | Post | Incidence increased from 2.8 to 5.3/1000 person-years between 1999 and 2003 |
| USA | Mullooly | 1997–2002 | Post | Incidence did not change between 1997 and 2002 |
| USA | Yawn | 1996–2005 | Post | Incidence increased from 3.2 to 4.1/1000 person-years between 1996–1997 and 2000–2001 |
| USA | Patel | 1993–2004 | Pre and post | Hospitalisation rate did not change during 1993–2000 but increased between 2001 and 2004 |
| USA | Jackson | 1992–2004 | Pre and post | Hospitalisation rate did not change during 1992–2004 |
| USA | Civen | 2000–2006 | Post | Incidence increased between 2000 and 2006 among unvaccinated adolescents 10–19 years |
| USA | Rimland | 2000–2007 | Post | Incidence increased from 3.1 to 5.2/1000 person-years between 2000 and 2007 |
| USA | Yawn | 1945–2008 | Pre and post | Incidence increased from 0.8/1000 person-years in 1945–1947, to 1.6/1000 person-years in 1980–1982, to 3.0/1000 person-years in 2005–2007 |
| USA | Leung | 1993–2006 | Pre and post | Incidence increased from 1.7 to 4.4/1000 person-years between 1993 and 2006 |
| USA | Hales | 1992–2010 | Pre and post | Incidence increased from 10.0 to 13.9/1000 person-years between 1992 and 2010 in adults ≥65 years |
| Canada | Brisson | 1979–1997 | Pre | Incidence increased from 2.6 to 3.5/1000 person-years between 1979 and 1997 |
| Canada | Russell | 1986–2002 | Pre and post (2001–) | Incidence increased from 2.8 to 4.2/1000 person-years between 1986 and 2002 |
| Canada | Tanuseputro | 1992–2010 | Pre and post | Incidence did not change during 1992–2009 |
| Canada | Russell | 1994–2010 | Pre and post | Incidence increased from 3.5 to 4.5/1000 person-years between 1994 and 2010 |
| UK | Brisson | 1979–1997 | Pre | Incidence increased from 3.2 to 3.9/1000 person-years between 1979 and 1997 |
| Spain | Perez-Farinos | 1997–2004 | Pre | Incidence increased from 2.5 to 3.6/1000 person-years between 1997 and 2004 |
| Spain | Esteban-Vasallo | 2005–2012 | Pre and post (2006–) | Incidence increased from 3.6 to 4.8/1000 person-years between 2005 and 2012 |
| Australia | Macintyre | 1993–1999 | Pre | Hospitalisation rate increased between 1993 and 1999 |
| Australia | Carville | 1995–2007 | Pre and post (2005–) | Hospitalisation rate increased from 6.3 to 9.1/100 000 person-years between 1995 and 2007 |
| Australia | Nelson | 1998–2009 | Pre and post | Incidence increased from 1.7 to 2.4/1000 person-years between 1998 and 2008 |
| Australia | Jardine | 1998–2007 | Pre and post | Hospitalisation rate did not change during 1992–2009 |
| Taiwan | Chao | 2000–2008 | Pre and post | Incidence increased from 4.5 to 6.9/1000 person-years between 2000 and 2008 |
| Taiwan | Wu | 2000–2009 | Pre and post | Incidence increased from 4.0 to 6.2/1000 person-years between 2000 and 2009 |
| Japan | Toyama | 1997–2006 | Low coverage (20–30%) | Incidence increased from 3.8 to 4.5/1000 person-years between 1997 and 2006 |
Risk of PHN
The risk of developing PHN varied from 5% to more than 30% (table 3; 49 studies). The estimated risk of PHN varied by study design, age distribution of study populations and definitions used for PHN. For studies that used multiple definitions of PHN, we present results based on the definition of at least 90 days of persistent pain. Studies that reported risk of PHN by age groups consistently found that older patients have a greater risk of developing PHN (see online supplementary table S1). In this review, we found that researchers have used a different duration of persistent pain (persisting for 30, 90 or 180 days) and severity of pain (clinically meaningful pain or any pain) to define PHN. For example, 18% of patients had pain for at least 30 days and 10% for at least 90 days in a population-based study using medical records by Yawn et al3 in the USA. Similarly, 20% of patients had pain for at least 30 days and 14% for at least 90 days in a study by Gauthier et al34 in the UK. Administrative database studies (eg, Ultsch et al42 (4.5%), Opstelten et al43 (2.6%) and Gialloreti et al56 (6.2%)) were more likely to report a lower estimated risk of PHN compared with other studies. Researchers have used diagnosis and medication data in various algorithms, many of which are not validated. It is noteworthy that retrospective studies involving specialists (eg, Mick et al38 (32.5%), Kanbayashi et al102 (52%) and Ro et al103 (39.4%)) may have included existing severe cases of patients with PHN and possibly overestimated the overall risk of PHN.
Table 3.
Risk of PHN in patients with herpes zoster
| Country | Author | Study design | Definition of PHN* | Year | PHN cases | Age | Risk of PHN (%) |
|---|---|---|---|---|---|---|---|
| USA | Ragozzino | Medical records database in Minnesota | Physician diagnosis | 1945–1959 | 55 | All ages | 9.3 |
| USA | Galil | Administrative claims database confirmed by medical records in Massachusetts | Pain persisted for ≥60 days from medical records | 1990–1992 | 68 | All ages | 7.9 |
| USA | Oxman | Zostavax trial in the control | Pain ≥3 score for ≥90 days | 1998–2001 | 80 | ≥60 years | 14.0 |
| USA | Yawn | Retrospective population-based study confirmed by medical records in Minnesota | Pain persisted for ≥90 days from medical records | 1996–2001 | 171 | ≥22 years | 10.0 |
| USA | Thyregod | Prospective cohort study in California | Pain persisted for ≥180 days | 1999–2003 | 30 | ≥50 years | 31.9 |
| USA | Klompas | Administrative claims database confirmed by medical records in Massachusetts | Pain persisted for ≥30 days and required pain medication from medical records | 2008 | 237 | ≥20 years | 12.2 |
| USA | Rimland | Atlanta Veterans Affairs claims database confirmed by medical records | Physician diagnosis from medical charts | 2000–2007 | 205 | All ages | 19.6 |
| USA | Katz | Prospective cohort study in New York | Pain persisted for ≥120 days | NA | 20 | ≥18 years | 19.6 |
| Canada | Drolet | Prospective cohort study, recruited by 83 physicians throughout country | Pain ≥3 score for ≥90 days | 2005–2006 | 56 | ≥50 years | 22.5 |
| UK | Hope-Simpson | Prospective population-based study in Cirencester | Physician diagnosis | 1947–1962 | 46 | All ages | 14.3 |
| UK | Scott | Prospective cohort study | Pain persisted for ≥90 days | NA | 45 | All ages | 27.4 |
| UK | Jung | Prospective cohort study (combined two trials) | Pain persisted for ≥120 days | NA | 114 | ≥15 years | 12.8 |
| UK | Scott | Prospective cohort study in East London | Pain persisted for ≥90 days | NA | 9 | All ages | 13.4 |
| UK | Coen | Prospective cohort study, recruited by GPs | Pain ≥3 score for ≥90 days | 1998–2001 | 24 | All ages | 9.0 |
| UK | Gauthier | GPRD in the UK | Physician diagnosis or pain medication at 90 days from medical records | 2000–2006 | 415 | ≥50 years | 13.7 |
| France | Chidiac | Prospective sentinel surveillance | Physician diagnosis | 1997–1998 | 935 | All ages | 10.3 |
| France | Czernichow | Retrospective population-based survey from GPs | Pain persisted for ≥30 days and required treatment from medical records | 1998 | 111 | All ages | 18.4 |
| France | Mick | Retrospective population-based survey from GPs, dermatologists and neurologists | Pain persisted for ≥90 days from medical records | 2005 | 227 | ≥50 years | 32.5 |
| France | Bouhassira | Prospective cohort study, recruited by GPs | Pain persisted for ≥90 days | 2007–2008 | 127 | ≥50 years | 11.6 |
| Germany | Meister | Retrospective population-based survey from GPs, dermatologists and specialists | Pain persisted for ≥30 days and physician diagnosis | NA | 131 | ≥50 years | 20.6 |
| Germany | Schiffner-Rohe | National Statutory Health Insurance claims database | Pain persisted for ≥90 days and diagnosis or pain medication from ICD-10 | 2004 | NA | ≥50 years | 6.9 |
| Germany | Weinke | Telephone survey of patients, previous HZ diagnosis in 5 years | Pain persisted for ≥90 days | 2008 | 32 | ≥50 years | 11.4 |
| Germany | Ultsch | National Statutory Health Insurance claims database | Pain persisted for ≥90 days and diagnosis or pain medication from ICD-10 | 2004–2009 | 18 160 | All ages | 4.5 |
| The Netherlands | Opstelten | Huisartsen Netwerk Utrecht database in six locations | Pain persisted for ≥90 days and required treatment from medical records | 1994–1999 | 22 | All ages | 2.6 |
| The Netherlands | Opstelten | Prospective cohort study, recruited by GPs (PINE trial) | Pain ≥3 score for ≥90 days | 2001–2004 | 46 | ≥50 years | 7.1 |
| The Netherlands | Pierik | Population-based GPs database in Almere | Physician diagnosis from medical codes | 2004–2008 | 195 | All ages | 5.8 |
| Spain | Cebrian-Cuenca | Prospective cohort study, recruited by 25 GPs in Valencia | Pain persisted for ≥90 days | 2006–2007 | 19 | ≥14 years | 14.5 |
| Spain | Sicras Mainar | Medical records from six primary care and one hospital | Physician diagnosis from medical records | 2007–2010 | 228 | ≥30 years | 15.1 |
| Italy | di Luzio Paparatti | Retrospective population-based survey from GPs | Pain persisted for ≥30 days from medical records | 1995 | 275 | ≥15 years | 19.6 |
| Italy | Volpi | Prospective cohort study, recruited by dermatologists | Pain ≥3 score for ≥180 days | 2001 | 70 | NA | 32.0 |
| Italy | Parruti | Prospective cohort study, recruited from GPs and hospitals in Pescara | Pain persisted for ≥90 days | 2006–2008 | 130 | NA | 30.0 |
| Italy | Gialloreti | National primary care database (Societa Italiana Medici Generici) | Pain persisted for ≥90 days and diagnosis or pain medication from ICD-9 | 2003–2005 | 350 | ≥50 years | 6.2 |
| Italy | Bricout | Prospective cohort study, recruited from GPs | Pain persisted for ≥90 days | 2009–2010 | 85 | ≥50 years | 20.6 |
| Iceland | Helgason | Prospective population-based study | Physician diagnosis at 90 days | 1990–1995 | 28 | All ages | 7.2 |
| 6 European countries | Lukas | Telephone survey, previous 5 years | Pain persisted for ≥90 days | 2008––2009 | 131 | ≥50 years | 13.0 |
| Israel | Weitzman | Maccabi Healthcare Services claims database | ICD-9 code and healthcare service code | 2006–2010 | 1508 | All ages | 5.2 |
| Saudi Arabia | Alakloby | Medical record database from the dermatology clinic | Physician diagnosis | 1988–2006 | 21 | ≥18 years | 14.9 |
| Australia | Stein | National GP database (Bettering the Evaluation of Care and Health) | Physician diagnosis from medical codes | 2000–2006 | 57 | ≥50 years | 15.0 |
| Taiwan | Jih | Taiwan National Health Insurance claims database | Pain persisted for ≥90 days and diagnosis or pain medication from ICD-9 | 2000–2006 | 2944 | All ages | 8.6 |
| Taiwan | Tsai | Prospective cohort study in five centres | Pain ≥3 score for ≥90 days | 2008–2009 | 31 | ≥50 years | 20.7 |
| Japan | Kurokawa | Prospective cohort study in hospitals and clinics in Hyogo | Pain persisted for ≥90 days | NA | 37 | ≥20 years | 26.2 |
| Japan | Kurokawa | Prospective cohort study in hospitals and clinics in Hyogo | Pain persisted for ≥90 days | 2001–2003 | 78 | All ages | 24.7 |
| Japan | Kanbayashi | Retrospective cohort study in pain treatment hospital | Pain persisted for ≥90 days | 2008–2010 | 38 | NA | 52.0 |
| South Korea | Ro | Retrospective, dermatology department hospital | NA | 2007–2011 | 826 | NA | 39.4 |
| South Korea | Song | Prospective cohort study in clinics | Pain ≥3 score for ≥90 days | 2009–2010 | 58 | ≥50 years | 38.4 |
| South Korea | Cho | Prospective cohort study in clinics | Pain ≥3 score for ≥90 days | 2010–2012 | 19 | ≥18 years | 6.2 |
| Thailand | Tunsuriyawong | Retrospective study of medical records at hospital | Physician diagnosis from medical record | 1995–2000 | 67 | All ages | 16.8 |
| Thailand | Aunhachoke | Prospective cohort study, recruited by GPs | Pain persisted for ≥90 days | 2007–2008 | 35 | ≥50 years | 19.4 |
| Singapore | Goh | Prospective cohort study in dermatology clinic | Pain persisted for ≥90 days | 1994–1995 | 46 | All ages | 28.0 |
| India | Chaudhary | NA | NA | NA | 33 | NA | 14.3 |
| India | Abdul Latheef | NA | NA | NA | 21 | All ages | 10.2 |
| Argentina | Vujacich | Medical record database from ID reference centre | Pain persisted for ≥60 days and diagnosis from medical records | 2000–2005 | 39 | All ages | 12.9 |
| Argentina | Vujacich | Prospective cohort study, recruited by GPs | Pain ≥3 score for ≥90 days | NA | 11 | ≥50 years | 11.5 |
*For studies that used multiple definitions of PHN, we present results based on the definition that used at least 90 days of persistent pain.
GP, general practitioner; GPRD, general practice research database; HZ, herpes zoster; ICD, International Classification of Diseases; PHN, postherpetic neuralgia.
We identified six prospective cohort and three cross-sectional studies examining the duration of PHN in North America and Europe (table 4). Several studies reported that PHN may last up to 10 years. Prospective cohort studies demonstrated that approximately 30–50% of patients with PHN experienced pain lasting for more than 1 year. Cross-sectional studies also reported a similar high proportion of patients with PHN; however, these studies are most likely an overestimate because they are more likely to include patients experiencing a longer duration of pain.
Table 4.
Duration of postherpetic neuralgia (sorted by study design)
| Country | Author | Method | Population | Duration of PHN | |
|---|---|---|---|---|---|
| USA | Reda | A prospective cohort study of 8-year follow-up | 14 patients with PHN with a median age of 65 years | Up to 4 years: 14% | |
| Canada | Watson | A prospective cohort study of 11-year follow-up | 156 patients with PHN with a median age of 71 years | 1–11 years: 56% | |
| UK | Hope-Simpson | A prospective cohort study of 26-year follow-up | 46 patients with PHN ≥60 years of age | 1–2 years: 7% | 2–10 years: 22% |
| UK | McKendrick | A prospective cohort study of 9-year follow-up | 158 patients with HZ ≥60 years of age | 21% of patients with HZ had pain for >8 years | |
| Iceland | Helgason | A prospective cohort study of 7-year follow-up | 23 patients with PHN ≥60 years of age | 1–7 years: 35% | >7 years: 17% |
| France | Bouhassira | A prospective cohort study of 1-year follow-up | 127 patients with PHN ≥50 years of age | >1 year: 50% | |
| USA | Oster | A cross-sectional study | 385 patients with PHN with a mean age of 77 years | 1–2 years: 21% | 2 to >10 years: 46% |
| UK | Bowsher | A cross-sectional study | 39 patients with PHN with a mean age of 66 years | 1–2 years: 21% | 2 to >10 years: 33% |
| 6 European countries | van Seventer | A cross-sectional study | 84 patients with PHN with a mean age of 71 years | >1 years: 45% |
HZ, herpes zoster; PHN, postherpetic neuralgia.
Risk of recurrence
A limited number (N=9) of studies examined recurrence of HZ. Four studies reported a risk of <1.5%, with three of these studies conducted over 1–2 years of follow-up.13 57 119 122 About 2.9% of patients had recurrence of HZ in Israel during 2 years of follow-up, while 2.3% of patients had recurrence in South Korea up to 10 years of obervation.60 121 However, studies with a long-term follow-up period tended to report a higher risk of recurrence. Hope-Simpson et al115 reported that 4.7% had recurrence of HZ during 16 years of follow-up in the UK. Similarly, Ragozzino et al12 reported that 5.3% of patients had episodes of recurrence during more than 20 years of follow-up. A recent study by Yawn et al120 also demonstrated that a recurrence of HZ occurred with a rate of 6.2% after 8 years of follow-up. The risk of recurrence may also depend on immune status.120 Thus, overall risk of recurrence may vary by inclusion of those immunocompromised individuals.
Risk of HZO
HZO occurs when VZV reactivation affects the distribution of the ophthalmic division of the trigeminal nerve and can occur with or without eye involvement. Although the number of population-based studies is limited, similar risks of HZO were reported across studies. The reported risks of HZO among patients with HZ were 10.1% (Ragozzino et al,12 USA), 12.3% (Chidiac et al,35 France), 14.4% (Opstelten et al,43 the Netherlands) and 14.9% (Alakloby et al,61 Saudi Arabia). Borkar et al124 reported an overall incidence of 30.9/100 000 person-years, which corresponds to an approximately 10% risk among patients with HZ in the USA. As has been previously recognised, the risk of HZO is similar across age groups.123 124
A wide range of eye complications, such as keratitis, uveitis and conjunctivitis, could result from HZO. The reported risk of these eye complications in patients with HZO ranged widely from approximately 30% to 78%.125–129 In a population-based study in the USA, the risk of HZO with eye involvement among patients with HZ was 2.5%.130 The HZ-associated eye complications required an average of 10 months of medical care with 6% of cases resulting in vision loss.130
Hospitalisation rates associated with HZ
We identified 28 studies that reported HZ-associated hospitalisation (table 5). All studies used hospital discharge or claims data. Rates of HZ-related hospitalisation ranged widely from 2 to 25/100 000 person-years in studies examining all ages. The variation in the estimates may reflect the differing admission criteria in the different settings. Hospitalisations with a primary diagnosis of HZ accounted for about 29–42% of HZ-related hospitalisations.37 62 73 Studies that included hospitalisations with non-primary diagnosis codes (eg, secondary) may have overestimated the hospitalisation rate because they may represent prior or incidental HZ. Hospitalisation rates increased steeply with age, with the majority of the cases occurring in adults ≥50 years of age. For example, Jackson et al73 reported HZ-associated hospitalisation rates (confirmed with medical records) ranging from 10/100 000 in adults 60–69 years of age to 65/100 000 in adults ≥80 years of age in the USA. Similarly, the rate of hospitalisation with primary diagnosis of HZ ranged from 13/100 000 in adults 60–64 years of age to 96/100 000 in adults ≥80 years of age in Australia.62 The rates ranged from 31/100 000 in adults 60–64 years of age to 100/100 000 in adults ≥80 years of age in Germany.41
Table 5.
Hospitalisation rates associated with herpes zoster
| Country | Author | Study design/database | Case ascertainment | Years | Age | Hospitalisation, 100 000 person-years | Older age group |
|---|---|---|---|---|---|---|---|
| USA | Lin | Hospital discharge data in Connecticut | ICD-9 primary or secondary | 1986–1995 | All ages | 16.1 | 144.2 in ≥80 years |
| USA | Coplan | Kaiser Northern California | ICD-9 primary confirmed by medical charts | 1994 | All ages | 2.1 | 9.3 in ≥60 years |
| USA | Patel | National inpatient sample data | ICD-9 any diagnostic position | 1993–2004 | All ages | 25.0 | 112.3 in ≥60 years |
| USA | Jackson | Group Health in Washington medical records | ICD-9 primary confirmed by medical charts | 1992–2004 | ≥50 years | 14.0 | 65.1 in ≥80 years |
| Canada | Brisson | Hospital claims in Manitoba | ICD-9 any diagnostic position | 1979–1997 | All ages | NA | 86.0 in ≥65 years |
| Canada | Edgar | Ministry of health service data in British Columbia | ICD-9/ICD-10 any diagnostic position | 1994–2003 | All ages | 10.0 | 99.0 in ≥80 years |
| Canada | Tanuseputro | Hospital discharge data in Ontario | ICD-9/ICD-10 any diagnostic position | 1992–2010 | All ages | 6.7 | 75.0 in ≥80 years |
| UK | Brisson | Hospitalisation episode statistics in England | ICD-9/ICD-10 any diagnostic position | 1995–1996 | All ages | NA | 148.0 in ≥65 years |
| UK | Brisson | Hospitalisation episode statistics in England | ICD-10 primary diagnosis | 1991–2000 | All ages | 4.4 | 19.1 in ≥60 years |
| France | Gonzalez- Chiappe | National hospital data | ICD-10 primary diagnosis | 2005–2008 | All ages | 4.1 | – |
| Germany | Ultsch | Federal health monitoring system | ICD-10 primary diagnosis | 2007–2008 | ≥50 years | 44.6 | 102.5 in ≥80 years |
| The Netherlands | de Melker | National healthcare registry | ICD-9/ICD-10 primary or secondary | 1998–2001 | All ages | 2.7 | 19.0 in ≥80 years |
| The Netherlands | Pierik | Retrospective population-based study, GPs in Almere | Hospital referrals by GPs | 2004–2008 | All ages | 15.5 | – |
| Belgium | Bilcke | National Christian Sickness Fund | ICD-9 primary or secondary | 2000–2007 | All ages | 14.2 | 85.0 in ≥80 years |
| Spain | Gil | National hospital data | ICD-9 any diagnostic position | 1999–2000 | All ages | 8.4 | – |
| Spain | Gil | National hospital data | ICD-9 primary or secondary | 1998–2004 | ≥30 years | 13.4 | 54.3 in ≥80 years |
| Spain | Bayas | National hospital data in Catalonia | ICD-9 any diagnostic position | 1993–2003 | All ages | 9.7 | – |
| Spain | Morant- Talamante | Electronic medical record database in Valencia | ICD-9 any diagnostic position | 2007–2010 | All ages | 3.0 | 15.7 in ≥80 years |
| Spain | Gil-Prieto | National hospital data | ICD-9 any diagnostic position | 2005–2010 | All ages | 10.3 | – |
| Italy | Di Legami | Hospital discharge records in Piemonte | ICD-9 primary or secondary | 2004 | ≥14 years | 12.0 | 46.0 in ≥80 years |
| Italy | Gialloreti | National hospital discharge records | ICD-9 primary diagnosis | 2003–2005 | All ages | 5.6 | 26.0 in ≥80 years |
| Portugal | Mesquita | National public hospital data | ICD-9 primary diagnosis | 2000–2010 | All ages | 1.9 | – |
| Sweden | Studahl | National patient register | ICD-10 primary diagnosis | 2006–2010 | All ages | 6.9 | – |
| Australia | MacIntyre | National hospital morbidity data | ICD-9/ICD-10 any diagnostic position | 1998–1999 | All ages | 25.0 | 300.0 in ≥80 years |
| Australia | Stein | National hospital morbidity data | ICD-10 primary diagnosis | 1998–2005 | ≥50 years | 28.0 | 95.8 in ≥80 years |
| Australia | Carville | Victoria admitted episode data | ICD-10 primary diagnosis | 2006–2007 | All ages | 9.1 | 89.4 in ≥80 years |
| Taiwan | Jih | National health insurance registry | ICD-9 | 2000–2006 | All ages | 16.1 | 100.0 in ≥80 years |
| Taiwan | Lin | National health insurance registry | ICD-9 | 2000–2005 | All ages | 14.6 | – |
GP, general practitioner; ICD, International Classification of Diseases.
Mortality rates associated with HZ
Mortality rates associated with HZ ranged from 0.017 to 0.465/100 000 person-years in studies (see online supplementary table S2). Most studies reported that the majority of deaths occurred in adults ≥60 years of age.
Discussion
HZ is a significant global health burden that is expected to increase as the population ages. The incidence rises steeply after 50 years of age and many working-age adults and elderly individuals are at increased risk. Risk of complications, particularly debilitating and long-lasting PHN, and hospitalisation is common in the elderly population. The major strength of our study is that we assessed the HZ burden across the globe and comprehensively reviewed incidence, risk of complications, hospitalisation and mortality. Our review included 63 studies on incidence, substantially more than the prior review by Thomas and Hall,9 which included 17 studies with overall incidence ranging from 1.2 to 4.8/1000 person-years. Other reviews were restricted to specific geographic regions and/or assessed only incidence.10 11
Relatively similar estimates of the HZ incidence rate (between 3 and 5/1000 person-years) were reported in North America, Europe and Asia-Pacific. However, we observed some variations in estimates most likely due to the various study designs, case ascertainments, age distributions of the population and year of the study. It is difficult to accurately estimate the incidence rates because it is not a commonly reportable disease and surveillance systems are not usually in place. Most studies had limitations in their study methodology. Almost all studies may be susceptible to under-reporting due to patients who did not seek medical care. However, administrative database studies using diagnostic and billing codes may have overestimated the incidence due to misclassification. Several validation studies reported a relatively high sensitivity for the International Classification of Diseases (ICD)-9 code (98%) and positive predictive value (PPV; 84–94%).15 83 139 Furthermore, studies using administrative insurance data may lack generalisability because they may not be representative of the general population. Population-based surveillance studies face difficulty in estimating the numbers of the population at risk in the study catchment area. Several prospective cohort studies that identified relatively small numbers of patients with HZ (eg, by Scott et al, Paul and Thiel, Di Legami et al and Lionis et al) may have underestimated the rate of HZ due to under-reporting of cases or inaccuracy in estimating the numbers of the population at risk. In spite of these limitations, it is reassuring to find similar incidences across countries in well-conducted studies.
There is a scarcity of research examining the incidence of HZ in Asia, Latin America and Africa. HZ may be regarded as a low health priority in many of these countries; however, the proportion of people ≥60 years of age is projected to double in the next several decades, and the numbers of HZ cases are expected to increase substantially. Further research is needed because it is unclear whether the incidence would be similar in these regions. Age-specific incidence rates may vary because of the regional differences in epidemiology of varicella infection and VZV genotype distribution. Varicella primarily affects young children in temperate countries, whereas varicella tends to occur at a later age during adolescence and adulthood, presenting in severe form with frequent risks of complication and mortality in tropical countries.140 141 Severe varicella infections during adolescence may result in greater numbers of VZVs remaining latent and possibly resulting in earlier reactivation of VZV.142 The distribution of VZV clades varies globally.143 144 VZV can be classified into at least five major clades. VZV clades 1 and 3 are dominant strains in Europe and the Americas, whereas clade 2 is a dominant strain in Asia and clade 5 in Africa.143 Molecular epidemiology of VZV is still an active area of investigation and requires more research. Furthermore, the incidence of HZ may be higher in the countries heavily affected by HIV/AIDS or other immunocompromising conditions.
Hope-Simpson4 hypothesised that exogenous exposure to VZV from individuals with varicella or HZ may boost VZV-specific cell-mediated immunity and thereby decrease the risk of HZ. Because varicella vaccination programmes reduce VZV circulating in the community, thus potentially leading to a decrease in the opportunity for boosting immunity against VZV, it has been hypothesised that the introduction of varicella vaccination might increase the incidence of HZ in the population. However, based on the current literature, there is no conclusive evidence as to whether varicella vaccination programmes have been associated with an increase in the incidence of HZ. In fact, a number of studies across countries have found an increase in the incidence of HZ before introduction of the varicella vaccination programme. It is unclear why the incidence of HZ is increasing. The temporal change or emergence of infectious disease is usually due to changes in the society, technology, virus itself or environment, such as climate change.145 The temporal increase was independent of age. It may partly be explained by an increase in the prevalence of risk factors, an increase in the use of immunosuppressive agents (eg, chemotherapy) or an increase in diagnosis through improved access to healthcare and public awareness. Because HZ is usually clinically diagnosed, diagnostic modalities are unlikely to have affected the reported incidences. Given the steady continuous increase in the incidence of HZ across age groups, it is plausible that a genetic change in the VZV may be playing a role. For example, a study in the UK suggested that changes in genotype distribution have occurred through importation of different strains.146 Although VZV is considered a genetically stable virus, a recombination between different VZV strains could possibly occur.143 147
We reviewed the risk of PHN in patients with HZ. Several long-term prospective cohort studies demonstrated that more than 30% of patients with PHN could experience pain lasting for more than 1 year. The reported risk of developing PHN in patients with HZ varied widely from 5% to more than 30%. The risk of PHN may have differed across countries due to the varying prevalence of disability and other underlying comorbidities in the elderly population.8 148 However, we could not conclude whether the risk of PHN differed by country because of wide variation. The wide variation in the estimates could be partly due to the different study designs used in prior studies. Prospective cohort studies of patients with HZ tend to report greater risk of PHN than studies utilising electronic medical records or administrative databases. We found that administrative database studies often face a numbers of challenges in identifying patients with PHN and they are likely to underestimate the risk of PHN. Currently, there is only one study, by Klompas et al,83 that developed and validated an algorithm for PHN using ICD-9 codes and claims for a filled prescription. The algorithm detected PHN with a sensitivity of 86% and PPV of 78%; however, they defined PHN as a persistent pain for 30 days or more after zoster onset rather than 90 days or more. More validation studies are needed.
Researchers used different definitions of PHN. A difficulty in reaching consensus on a definition for PHN is probably due to a multifactorial pathophysiological nature of the condition and difficulty in objectively assessing the pain.149 Patients with PHN also experience different types of pain including a steady burning pain, a sudden stabbing pain or stimulus-evoked pain (allodynia). The best option for defining PHN would be clinically meaningful pain lasting for more than 90 days after rash onset, considering the pathophysiology and definitions suggested from prior trials on antiviral treatment and zoster vaccination.6 150 151 We also believe that healthcare utilisation patterns and prescribed treatment for PHN vary across countries and that characterising the treatment patterns would be important for future research.
Several prior studies with a long-term follow-up found that recurrence of HZ is frequent, with a rate of 5–6%, which is comparable to rates of first occurrence of HZ. However, a limited number of studies examined the risk of recurrence and more studies are needed to confirm these findings. There were a limited number of population-based studies examining HZO, a severe condition that may lead to significant visual impairment.
Several limitations of this review are worth noting. Because the quality of the study, study design and age distribution of population varied widely across studies, we could not synthesise the data quantitatively to estimate the pooled incidence rates. We did not conduct a formal study quality assessment. However, we described the study design and outcome ascertainment of each study and discussed limitations of studies. Our review focused on general populations, primarily immunocompetent populations, and we did not include studies restricted to immunocompromised populations (such as HIV/AIDS, malignancy or autoimmune disease). Our review also did not include uncommon complications of HZ, such as Ramsay Hunt syndrome, Bell's palsy and transverse myelitis.
In conclusion, similar age-specific incidence of HZ was reported in North America, Europe and Asia-Pacific; however, there is a scarcity of research from other regions. Risk of complications, particularly PHN, and hospitalisation is common in the elderly population. HZ is a global health burden that is expected to increase as the population ages across the world in the near future. The prevalence of disability in the elderly populations is also increasing. It is important for healthcare practitioners and health policymakers to consider implementing effective preventive measures such as vaccination against HZ across the globe.
Supplementary Material
Footnotes
Contributors: KK, BG and CJA designed the study. KK and BG conducted the literature search and extracted data. KK wrote the first draft of the manuscript. KK, BG and CJA interpreted the data, critically revised the manuscript and approved the final version of this manuscript.
Funding: Merck & Co, Inc.
Competing interests: KK is a consultant working for Merck & Co, Inc. BG is a research fellow funded by Merck & Co, Inc. CJA is employed by Merck & Co, Inc.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Cohen JI. Clinical practice: herpes zoster. N Engl J Med 2013;369:255–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dworkin RH, Johnson RW, Breuer J, et al. Recommendations for the management of herpes zoster. Clin Infect Dis 2007;44(Suppl 1):S1–26 [DOI] [PubMed] [Google Scholar]
- 3.Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 2007;82:1341–9 [DOI] [PubMed] [Google Scholar]
- 4.Hope-Simpson RE. The nature of herpes zoster: a long-term study and a new hypothesis. Proc R Soc Med 1965;58:9–20 [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson RW, Bouhassira D, Kassianos G, et al. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med 2010;8:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 2005;352:2271–84 [DOI] [PubMed] [Google Scholar]
- 7.World Population Prospects: The 2012 Revision. United Nations, Department of Economic and Social Affairs, Population Division, 2013
- 8.World report on disability. World Health Organization and the World Bank, 2011
- 9.Thomas SL, Hall AJ. What does epidemiology tell us about risk factors for herpes zoster? Lancet Infect Dis 2004;4:26–33 [DOI] [PubMed] [Google Scholar]
- 10.Araújo LQ, Macintyre CR, Vujacich C. Epidemiology and burden of herpes zoster and post-herpetic neuralgia in Australia, Asia and South America. Herpes 2007;14(Suppl 2):40–4 [PubMed] [Google Scholar]
- 11.Pinchinat S, Cebrián-Cuenca AM, Bricout H, et al. Similar herpes zoster incidence across Europe: results from a systematic literature review. BMC Infect Dis 2013;13:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ragozzino MW, Melton LJ, Kurland LT, et al. Population-based study of herpes zoster and its sequelae. Medicine (Baltimore) 1982;61:310–16 [DOI] [PubMed] [Google Scholar]
- 13.Donahue JG, Choo PW, Manson JE, et al. The incidence of herpes zoster. Arch Intern Med 1995;155:1605–9 [PubMed] [Google Scholar]
- 14.Insinga RP, Itzler RF, Pellissier JM, et al. The incidence of herpes zoster in a United States administrative database. J Gen Intern Med 2005;20:748–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mullooly JP, Riedlinger K, Chun C, et al. Incidence of herpes zoster, 1997–2002. Epidemiol Infect 2005;133:245–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yih WK, Brooks DR, Lett SM, et al. The incidence of varicella and herpes zoster in Massachusetts as measured by the Behavioral Risk Factor Surveillance System (BRFSS) during a period of increasing varicella vaccine coverage, 1998–2003. BMC Public Health 2005;5:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jumaan AO, Yu O, Jackson LA, et al. Incidence of herpes zoster, before and after varicella-vaccination-associated decreases in the incidence of varicella, 1992–2002. J Infect Dis 2005;191:2002–7 [DOI] [PubMed] [Google Scholar]
- 18.Rimland D, Moanna A. Increasing incidence of herpes zoster among veterans. Clin Infect Dis 2010;50:1000–5 [DOI] [PubMed] [Google Scholar]
- 19.Leung J, Harpaz R, Molinari NA, et al. Herpes zoster incidence among insured persons in the United States, 1993–2006: evaluation of impact of varicella vaccination. Clin Infect Dis 2011;52:332–40 [DOI] [PubMed] [Google Scholar]
- 20.Tseng HF, Smith N, Harpaz R, et al. Herpes zoster vaccine in older adults and the risk of subsequent herpes zoster disease. JAMA 2011;305:160–6 [DOI] [PubMed] [Google Scholar]
- 21.Langan SM, Smeeth L, Margolis DJ, et al. Herpes zoster vaccine effectiveness against incident herpes zoster and post-herpetic neuralgia in an older US population: a cohort study. PLoS Med 2013;10:e1001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen SY, Suaya JA, Li Q, et al. Incidence of herpes zoster in patients with altered immune function. Infection 2014;42:325–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hales CM, Harpaz R, Joesoef MR, et al. Examination of links between herpes zoster incidence and childhood varicella vaccination. Ann Intern Med 2013;159:739–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brisson M, Edmunds WJ, Law B, et al. Epidemiology of varicella zoster virus infection in Canada and the United Kingdom. Epidemiol Infect 2001;127:305–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Russell ML, Schopflocher DP, Svenson L, et al. Secular trends in the epidemiology of shingles in Alberta. Epidemiol Infect 2007;135:908–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edgar BL, Galanis E, Kay C, et al. The burden of varicella and zoster in British Columbia 1994–2003: baseline assessment prior to universal vaccination. Can Commun Dis Rep 2007;33: 1–15 [PubMed] [Google Scholar]
- 27.Tanuseputro P, Zagorski B, Chan KJ, et al. Population-based incidence of herpes zoster after introduction of a publicly funded varicella vaccination program. Vaccine 2011;29:8580–4 [DOI] [PubMed] [Google Scholar]
- 28.Russell ML, Dover DC, Simmonds KA, et al. Shingles in Alberta: before and after publicly funded varicella vaccination. Vaccine 2013. 10.1016/j.vaccine.2013.09.018. [Epub ahead of print 4 Oct 2013]. [DOI] [PubMed] [Google Scholar]
- 29.Ross CA, Brown WK, Clarke A, et al. Herpes zoster in general practice. J R Coll Gen Pract 1975;25:29–32 [PMC free article] [PubMed] [Google Scholar]
- 30.Brisson M, Edmunds WJ. Epidemiology of varicella-zoster virus in England and Wales. J Med Virol 2003;70(Suppl 1):S9–14 [DOI] [PubMed] [Google Scholar]
- 31.Fleming DM, Cross KW, Cobb WA, et al. Gender difference in the incidence of shingles. Epidemiol Infect 2004;132:1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chapman RS, Cross KW, Fleming DM. The incidence of shingles and its implications for vaccination policy. Vaccine 2003;21: 2541–7 [DOI] [PubMed] [Google Scholar]
- 33.Scott FT, Leedham-Green ME, Barrett-Muir WY, et al. A study of shingles and the development of postherpetic neuralgia in East London. J Med Virol 2003;70(Suppl 1):S24–30 [DOI] [PubMed] [Google Scholar]
- 34.Gauthier A, Breuer J, Carrington D, et al. Epidemiology and cost of herpes zoster and post-herpetic neuralgia in the United Kingdom. Epidemiol Infect 2009;137:38–47 [DOI] [PubMed] [Google Scholar]
- 35.Chidiac C, Bruxelle J, Daures JP, et al. Characteristics of patients with herpes zoster on presentation to practitioners in France. Clin Infect Dis 2001;33:62–9 [DOI] [PubMed] [Google Scholar]
- 36.Czernichow S, Dupuy A, Flahault A, et al. [Herpes zoster: incidence study among “sentinel” general practitioners]. Ann Dermatol Venereol 2001;128:497–501 [PubMed] [Google Scholar]
- 37.Gonzalez Chiappe S, Sarazin M, Turbelin C, et al. Herpes zoster: burden of disease in France. Vaccine 2010;28:7933–8 [DOI] [PubMed] [Google Scholar]
- 38.Mick G, Gallais JL, Simon F, et al. [Burden of herpes zoster and postherpetic neuralgia: incidence, proportion, and associated costs in the French population aged 50 or over]. Rev Epidemiol Sante Publique 2010;58:393–401 [DOI] [PubMed] [Google Scholar]
- 39.Paul E, Thiel T. [Epidemiology of varicella zoster infection. Results of a prospective study in the Ansbach area]. Hautarzt 1996;47:604–9 [DOI] [PubMed] [Google Scholar]
- 40.Schiffner-Rohe J, Jow S, Lilie HM, et al. [Herpes zoster in Germany. A retrospective analyse of SHL data] MMW Fortschr Med 2010;151(Suppl 4):193–7 [PubMed] [Google Scholar]
- 41.Ultsch B, Siedler A, Rieck T, et al. Herpes zoster in Germany: quantifying the burden of disease. BMC Infect Dis 2011;11:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ultsch B, Köster I, Reinhold T, et al. Epidemiology and cost of herpes zoster and postherpetic neuralgia in Germany. Eur J Health Econ 2013;14:1015–26 [DOI] [PubMed] [Google Scholar]
- 43.Opstelten W, Mauritz JW, de Wit NJ, et al. Herpes zoster and postherpetic neuralgia: incidence and risk indicators using a general practice research database. Fam Pract 2002;19:471–5 [DOI] [PubMed] [Google Scholar]
- 44.de Melker H, Berbers G, Hahné S, et al. The epidemiology of varicella and herpes zoster in the Netherlands: implications for varicella zoster virus vaccination. Vaccine 2006;24:3946–52 [DOI] [PubMed] [Google Scholar]
- 45.Opstelten W, Van Essen GA, Schellevis F, et al. Gender as an independent risk factor for herpes zoster: a population-based prospective study. Ann Epidemiol 2006;16:692–5 [DOI] [PubMed] [Google Scholar]
- 46.Pierik JG, Gumbs PD, Fortanier SA, et al. Epidemiological characteristics and societal burden of varicella zoster virus in the Netherlands. BMC Infect Dis 2012;12:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richard J-L, Zimmermann H. Herpès zoster 1998–2001. Sentinella-Jahresbericht; 2001
- 48.Bilcke J, Ogunjimi B, Marais C, et al. The health and economic burden of chickenpox and herpes zoster in Belgium. Epidemiol Infect 2012;140:2096–109 [DOI] [PubMed] [Google Scholar]
- 49.Pérez-Farinós N, Ordobás M, García-Fernández C, et al. Varicella and herpes zoster in Madrid, based on the Sentinel General Practitioner Network: 1997–2004. BMC Infect Dis 2007;7:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.García Cenoz M, Castilla J, Montes Y, et al. [Varicella and herpes zoster incidence prior to the introduction of systematic child vaccination in Navarre, 2005–2006]. An Sist Sanit Navar 2008;31:71–80 [DOI] [PubMed] [Google Scholar]
- 51.Cebrián-Cuenca AM, Díez-Domingo J, Rodríguez MS, et al. Epidemiology of herpes zoster infection among patients treated in primary care centres in the Valencian community (Spain). BMC Fam Pract 2010;11:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morant-Talamante N, Diez-Domingo J, Martínez-Úbeda S, et al. Herpes zoster surveillance using electronic databases in the Valencian community (Spain). BMC Infect Dis 2013;13:463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Esteban-Vasallo MD, Gil-Prieto R, Domínguez-Berjón MF, et al. Temporal trends in incidence rates of herpes zoster among patients treated in primary care centers in Madrid (Spain), 2005–2012. J Infect 2014;68:378–86 [DOI] [PubMed] [Google Scholar]
- 54.di Luzio Paparatti U, Arpinelli F, Visonà G. Herpes zoster and its complications in Italy: an observational survey. J Infect 1999;38:116–20 [DOI] [PubMed] [Google Scholar]
- 55.Di Legami V, Gianino MM, Ciofi degli Atti M, et al. Epidemiology and costs of herpes zoster: background data to estimate the impact of vaccination. Vaccine 2007;25:7598–604 [DOI] [PubMed] [Google Scholar]
- 56.Gialloreti LE, Merito M, Pezzotti P, et al. Epidemiology and economic burden of herpes zoster and post-herpetic neuralgia in Italy: a retrospective, population-based study. BMC Infect Dis 2010;10:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Helgason S, Sigurdsson J, Gudmundsson S. The clinical course of herpes zoster: a prospective study in primary care. Eur J Gen Pract 1996;2:12–16 [Google Scholar]
- 58.Studahl M, Petzold M, Cassel T. Disease burden of herpes zoster in Sweden—predominance in the elderly and in women—a register based study. BMC Infect Dis 2013;13:586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lionis CD, Vardavas CI, Symvoulakis EK, et al. Measuring the burden of herpes zoster and post herpetic neuralgia within primary care in rural Crete, Greece. BMC Fam Pract 2011;12:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weitzman D, Shavit O, Stein M, et al. A population based study of the epidemiology of Herpes Zoster and its complications. J Infect 2013;67:463–9 [DOI] [PubMed] [Google Scholar]
- 61.Alakloby OM, AlJabre SH, Randhawa MA, et al. Herpes zoster in eastern Saudi Arabia: clinical presentation and management. J Drugs Dermatol 2008;7:457–62 [PubMed] [Google Scholar]
- 62.Stein AN, Britt H, Harrison C, et al. Herpes zoster burden of illness and health care resource utilisation in the Australian population aged 50 years and older. Vaccine 2009;27:520–9 [DOI] [PubMed] [Google Scholar]
- 63.Jih JS, Chen YJ, Lin MW, et al. Epidemiological features and costs of herpes zoster in Taiwan: a national study 2000 to 2006. Acta Derm Venereol 2009;89:612–16 [DOI] [PubMed] [Google Scholar]
- 64.Lin YH, Huang LM, Chang IS, et al. Disease burden and epidemiology of herpes zoster in pre-vaccine Taiwan. Vaccine 2010;28:1217–20 [DOI] [PubMed] [Google Scholar]
- 65.Chao DY, Chien YZ, Yeh YP, et al. The incidence of varicella and herpes zoster in Taiwan during a period of increasing varicella vaccine coverage, 2000–2008. Epidemiol Infect 2012;140: 1131–40 [DOI] [PubMed] [Google Scholar]
- 66.Park S, Kim J, Kim C, et al. A clinical study on herpes zoster during the last 10-year-period (1994–2003). Korean J Dermatol 2004;42:1531–5 [Google Scholar]
- 67.Choi WS, Noh JY, Huh JY, et al. Disease burden of herpes zoster in Korea. J Clin Virol 2010;47:325–9 [DOI] [PubMed] [Google Scholar]
- 68.Toyama N, Shiraki K; Society of the Miyazaki Prefecture Dermatologists. Epidemiology of herpes zoster and its relationship to varicella in Japan: a 10-year survey of 48,388 herpes zoster cases in Miyazaki prefecture. J Med Virol 2009;81:2053–8 [DOI] [PubMed] [Google Scholar]
- 69.Vujacich C, Poggi E, Cecchini D, et al. [Clinical and epidemiological aspects of herpes zoster]. Medicina (B Aires) 2008;68:125–8 [PubMed] [Google Scholar]
- 70.Castro L, Chen S. Zoster: mais frequentes entre jovens que entre idosos/zoster: is more frequent among youngers than aged. An Bras Dermatol 1990;65:129–33 [Google Scholar]
- 71.Gaitan M. Herpes zoster y cancer: relaciones entre estas dos enfermedades/herpes zoster and cancer: relationship between these 2 diseases. Acta Med Colomb 1981;6:287–93 [Google Scholar]
- 72.Patel MS, Gebremariam A, Davis MM. Herpes zoster-related hospitalizations and expenditures before and after introduction of the varicella vaccine in the United States. Infect Control Hosp Epidemiol 2008;29:1157–63 [DOI] [PubMed] [Google Scholar]
- 73.Jackson LA, Reynolds MA, Harpaz R. Hospitalizations to treat herpes zoster in older adults: causes and validated rates. Clin Infect Dis 2008;47:754–9 [DOI] [PubMed] [Google Scholar]
- 74.Civen R, Chaves SS, Jumaan A, et al. The incidence and clinical characteristics of herpes zoster among children and adolescents after implementation of varicella vaccination. Pediatr Infect Dis J 2009;28:954–9 [DOI] [PubMed] [Google Scholar]
- 75.Yawn B, Wollan P, Bialek S, et al. Trends in herpes zoster prevalence in a population based cohort from 1945 to 2008. 48th Annual Meeting of the Infectious Diseases Society of America 2010 [Google Scholar]
- 76.MacIntyre CR, Chu CP, Burgess MA. Use of hospitalization and pharmaceutical prescribing data to compare the prevaccination burden of varicella and herpes zoster in Australia. Epidemiol Infect 2003;131:675–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Carville KS, Riddell MA, Kelly HA. A decline in varicella but an uncertain impact on zoster following varicella vaccination in Victoria, Australia. Vaccine 2010;28:2532–8 [DOI] [PubMed] [Google Scholar]
- 78.Nelson MR, Britt HC, Harrison CM. Evidence of increasing frequency of herpes zoster management in Australian general practice since the introduction of a varicella vaccine. Med J Aust 2010;193:110–13 [PubMed] [Google Scholar]
- 79.Jardine A, Conaty SJ, Vally H. Herpes zoster in Australia: evidence of increase in incidence in adults attributable to varicella immunization? Epidemiol Infect 2011;139:658–65 [DOI] [PubMed] [Google Scholar]
- 80.Wu PY, Wu HD, Chou TC, et al. Varicella vaccination alters the chronological trends of herpes zoster and varicella. PLoS ONE 2013;8:e77709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Galil K, Choo PW, Donahue JG, et al. The sequelae of herpes zoster. Arch Intern Med 1997;157:1209–13 [PubMed] [Google Scholar]
- 82.Thyregod HG, Rowbotham MC, Peters M, et al. Natural history of pain following herpes zoster. Pain 2007;128:148–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Klompas M, Kulldorff M, Vilk Y, et al. Herpes zoster and postherpetic neuralgia surveillance using structured electronic data. Mayo Clin Proc 2011;86:1146–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Katz J, McDermott MP, Cooper EM, et al. Psychosocial risk factors for postherpetic neuralgia: a prospective study of patients with herpes zoster. J Pain 2005;6:782–90 [DOI] [PubMed] [Google Scholar]
- 85.Drolet M, Brisson M, Schmader K, et al. Predictors of postherpetic neuralgia among patients with herpes zoster: a prospective study. J Pain 2010;11:1211–21 [DOI] [PubMed] [Google Scholar]
- 86.Jung BF, Johnson RW, Griffin DR, et al. Risk factors for postherpetic neuralgia in patients with herpes zoster. Neurology 2004;62:1545–51 [DOI] [PubMed] [Google Scholar]
- 87.Coen PG, Scott F, Leedham-Green M, et al. Predicting and preventing post-herpetic neuralgia: are current risk factors useful in clinical practice? Eur J Pain 2006;10:695–700 [DOI] [PubMed] [Google Scholar]
- 88.Bouhassira D, Chassany O, Gaillat J, et al. Patient perspective on herpes zoster and its complications: an observational prospective study in patients aged over 50 years in general practice. Pain 2012;153:342–9 [DOI] [PubMed] [Google Scholar]
- 89.Meister W, Neiss A, Gross G, et al. A prognostic score for postherpetic neuralgia in ambulatory patients. Infection 1998;26:359–63 [DOI] [PubMed] [Google Scholar]
- 90.Weinke T, Edte A, Schmitt S, et al. Impact of herpes zoster and post-herpetic neuralgia on patients’ quality of life: a patient-reported outcomes survey. Z Gesundh Wiss 2010;18:367–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Opstelten W, Zuithoff NP, van Essen GA, et al. Predicting postherpetic neuralgia in elderly primary care patients with herpes zoster: prospective prognostic study. Pain 2007;132(Suppl 1):S52–9 [DOI] [PubMed] [Google Scholar]
- 92.Sicras-Mainar A, Navarro-Artieda R, Ibáñez-Nolla J, et al. [Incidence, resource use and costs associated with postherpetic neuralgia: a population-based retrospective study]. Rev Neurol 2012;55:449–61 [PubMed] [Google Scholar]
- 93.Cebrián-Cuenca AM, Díez-Domingo J, San-Martín-Rodríguez M, et al. Epidemiology and cost of herpes zoster and postherpetic neuralgia among patients treated in primary care centres in the Valencian community of Spain. BMC Infect Dis 2011;11:302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Volpi A, Gatti A, Pica F, et al. Clinical and psychosocial correlates of post-herpetic neuralgia. J Med Virol 2008;80:1646–52 [DOI] [PubMed] [Google Scholar]
- 95.Parruti G, Tontodonati M, Rebuzzi C, et al. Predictors of pain intensity and persistence in a prospective Italian cohort of patients with herpes zoster: relevance of smoking, trauma and antiviral therapy. BMC Med 2010;8:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bricout H, Perinetti E, Marchettini P, et al. Predictor factors for the presence of post herpetic neuralgia at 3 months in herpes zoster patients aged 50 and over in Italy: results from a gp-based observational prospective multicenter study. Value Health 2013;16:A343 [Google Scholar]
- 97.Helgason S, Petursson G, Gudmundsson S, et al. Prevalence of postherpetic neuralgia after a first episode of herpes zoster: prospective study with long term follow up. BMJ 2000;321:794–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lukas K, Edte A, Bertrand I. The impact of herpes zoster and post-herpetic neuralgia on quality of life: patient-reported outcomes in six European countries. J Public Health(Germany) 2012;20:441–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tsai TF, Yu HS, Rampakakis E, et al. Assessment of burden of illness due to herpes zoster and predictors of outcomes in Taiwan: a prospective observational study. Int J Infect Dis 2012;16:e115 [Google Scholar]
- 100.Kurokawa I, Kumano K, Murakawa K, et al. Clinical correlates of prolonged pain in Japanese patients with acute herpes zoster. J Int Med Res 2002;30:56–65 [DOI] [PubMed] [Google Scholar]
- 101.Kurokawa I, Murakawa K, Kumano K. The change in zoster-associated pain treated with oral valaciclovir in immunocompetent patients with acute herpes zoster. Int J Clin Pract 2007;61:1223–9 [DOI] [PubMed] [Google Scholar]
- 102.Kanbayashi Y, Onishi K, Fukazawa K, et al. Predictive factors for postherpetic neuralgia using ordered logistic regression analysis. Clin J Pain 2012;28:712–14 [DOI] [PubMed] [Google Scholar]
- 103.Ro BI, Go JW, Kim SH, et al. A clinical study on 2096 patients with herpes zoster during the four-year-period (2007–2011). J Dermatol 2012;39:10 [Google Scholar]
- 104.Song HJ, Choi WS, Lee JD, et al. Measuring herpes zoster and post-herpetic neuralgia associated burden of illness and health care utilization and costs in Korea: a clinical epidemiological study. Int J Infect Dis 2012;16:e111 [Google Scholar]
- 105.Cho SI, Lee CH, Park GH, et al. Use of S-LANSS, a tool for screening neuropathic pain, for predicting postherpetic neuralgia in patients after acute herpes zoster events: a single-center, 12-month, prospective cohort study. J Pain 2014;15:149–56 [DOI] [PubMed] [Google Scholar]
- 106.Tunsuriyawong S, Puavilai S. Herpes zoster, clinical course and associated diseases: a 5-year retrospective study at Tamathibodi Hospital. J Med Assoc Thai 2005;88:678–81 [PubMed] [Google Scholar]
- 107.Aunhachoke K, Bussaratid V, Chirachanakul P, et al. Measuring herpes zoster, zoster-associated pain, post-herpetic neuralgia-associated loss of quality of life, and healthcare utilization and costs in Thailand. Int J Dermatol 2011;50:428–35 [DOI] [PubMed] [Google Scholar]
- 108.Goh CL, Khoo L. A retrospective study of the clinical presentation and outcome of herpes zoster in a tertiary dermatology outpatient referral clinic. Int J Dermatol 1997;36:667–72 [DOI] [PubMed] [Google Scholar]
- 109.Chaudhary SD, Dashore A, Pahwa US. A clinico-epidemiologic profile of herpes zoster in North India. Indian J Dermatol Venereol Leprol 1987;53:213–16 [PubMed] [Google Scholar]
- 110.Abdul Latheef EN, Pavithran K. Herpes zoster: a clinical study in 205 patients. Indian J Dermatol 2011;56:529–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Vujacich C, De Wouters L, Margari A, et al. Assessment of burden of illness due to herpes zoster in Argentina: a prospective observational study. Value Health 2013;16:A668 [Google Scholar]
- 112.Oster G, Harding G, Dukes E, et al. Pain, medication use, and health-related quality of life in older persons with postherpetic neuralgia: results from a population-based survey. J Pain 2005;6:356–63 [DOI] [PubMed] [Google Scholar]
- 113.Reda H, Greene K, Rice FL, et al. Natural history of herpes zoster: late follow-up of 3.9 years (n=43) and 7.7 years (n=10). Pain 2013;154:2227–33 [DOI] [PubMed] [Google Scholar]
- 114.Watson CP, Oaklander AL. Postherpetic neuralgia. Pain Pract 2002;2:295–307 [DOI] [PubMed] [Google Scholar]
- 115.Hope-Simpson RE. Postherpetic neuralgia. J R Coll Gen Pract 1975;25:571–5 [PMC free article] [PubMed] [Google Scholar]
- 116.Bowsher D. The lifetime occurrence of herpes zoster and prevalence of post-herpetic neuralgia: a retrospective survey in an elderly population. Eur J Pain 1999;3:335–42 [DOI] [PubMed] [Google Scholar]
- 117.McKendrick MW, Ogan P, Care CC. A 9 year follow up of post herpetic neuralgia and predisposing factors in elderly patients following herpes zoster. J Infect 2009;59:416–20 [DOI] [PubMed] [Google Scholar]
- 118.van Seventer R, Sadosky A, Lucero M, et al. A cross-sectional survey of health state impairment and treatment patterns in patients with postherpetic neuralgia. Age Ageing 2006;35:132–7 [DOI] [PubMed] [Google Scholar]
- 119.Epstein E. Recurrences in herpes zoster. Cutis 1980;26: 378–9 [PubMed] [Google Scholar]
- 120.Yawn BP, Wollan PC, Kurland MJ, et al. Herpes zoster recurrences more frequent than previously reported. Mayo Clin Proc 2011;86:88–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jeong S, Kim I. Recurrence rate of herpes zoster during the previous decade. Korean J Dermatol 2012;50:287–9 [Google Scholar]
- 122.Tseng HF, Chi M, Smith N, et al. Herpes zoster vaccine and the incidence of recurrent herpes zoster in an immunocompetent elderly population. J Infect Dis 2012;206:190–6 [DOI] [PubMed] [Google Scholar]
- 123.Ghaznawi N, Virdi A, Dayan A, et al. Herpes zoster ophthalmicus: comparison of disease in patients 60 years and older versus younger than 60 years. Ophthalmology 2011;118:2242–50 [DOI] [PubMed] [Google Scholar]
- 124.Borkar DS, Tham VM, Esterberg E, et al. Incidence of herpes zoster ophthalmicus: results from the pacific ocular inflammation study. Ophthalmology 2013;120:451–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bayu S, Alemayehu W. Clinical profile of herpes zoster ophthalmicus in Ethiopians. Clin Infect Dis 1997;24:1256–60 [DOI] [PubMed] [Google Scholar]
- 126.Liesegang TJ. Herpes zoster ophthalmicus natural history, risk factors, clinical presentation, and morbidity. Ophthalmology 2008;115(Suppl 2):S3–12 [DOI] [PubMed] [Google Scholar]
- 127.Zaal MJ, Völker-Dieben HJ, D'Amaro J. Visual prognosis in immunocompetent patients with herpes zoster ophthalmicus. Acta Ophthalmol Scand 2003;81:216–20 [DOI] [PubMed] [Google Scholar]
- 128.Womack LW, Liesegang TJ. Complications of herpes zoster ophthalmicus. Arch Ophthalmol 1983;101:42–5 [DOI] [PubMed] [Google Scholar]
- 129.Harding SP, Lipton JR, Wells JC. Natural history of herpes zoster ophthalmicus: predictors of postherpetic neuralgia and ocular involvement. Br J Ophthalmol 1987;71:353–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yawn BP, Wollan PC, St Sauver JL, et al. Herpes zoster eye complications: rates and trends. Mayo Clin Proc 2013;88: 562–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lin F, Hadler JL. Epidemiology of primary varicella and herpes zoster hospitalizations: the pre-varicella vaccine era. J Infect Dis 2000;181:1897–905 [DOI] [PubMed] [Google Scholar]
- 132.Coplan P, Black S, Rojas C, et al. Incidence and hospitalization rates of varicella and herpes zoster before varicella vaccine introduction: a baseline assessment of the shifting epidemiology of varicella disease. Pediatr Infect Dis J 2001;20:641–5 [DOI] [PubMed] [Google Scholar]
- 133.Gil A, San-Martín M, Carrasco P, et al. Epidemiology of severe varicella-zoster virus infection in Spain. Vaccine 2004;22: 3947–51 [DOI] [PubMed] [Google Scholar]
- 134.Gil A, Gil R, Alvaro A, et al. Burden of herpes zoster requiring hospitalization in Spain during a seven-year period (1998–2004). BMC Infect Dis 2009;9:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Bayas JM, Gil R, Llupia A, et al. Hospitalizations due to herpes zoster and postherpetic neuralgia in Catalonia, 1998–2003. Vacunas 2011;12:122–8 [Google Scholar]
- 136.Gil-Prieto R, Walter S, Gonzalez-Escalada A, et al. Different vaccination strategies in Spain and its impact on severe varicella and zoster. Vaccine 2014;32:277–83 [DOI] [PubMed] [Google Scholar]
- 137.Mesquita M, Froes F. Hospital admissions for herpes zoster in Portugal between 2000 and 2010. Acta Med Port 2013;26:531–6 [PubMed] [Google Scholar]
- 138.Mahamud A, Marin M, Nickell SP, et al. Herpes zoster-related deaths in the United States: validity of death certificates and mortality rates, 1979–2007. Clin Infect Dis 2012;55:960–6 [DOI] [PubMed] [Google Scholar]
- 139.Yawn BP, Wollan P, St Sauver J. Comparing shingles incidence and complication rates from medical record review and administrative database estimates: how close are they? Am J Epidemiol 2011;174:1054–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lee BW. Review of varicella zoster seroepidemiology in India and Southeast Asia. Trop Med Int Health 1998;3:886–90 [DOI] [PubMed] [Google Scholar]
- 141.Vergara-Castañeda A, Escobar-Gutiérrez A, Ruiz-Tovar K, et al. Epidemiology of varicella in Mexico. J Clin Virol 2012;55:51–7 [DOI] [PubMed] [Google Scholar]
- 142.Nagasako EM, Johnson RW, Griffin DR, et al. Geographic and racial aspects of herpes zoster. J Med Virol 2003;70(Suppl 1):S20–3 [DOI] [PubMed] [Google Scholar]
- 143.Schmidt-Chanasit J, Sauerbrei A. Evolution and world-wide distribution of varicella-zoster virus clades. Infect Genet Evol 2011;11:1–10 [DOI] [PubMed] [Google Scholar]
- 144.Loparev VN, Gonzalez A, Deleon-Carnes M, et al. Global identification of three major genotypes of varicella-zoster virus: longitudinal clustering and strategies for genotyping. J Virol 2004;78:8349–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Morse SS. Factors in the emergence of infectious diseases. Emerg Infect Dis 1995;1:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sengupta N, Taha Y, Scott FT, et al. Varicella-zoster-virus genotypes in East London: a prospective study in patients with herpes zoster. J Infect Dis 2007;196:1014–20 [DOI] [PubMed] [Google Scholar]
- 147.Sauerbrei A, Wutzler P. Different genotype pattern of varicella-zoster virus obtained from patients with varicella and zoster in Germany. J Med Virol 2007;79:1025–31 [DOI] [PubMed] [Google Scholar]
- 148.Wahrendorf M, Reinhardt JD, Siegrist J. Relationships of disability with age among adults aged 50 to 85: evidence from the United States, England and continental Europe. PLoS ONE 2013;8:e71893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Johnson RW, Wasner G, Saddier P, et al. Postherpetic neuralgia: epidemiology, pathophysiology and management. Expert Rev Neurother 2007;7:1581–95 [DOI] [PubMed] [Google Scholar]
- 150.Dworkin RH, Carrington D, Cunningham A, et al. Assessment of pain in herpes zoster: lessons learned from antiviral trials. Antiviral Res 1997;33:73–85 [DOI] [PubMed] [Google Scholar]
- 151.Coplan PM, Schmader K, Nikas A, et al. Development of a measure of the burden of pain due to herpes zoster and postherpetic neuralgia for prevention trials: adaptation of the brief pain inventory. J Pain 2004;5:344–56 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.