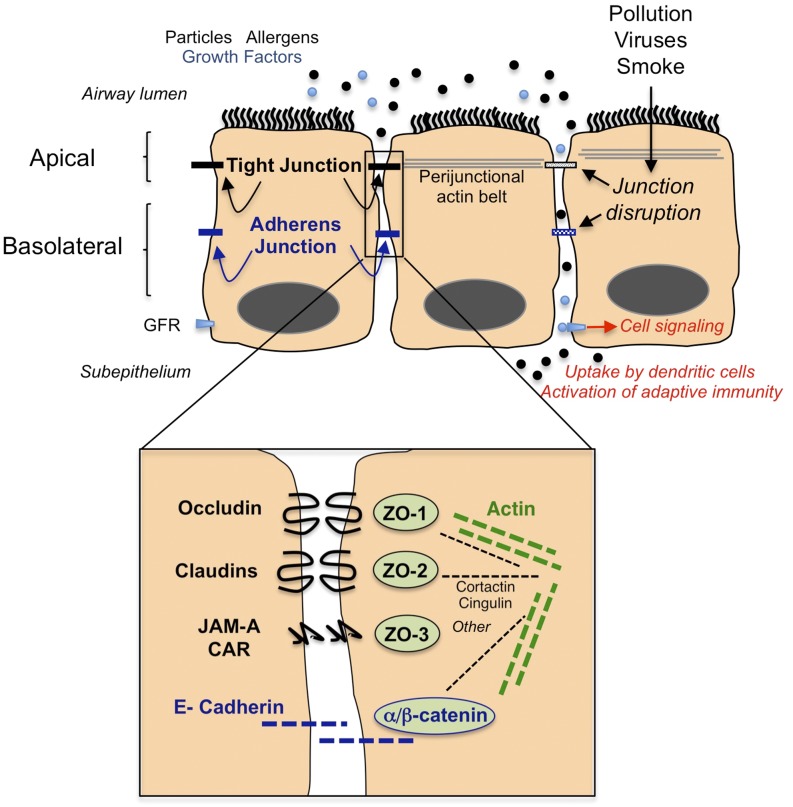
Figure 1.
Cartoon diagram demonstrating organization of junctional structures in the airway epithelium including tight junctions (black) and adherens junctions (blue). Certain environmental exposures lead to dysfunction of epithelial junction, resulting in greater outside/in permeability. The figure demonstrates the potential for barrier dysfunction to lead to cell signaling because it allows apical cytokines and growth factors, which may be constitutively present in epithelial lining fluids (light blue dots), to interact with basolateral receptors (light blue rectangle labeled GFR [growth factor receptor]). In the presence of intact epithelial junctions, these ligand/receptor interactions are prevented. Barrier dysfunction also allows penetration of luminal particles and antigens into the subepithelial space, where they encounter innate immune cells that initiate inflammation and immune reactions. The fate of subepithelial particles is complex; subepithelial particles may, depending on size and shape, translocate via afferent lymphatics to the pleural space, regional lymph nodes, or the blood stream (not shown). The inset shows an enlarged schematic of protein–protein interactions in tight junctions (black text) and adherens junctions (blue text), including ability of zonula occludens (ZO) proteins to interact with intracytoplasmic domains. The inset also indicates that junctional proteins are linked to the actin cytoskeleton (green dashed line) via several potential adaptor proteins (black dashed line). This figure is meant to be illustrative and not comprehensive and does not include many other potential interacting partners or other molecules that contribute to barrier integrity or cell polarity. CAR, coxsackie adenovirus receptor; JAM-A, junctional adhesion molecule.