Abstract
Literature on neighborhood effects on health largely employs non-experimental study designs and does not typically test specific neighborhood mediators that influence health. We address these gaps using the Moving to Opportunity (MTO) housing voucher experiment. Research has documented both beneficial and adverse effects on health in MTO, but mediating mechanisms have not been tested explicitly. We tested mediation of MTO effects on youth asthma (n = 2829). MTO randomized families living in public housing to an experimental group receiving a voucher to subsidize rental housing, or a control group receiving no voucher, and measured outcomes 4–7 years following randomization. MTO had a harmful main effect vs. controls for self-reported asthma diagnosis (b = 0.24, p = 0.06), past-year asthma attack (b = 0.44, p = 0.02), and past-year wheezing (b = 0.17, p = 0.17). Using Inverse Odds Weighting mediation we tested mental health, smoking, and four housing dimensions as potential mediators of the MTO–asthma relationship. We found no significant mediation overall, but mediation may be gender-specific. Gender-stratified models displayed countervailing mediation effects among girls for asthma diagnosis by smoking (p = 0.05) and adult-reported housing quality (p = 0.06), which reduced total effects by 35% and 42% respectively. MTO treatment worsened boys’ mental health and mental health reduced treatment effects on asthma diagnosis by 27%. Future research should explore other potential mediators and gender-specific mediators of MTO effects on asthma. Improving measurement of housing conditions and other potential mediators may help elucidate the “black box” of neighborhood effects.
Keywords: Asthma, Mediation, Housing mobility, Neighborhood, Housing
1. Introduction
Asthma is one of the most common childhood ailments in the US, with 14% lifetime prevalence among children aged 0–17 in 2011 (CDC, 2011), and even higher prevalence among African American and low-income, urban populations (Akinbami et al., 2012). The Moving to Opportunity (MTO) program provides a unique opportunity to examine housing-related causes and mediators of asthma within an experimental design, among this population that is disproportionately affected. The MTO study randomized low-income families to receive a housing voucher to subsidize a private rental apartment and move out of public housing, thereby improving their neighborhood and housing environment compared to controls (Orr et al., 2003), which presumably should have reduced asthma. Although prior work has documented both beneficial and harmful effects of MTO on health (Kling et al., 2007; Ludwig et al., 2011; Orr et al., 2003; Osypuk et al., 2012a, 2012b), including harmful effects on asthma (Fortson and Sanbonmatsu, 2010), the mechanisms through which MTO affects asthma have not been formally tested. The MTO experiment provides a rich source of data that we use to test whether specific potential mediators can explain these unexpected adverse effects on asthma, including: mental health, tobacco exposure, housing characteristics, and housing-related stressors. Potential mediators were selected based on evidence from prior research and on the feasibility of being affected by housing mobility. Before outlining our specific hypotheses, we review literature linking our candidate mediators with asthma.
Ample evidence, derived from multiple study designs, documents that asthma and mental health problems frequently co-occur (Katon et al., 2007, 2004; Richardson et al., 2006). Both asthma diagnosis (Katon et al., 2007, 2004) and asthma symptoms (Richardson et al., 2006) are highly co-morbid with depression and anxiety. For example, among adolescents with asthma, youth with depression or anxiety reported significantly more days with symptoms in the prior two weeks, than youth without depression or anxiety, even after controlling for asthma severity (Richardson et al., 2006). Explanations for the comorbidity range from cognitive, where the stress of coping with chronic asthma may provoke recurring panic attacks, to biological, where neurons in the brain are sensitized to produce an overactive fear response to recurrent asthma episodes (Katon et al., 2004).
Both environmental tobacco smoke exposure and active smoking are important triggers for asthma. The link between environmental tobacco smoke and asthma symptoms is well documented (Agabiti et al., 1999; Mannino et al., 2001; Martinez et al., 1995). A comprehensive review of the literature showed that active smoking is a risk factor for the onset of asthma, and is associated with decreased asthma control and increased mortality and symptom severity (McLeish and Zvolensky, 2010). Moreover, youth smoking may be an important mediator between neighborhood stressors and asthma symptomatology (Chen et al., 2007).
Housing characteristics may also trigger asthma, primarily through two mechanisms: poor housing conditions and housing-related stressors. Indoor air pollutants present in substandard quality housing environments, such as carpeted floors, pet dander, pest infestation, and dust mites (Institute of Medicine (2000)), can exacerbate asthma and respiratory symptoms (Sandel and Wright, 2006). The effects of physical housing characteristics on asthma are well-documented, but emotional and psychological aspects of housing can also adversely influence asthma (Sandel and Wright, 2006). Increasingly, research is linking housing-related stressors, such as crowded or cluttered living conditions, noise levels, hardship with paying for essentials like heat, and frequent residential moves, to asthma (Sandel and Wright, 2006; Suglia et al., 2010). Although informative, much of this research relies on observational studies, limiting causal inference. Moreover, much of the literature examining neighborhood effects on health has taken a “black box” approach, focusing on ill-defined concepts such as context and/or composition (e.g., area-level vs. individual-level poverty), rather than on specific mechanisms that may influence health (Macintyre et al., 2002). We address this gap by explicitly testing mediating mechanisms of the MTO experimental effects on adolescent asthma by examining a wide variety of asthma triggers as potential mediators, including mental health, tobacco exposure and use, housing quality, and residential mobility. Examining mediators at multiple levels, and including a range of factors from behavioral to neighborhood-level factors, is consistent with a broader eco-epidemiologic approach (Susser and Susser, 1996) and allows us to think beyond the black box to analyze “determinants and outcomes at different levels of organization” (Susser and Susser, 1996) (p. 676). We hypothesize that changes in mental health, tobacco exposure, and housing characteristics induced by the MTO experiment will partially explain some of the adverse findings of MTO on asthma. Prior research has documented that gender modifies some of the mediators of interest (e.g., mental health and smoking (Orr et al., 2003; Osypuk et al., 2012a, 2012b)). Therefore, we further hypothesize that gender-specific pathways of mediation may be present. Specifically, we expect the harmful effects of MTO on boys’ mental health and smoking may partially account for some of the harmful effects of MTO on asthma. We apply an innovative weight-based method to estimate these indirect effects: Inverse Odds Weighting (IOW).
2. Methods
2.1. Data
The Moving to Opportunity for Fair Housing Demonstration Project (MTO) was a randomized controlled trial (RCT) sponsored by the US Department of Housing and Urban Development (HUD, 1996) in 5 US cities (Boston, Baltimore, Chicago, Los Angeles, New York). Eligible low-income families had children under age 18, qualified for rental assistance, and lived in public housing or project-based assisted housing in areas with high concentrations of poverty (Feins and McInnis, 2001). Applicants were drawn from waiting lists, signed enrollment agreements and informed consent, completed the Baseline Survey, and were evaluated for eligibility (Goering et al., 1999) by public housing authorities.
2.1.1. Treatment assignment
Special software randomly assigned 4610 eligible volunteer families to one of three MTO treatment arms: the “regular Section 8” treatment group was offered Section 8 housing vouchers to subsidize a private market rental apartment in any neighborhood; the “low-poverty-neighborhood” treatment group was offered Section 8 vouchers redeemable only in low-poverty neighborhoods (<10% of Census Tract in poverty) along with housing counseling services to aid relocation; the control group was offered no further assistance but could remain in public housing (Goering et al., 1999). Although MTO contained two experimental (voucher) groups, both groups experienced similar improvements in neighborhood poverty by 2002 (albeit larger improvements for the low-poverty group immediately after randomization), treatment effects on asthma were similar for both groups, and formal tests for each outcome could not reject treatment-effect homogeneity (p > 0.05). Therefore, we combined the voucher groups to improve statistical power and parsimony.
2.1.2. Assessment
Baseline surveys (1994–1998) and the interim follow-up survey (2001–2002) were conducted via in-person interviews with household heads and their children (Goering et al., 1999; Orr et al., 2003). Our sample includes adolescents (n = 3537 aged 12–19 as of 5/31/2001) randomized through 12/31/1997 in the MTO Tier 1 Restricted Access Data. The effective response rate was 89.3% (Orr et al., 2003), resulting in an analytic sample of 2829 youth (experimental group n = 1950; control group n = 879). Adults provided informed written consent for themselves and their children (Feins and McInnis, 2001; Goering et al., 1999; Orr et al., 2003).
2.2. Measures
See Table 1 for sources of data, coding, and descriptive statistics of outcomes and mediators by domain, overall and by treatment group. See Supplemental Table 1 for descriptive statistics by gender and treatment group.
Table 1.
Adolescent outcome and mediator coding and descriptive statistics by domain, moving to opportunity data (2001–02).
| Domain & variable | Variable description | Total sample |
Experimental voucher group
|
Control group |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | ||
| Outcomes | ||||||||||
| Asthma diagnosis | Ever diagnosed with asthma; YR | 2812 | 0.23 | 0.42 | 1936 | 0.24 | 0.43 | 876 | 0.20 | 0.40 |
| Asthma attack | Asthma attack in the past year; 0 = no diagnosis/no attack, 1 = diagnosis and attack; YR | 2809 | 0.08 | 0.26 | 1933 | 0.08 | 0.28 | 876 | 0.06 | 0.23 |
| Wheezing/whistling | Wheezing/whistling symptoms in past year; 0 = no, 1 = yes; YR | 2811 | 0.17 | 0.38 | 1937 | 0.18 | 0.39 | 874 | 0.15 | 0.36 |
| Mediators | ||||||||||
| Mental health | ||||||||||
| Psychological distress | K6 psychological distress scale; 2-parameter binary IRT model, higher = more distress; YR | 2829 | −0.04 | 0.93 | 1950 | −0.04 | 0.93 | 879 | −0.04 | 0.92 |
| Behavior problems | Behavior problems index (BPI); 2-parameter binary IRT model, higher = more distress; YR | 2829 | −0.03 | 0.90 | 1950 | −0.01 | 0.89 | 879 | −0.06 | 0.90 |
| Smoking | ||||||||||
| Adult smoker | Adult is current smoker; 0 = no, 1 = yes; AR | 2725 | 0.30 | 0.46 | 1883 | 0.30 | 0.46 | 842 | 0.32 | 0.47 |
| Youth ever smoked | Youth ever smoked; 0 = no, 1 = yes; YR | 2812 | 0.22 | 0.41 | 1938 | 0.23 | 0.42 | 874 | 0.20 | 0.40 |
| Housing disarray | ||||||||||
| Rooms cluttered | Visible rooms in house were cluttered; 1 = very cluttered, 2 = somewhat cluttered, 3 = not at all cluttered; IO | 2625 | 2.43 | 0.71 | 1807 | 2.43 | 0.70 | 818 | 2.42 | 0.72 |
| Pet fur | Housing had cat, dog, or other pet fur; 0 = no, 1 = yes; IO | 2571 | 0.19 | 0.39 | 1775 | 0.18 | 0.39 | 796 | 0.21 | 0.41 |
| Interior-of-home index | Fraction of 7 negative interior housing unit characteristics, range 0–1; includes open cracks/holes in walls/ceilings, broken plaster/peeling paint, obvious dampness/mold, evidence of cigarette smoking, noisy from noise inside the house, noisy from noise outside the house, rooms were cluttered; IO | 2628 | 0.19 | 0.23 | 1817 | 0.18 | 0.23 | 811 | 0.21 | 0.23 |
| Housing quality-observed | ||||||||||
| No wall-to-wall carpet | Housing did not have wall-to-wall carpet; 0 = no, 1 = yes; IO | 2603 | 0.68 | 0.47 | 1800 | 0.65 | 0.48 | 803 | 0.74 | 0.44 |
| Broken plaster/peeling paint | Problem with broken plaster/peeling paint; 0 = no, 1 = yes; IO | 2633 | 0.13 | 0.34 | 1817 | 0.12 | 0.32 | 816 | 0.16 | 0.36 |
| Cracks/holes in windows/walls | Windows or walls had open cracks or holes; 0 = no, 1 = yes; IO | 2633 | 0.15 | 0.35 | 1816 | 0.14 | 0.35 | 817 | 0.15 | 0.36 |
| General condition of unit | Rating of unit condition or building conditions; 1 = well-kept or good, 2 = fair, 3 = poor, 4 = badly deteriorated; IO | 2673 | 1.87 | 0.77 | 1840 | 1.82 | 0.74 | 833 | 1.97 | 0.84 |
| Exterior-of-home index | Fraction of 7 negative exterior housing unit characteristics, range 0–1; includes unit in poor condition, housing on block in poor condition, building had broken windows, building had bars on windows, nearby buildings had bars on windows, condition of street was poor (i.e., pot holes), and major accumulation of trash/junk in neighborhood; IO | 2661 | 0.18 | 0.24 | 1834 | 0.17 | 0.22 | 827 | 0.21 | 0.26 |
| Housing quality-adult report | ||||||||||
| Broken locks | Problem with broken locks on door; 0 = no, 1 = yes; AR | 2745 | 0.17 | 0.37 | 1897 | 0.16 | 0.37 | 848 | 0.18 | 0.38 |
| Peeling paint/wallpaper | Problem with peeling paint or wallpaper; 0 = no, 1 = yes | 2744 | 0.45 | 0.50 | 1896 | 0.42 | 0.49 | 848 | 0.50 | 0.50 |
| Vermin | Problem with mice, rats, or cockroaches; 0 = no, 1 = yes | 2743 | 0.53 | 0.50 | 1896 | 0.51 | 0.50 | 847 | 0.57 | 0.50 |
| Broken windows | Problem with broken windows; 0 = no, 1 = yes; AR | 2745 | 0.24 | 0.42 | 1897 | 0.23 | 0.42 | 848 | 0.26 | 0.44 |
| Count of housing problems | Count of 7 items adult reported as being a big or small problem in housing; includes peeling paint/wallpaper, heat, plumbing, broken locks, broken windows, rats, and roaches; AR | 2745 | 2.06 | 1.95 | 1897 | 1.98 | 1.95 | 848 | 2.25 | 1.94 |
| Housing excellent or good | Adult rated condition of housing as excellent or good overall; 0 = no, 1 = yes; AR | 2744 | 0.56 | 0.50 | 1896 | 0.58 | 0.49 | 848 | 0.51 | 0.50 |
| Housing hardship | ||||||||||
| Heating problem | Problem with heating; 0 = no, 1 = yes; AR | 2733 | 0.19 | 0.39 | 1892 | 0.18 | 0.38 | 841 | 0.20 | 0.40 |
| Plumbing problem | Problem with plumbing; 0 = no, 1 = yes; AR | 2744 | 0.32 | 0.47 | 1896 | 0.32 | 0.46 | 848 | 0.34 | 0.47 |
| Utilities shut off | Gas, water, or electricity ever shut off for non-payment; 0 = no, 1 = yes; AR | 2745 | 0.06 | 0.24 | 1897 | 0.07 | 0.25 | 848 | 0.05 | 0.21 |
| Evicted | Adult was evicted in past 12 months; 0 = no, 1 = yes; AR | 2744 | 0.02 | 0.15 | 1896 | 0.03 | 0.16 | 848 | 0.02 | 0.14 |
| Homeless/doubled up | Adult was homeless or doubled up in past 12 months; 0 = no, 1 = yes; AR | 2743 | 0.06 | 0.24 | 1895 | 0.06 | 0.24 | 848 | 0.06 | 0.24 |
| Problem paying for rent or mortgage | Sum of problems paying for housing unit; 0 = no problems, 2 = a lot of problems; AR | 2726 | 0.26 | 0.57 | 1886 | 0.24 | 0.56 | 840 | 0.29 | 0.60 |
| Problem paying for utilities | Sum of problems paying for utilities; 0 = no problems, 5 = a lot of problems; AR | 2730 | 0.80 | 1.33 | 1890 | 0.87 | 1.37 | 840 | 0.63 | 1.22 |
| Housing mobility | ||||||||||
| One move | One move since baseline; 0 = no, 1 = yes; MD | 2829 | 0.338 | 0.473 | 1950 | 0.337 | 0.473 | 879 | 0.340 | 0.474 |
| Two+ moves | Two or more moves since baseline; 0 = no, 1 = yes; MD | 2829 | 0.438 | 0.496 | 1950 | 0.483 | 0.500 | 879 | 0.336 | 0.473 |
YR = youth self-report; IRT = item response theory; AR = adult self-report; IO = interviewer observation; MD = MTO administrative data.
2.2.1. Outcomes
We examined three youth self-reported, binary outcomes measured in 2002: lifetime asthma diagnosis (0 = never diagnosed with asthma by a health care provider, 1 = diagnosed with asthma; mean(SD) = 0.23(0.42)), past-year asthma attack (0 = never diagnosed with asthma, or, diagnosed with asthma but no asthma attack in past year; 1 = diagnosed with asthma and asthma attack in past year; mean(SD) = 0.08(0.26)), and past-year wheezing or whistling symptoms (0 = no, and 1 = yes, for wheezing/whistling symptoms in past year; mean(SD) = 0.17(0.38)). Although MTO did not measure baseline asthma diagnosis, treatment randomization should ensure balance among treatment groups at baseline. Therefore, any treatment group differences in asthma diagnosis at follow-up should indicate new diagnoses since baseline, so we use this measure as a proxy for asthma incidence since baseline. To assess uncontrolled asthma, we use past-year asthma attack and wheezing/whistling, which can identify asthma symptoms among subjects with no asthma diagnosis. Self-reported measures of asthma and respiratory symptoms by adolescents are valid (Guyatt et al., 1997). MTO also measured parent-reported asthma for adolescents; inter-rater agreement was moderate to high between parent and youth measures (asthma diagnosis kappa = 0.75, asthma attack kappa = 0.59, and wheezing/whistling kappa = 0.50). Sensitivity analyses with parent-reported outcomes yielded similar results (Supplemental Tables 2–7).
2.2.2. Mediators
Potential mediators were measured in 2002 (see Table 1). To simplify analyses, each potential mediator was grouped into a domain, and in the mediation models, all component variables in a domain were entered into the model simultaneously. The mediator domains (and component variables) include: mental health (psychological distress scale, behavior problems index; see (Osypuk et al., 2012a, 2012b) for details on items and construction of these measures); smoking (adult in home smokes, youth ever smoked); housing disarray (cluttered rooms, presence of pet fur, index of negative interior-of-home characteristics); interviewer-observed housing quality (wall-to-wall carpeting, broken plaster/peeling paint, cracks/holes in windows or walls, general condition of housing unit, index of negative exterior-of-home characteristics); adult-reported housing quality (broken locks, peeling paint/wall-paper, vermin, broken windows, count of housing problems, rating of housing as good or excellent); housing hardship (problems with heating, problems with plumbing, utilities were shut off, household head was evicted, household head was homeless/doubled up, problems paying rent/mortgage, problems paying for utilities); housing mobility (moved once since baseline, moved two or more times since baseline). The housing measures were grouped together into 5 domains based on prior empirical evidence (Sandel and Wright, 2006; Suglia et al., 2010). We tested health care access and neighborhood domains (i.e., neighborhood disorder, safety, and satisfaction, and census variables) as mediators, yet none was significant (results not shown).
2.2.3. Baseline characteristics
To adjust for potential confounding of the mediator–outcome relationship, we adjust all regression models for any baseline characteristics significantly related (at p < 0.10) to each asthma outcome. Baseline characteristics include: youth gender, age; site; household head never married, received AFDC/TANF, was in school, had a car, lived in the neighborhood for 5 + years, moved more than three times in last five years, was very dissatisfied with neighborhood, was likely to tell neighbor if neighborhood child was getting in trouble, had no family or friends (separately) in the neighborhood, applied for section 8 before; household member was disabled, a crime victim, household had no teenagers; household size; youth received help for behavioral/emotional problem, school called to discuss youth’s school work/behavior problems, youth had problem that interfered with school or play, youth had problem requiring special medicine or equipment. Baseline characteristics were balanced across treatment groups as expected by the RCT design (Supplemental Table 8).
2.3. Analytic plan
We estimated intention-to-treat (ITT) models using baseline characteristic-adjusted logistic regression, separately for each asthma outcome. Before testing mediation, we assessed how treatment affected the potential mediators of interest using two tests. Because we test domains of mediators, we first examined whether treatment changed the mediators collectively within a domain. Therefore, adjusting for baseline characteristics, we predicted treatment from all mediators within a domain, for each domain. We then estimated a Wald test of joint significance that, collectively, the mediators in each domain significantly differed from zero (Table 2). This test does not indicate directionality of the MTO treatment effects, so, to examine how MTO treatment affected each specific mediator, including directionality, we next estimated first-leg mediation models (MTO treatment associations with each mediator individually) using linear, logistic, or multinomial regression, depending on each mediator’s functional form. These models adjusted for all baseline characteristics associated with any asthma outcome (Supplemental Table 9).
Table 2.
First-leg results: MTO treatment regressed on mediators, by domain.
| Mediator domainsa | Total sample |
Boys |
Girls |
|||
|---|---|---|---|---|---|---|
| χ2 | p | χ2 | p | χ2 | p | |
| Mental healthb | 3.60 | 0.166 | 9.96 | 0.007 | 3.88 | 0.144 |
| Smoking | 2.95 | 0.228 | 9.40 | 0.009 | 2.53 | 0.282 |
| Housing disarray | 7.72 | 0.052 | 7.18 | 0.067 | 3.60 | 0.308 |
| Housing quality observed | 27.33 | 0.000 | 16.13 | 0.007 | 17.98 | 0.003 |
| Housing quality adult report | 12.11 | 0.060 | 10.62 | 0.101 | 10.96 | 0.090 |
| Housing hardship | 20.42 | 0.005 | 13.96 | 0.052 | 17.42 | 0.015 |
| Housing mobility | 54.38 | 0.000 | 14.51 | 0.001 | 58.97 | 0.000 |
NOTE: From a model predicting treatment from all variables in a domain, plus baseline characteristics; reporting the Wald test of joint significance and associated p-value for whether the group of variables in each domain significantly predict treatment.
Each mediator domain included the group of variables detailed in Table 1.
We also tested a model adding generalized anxiety disorder; treatment significantly changed this group of mediators for the total sample (χ2 = 8.17, p = 0.04), boys (χ2 = 9.40, p = 0.02), and girls (χ2 = 9.80, p = 0.02).
We apply the Inverse Odds Weighting (IOW) method to test mediation of MTO on our binary asthma outcomes, as illustrated in the directed acyclic graph (DAG) in Fig. 1. Parametric (regression based) approaches are commonly used to test mediation, but most require linear outcomes (Baron and Kenny, 1986). With nonlinear models, the decomposition of direct and indirect effects would be incorrect. The IOW method resolves this by using a semiparametric method that condenses information on the relationship between the treatment and mediators, conditioned on covariates, into a weight. These weights are then used to estimate the direct effect by deactivating all indirect pathways, and the indirect effect (indicating mediation by the mediator variables tested) is calculated by subtracting the direct from the total effect (Tchetgen Tchetgen, In Press).
Fig. 1.
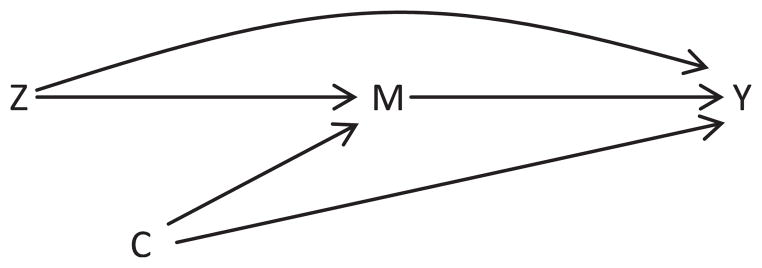
Title. Directed acyclic graph testing mediation of MTO treatment effects on asthma. Notes: Z = MTO treatment; M = Mediators (mental health, smoking, housing disarray, housing quality, housing hardship, and housing mobility); Y = asthma outcomes (asthma diagnosis, asthma Attack, and wheezing/whistling); C = Confounders.
To apply the IOW method, we first recovered the predicted odds for each individual from a logistic regression predicting treatment from all mediators in a domain, plus baseline characteristics. For example, for the mental health mediator domain, we predicted treatment from psychological distress, behavior problems, and baseline characteristics, to create the mental health IOW mediation weight. Next, we took the inverse of this predicted odds to create the IOW weight. Total effects of MTO treatment on asthma outcomes were estimated using generalized linear models (GLM) with a logit link, without mediators. Direct effects (the effect of treatment not operating through the modeled mediators) were calculated using a GLM with logit link, adjusting for the mediators by applying the IOW weights. Then, indirect effects were calculated by subtracting the direct effect from the total effect. All analyses were estimated using bootstrapping (500 replications) to recover correct standard errors for direct and indirect effects in Stata 11.0, and were adjusted for family-level clustering and weights. We tested for and found no evidence of area-level clustering. Given the qualitative gender effect modification of MTO treatment on certain mediators (e.g., mental health and smoking) (Kling et al., 2007; Osypuk et al., 2012a, 2012b), we tested gender-pooled and gender-stratified mediation. We focused on gender in lieu of sex differences since we are interested in the culturally-bound social experiences and contexts of boys and girls, rather than biological differences (Krieger, 2003). To quantify the magnitude of mediation, we estimated the percent change ((direct effect – total effect)/total effect). Positive values indicate an increase, or a countervailing (masked) mediation effect, and negative values indicate a decrease, or mediation in the expected direction, in the direct effect compared to the total effect. We also estimated a model incorporating all mediators together; results were non-significant (not shown). Northeastern University’s Institutional Review Board approved this study.
3. Results
3.1. Gender-pooled results
We found a harmful (total) effect of MTO treatment compared to controls for adolescent asthma diagnosis (b(SE) = 0.244(0.131), p = 0.062) and past-year asthma attack (b(SE) = 0.438(0.190), p = 0.021), and a nonsignificant harmful effect on past-year wheezing symptoms (b(SE) = 0.172(0.126), p = 0.173). Total effects of MTO on parent-reported asthma outcomes were also harmful and of similar, albeit slightly larger, magnitude (Supplemental Tables 2–4).
First-leg analyses of treatment–mediator associations indicate that MTO treatment significantly changed the following domains of mediators: mental health (boys), smoking (boys), housing disarray (total sample and boys), interviewer-observed and adult-reported housing quality, housing hardship, and housing mobility, as indicated in Table 2, which presents a Wald-statistic for the joint effect of all mediators within a domain on MTO treatment. Specifically (see Supplemental Table 9), MTO treatment increased boys’ psychological distress, behavior problems, and smoking prevalence, while it decreased girls’ psychological distress. MTO treatment also decreased indices of the fraction of indoor and outdoor negative housing characteristics present in the participants’ unit, decreased the presence of broken plaster/peeling paint/peeling wallpaper, cracks/holes in windows/walls, vermin, broken windows, reduced the number of housing unit problems, and improved the general condition and rating of housing. Wall-to-wall carpeting increased for the treatment group. There were mixed effects for housing hardship, with improvements in some aspects (i.e., participants had fewer problems with plumbing and paying rent/mortgage) and declines in other aspects (i.e., subjects had more problems paying utilities and having utilities shut off). As expected, treatment fostered more frequent housing mobility.
Despite that MTO treatment resulted in many differences between experimental and control groups 4–7 years after random assignment, mediation analyses with the total sample demonstrated no significant mediation in any domain for asthma diagnosis (Table 3), asthma attack (Table 4), or wheezing (Table 5), indicated by no significant indirect effects. In most instances, the indirect effect is negative indicating a countervailing, albeit nonsignificant, effect. Essentially, the severity of the adverse treatment effect was masked by the beneficial association between MTO and our tested mediators.
Table 3.
IOW Mediation of the adolescent MTO treatment-asthma diagnosis association; direct and indirect effects.
| Mediator domains | Direct effect |
Indirect effect |
% Change |
N | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | % Changeb | LCI | UCI | ||
| Mental healtha | 0.2482 | 0.137 | 0.070 | −0.0047 | 0.031 | 0.882 | 1.9% | −126.3% | 130.1% | 2812 |
| Smoking | 0.2279 | 0.139 | 0.100 | −0.0141 | 0.029 | 0.623 | 6.6% | −908.6% | 921.8% | 2693 |
| Housing disarray | 0.2871 | 0.142 | 0.043 | −0.0200 | 0.031 | 0.520 | 7.5% | −61.4% | 76.4% | 2534 |
| Housing quality observed | 0.2389 | 0.132 | 0.070 | −0.0044 | 0.037 | 0.906 | 1.9% | −146.5% | 150.3% | 2575 |
| Housing quality adult report | 0.2686 | 0.135 | 0.047 | −0.0445 | 0.032 | 0.160 | 19.9% | −289.8% | 329.6% | 2727 |
| Housing hardship | 0.2270 | 0.129 | 0.078 | 0.0037 | 0.035 | 0.916 | −1.6% | −454.4% | 451.2% | 2684 |
| Housing mobility | 0.2702 | 0.142 | 0.056 | −0.0266 | 0.042 | 0.527 | 10.9% | −173.0% | 194.9% | 2812 |
We tested a model including generalized anxiety disorder as a mediator; results were similar, with a percent change of −1.4%.
% change indicates the % change from the total to the direct effect. Positive values indicate an increase, or a countervailing mediation effect, and negative values indicate a decrease, or mediation in the expected direction, in the direct effect compared to the total effect. The total effect of MTO treatment on asthma diagnosis was b(SE) = 0.244(0.131), p = 0.062.
Table 4.
IOW Mediation of the adolescent MTO treatment-asthma Attack association; direct and indirect effects.
| Mediator domains | Direct effect |
Indirect effect |
% Change |
N | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | % Changeb | LCI | UCI | ||
| Mental healtha | 0.4679 | 0.206 | 0.023 | −0.0300 | 0.037 | 0.422 | 6.8% | −86.5% | 100.2% | 2809 |
| Smoking | 0.4737 | 0.194 | 0.015 | −0.0153 | 0.030 | 0.606 | 3.3% | −51.4% | 58.1% | 2690 |
| Housing disarray | 0.4765 | 0.204 | 0.020 | −0.0337 | 0.028 | 0.236 | 7.6% | −142.4% | 157.6% | 2531 |
| Housing quality observed | 0.4573 | 0.201 | 0.023 | −0.0175 | 0.039 | 0.652 | 4.0% | −84.5% | 92.5% | 2572 |
| Housing quality adult report | 0.5308 | 0.195 | 0.006 | −0.0505 | 0.038 | 0.185 | 10.5% | −49.0% | 70.1% | 2724 |
| Housing hardship | 0.5112 | 0.188 | 0.007 | −0.0239 | 0.040 | 0.549 | 4.9% | −45.2% | 55.0% | 2681 |
| Housing mobility | 0.4967 | 0.209 | 0.018 | −0.0587 | 0.051 | 0.248 | 13.4% | −153.6% | 180.5% | 2809 |
We tested a model including generalized anxiety disorder as a mediator; results were similar, with a percent change of 5.8%.
% change indicates the % change from the total to the direct effect. Positive values indicate an increase, or a countervailing mediation effect, and negative values indicate a decrease, or mediation in the expected direction, in the direct effect compared to the total effect. The total effect of MTO treatment on asthma attack was b(SE) = 0.438(0.190), p = 0.021.
Table 5.
IOW Mediation of the adolescent MTO treatment-wheezing/whistling association; direct and indirect effects.
| Mediator domains | Direct effect |
Indirect effect |
% Change |
N | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | % Changeb | LCI | UCI | ||
| Mental healtha | 0.1702 | 0.127 | 0.180 | 0.0016 | 0.032 | 0.961 | −0.9% | −657.9% | 656.1% | 2811 |
| Smoking | 0.1892 | 0.129 | 0.143 | 0.0060 | 0.017 | 0.726 | −3.1% | −90.9% | 84.8% | 2693 |
| Housing disarray | 0.1871 | 0.130 | 0.150 | −0.0032 | 0.021 | 0.877 | 1.7% | −101.8% | 105.3% | 2533 |
| Housing quality observed | 0.1458 | 0.140 | 0.298 | 0.0005 | 0.025 | 0.983 | −0.4% | −261.2% | 260.5% | 2573 |
| Housing quality adult report | 0.2235 | 0.127 | 0.078 | −0.0290 | 0.027 | 0.274 | 14.9% | −478.3% | 508.2% | 2725 |
| Housing hardship | 0.1981 | 0.129 | 0.126 | 0.0116 | 0.030 | 0.695 | −5.5% | −183.4% | 172.3% | 2683 |
| Housing mobility | 0.2149 | 0.133 | 0.106 | −0.0432 | 0.036 | 0.230 | 25.1% | −291.8% | 342.1% | 2811 |
We tested a model including generalized anxiety disorder as a mediator; results were similar, with a percent change of 3.5%.
% change indicates the % change from the total to the direct effect. Positive values indicate an increase, or a countervailing mediation effect, and negative values indicate a decrease, or mediation in the expected direction, in the direct effect compared to the total effect. The total effect of MTO treatment on wheezing/whistling was b(SE) = 0.172(0.126), p = 0.173.
3.2. Gender-stratified results
We found significant adverse total effects of MTO treatment on asthma attack for both boys and girls after gender-stratifying (boys: b(SE) = 0.595(0.294), p = 0.043; girls: b(SE) = 0.425(0.257), p = 0.098). Total effects on the other outcomes were also adverse for both genders, but nonsignificant (asthma diagnosis: boys b(SE) = 0.193(0.195), p = 0.321, girls: b(SE) = 0.270(0.172), p = 0.116; wheezing: boys b(SE) = 0.305(0.190), p = 0.108, girls b(SE) = 0.062(0.172), p = 0.719). Total effects were statistically homogenous across gender (not reported).
We found some evidence for countervailing indirect mediation effects among girls on asthma diagnosis in a few domains (Supplemental Table 10); after accounting for the mediators, the direct effect of treatment on asthma increased compared to the total effect. Indirect effects for smoking (p = 0.053), and adult-reported housing quality (p = 0.063) indicate marginally-significant (albeit countervailing) mediation, with direct effects for girls that were larger than total effects by 35% and 42% respectively. Improvements in these domains served to reduce, or mask, what would have been a more detrimental effect of MTO among girls in the treatment group; in other words, after accounting for improvements in housing quality, the effects of treatment on asthma were 42% worse. Mediation patterns differed by gender, suggesting that mediation may be gender-specific.
We found no significant mediation of MTO treatment on asthma diagnosis for boys, yet, there was one interesting trend. MTO treatment had a harmful effect on boys’ mental health, and this appears to account for, albeit non-significantly (p = 0.37), a portion of the harmful effect of treatment on asthma diagnosis. Boys’ mental health showed a suggestion of partially mediating the total effect of MTO treatment on asthma diagnosis by 27% in the expected direction, from an effect size of 0.19 (total effect) to 0.14 (direct effect). We found no significant mediation for asthma attack for either gender (Supplemental Table 11), and only one significant countervailing indirect effect for housing mobility on wheezing in girls (p = 0.041) (Supplemental Table 12).
4. Discussion
We anticipated that MTO would have improved asthma among a low-income population that moved from distressed public housing and impoverished neighborhoods into better housing and neighborhood environments. However, unexpectedly, this intervention worsened asthma outcomes. The treatment group exhibited higher lifetime asthma diagnosis at follow-up (marginally), a proxy for asthma incidence since baseline, as well as a higher prevalence of past-year asthma attack (significantly) and wheezing/whistling symptoms (non-significantly), which captures uncontrolled asthma. However, given that asthma diagnosis was not measured at baseline, we cannot conclude whether asthma worsened among those already diagnosed before baseline.
We tested whether a wide range of possible mediators (mental health, smoking, and housing, as well as health care access and neighborhood factors (the latter two analyses not shown)) could account for these unexpected adverse effects. Although MTO improved several mediators (except mental health and smoking of boys, which worsened, and medical care, which was unchanged) and certain domains suggested mediation (albeit nonsignificant) for asthma diagnosis and wheezing, overall these mediators did not account for the detrimental effect of the intervention on asthma. The few indirect effects that we find are countervailing, i.e., if the mediators had not improved, the intervention would have been even more harmful. In sum, we were unable to account for the detrimental effect of MTO on asthma.
There was one exception to the countervailing mediation pattern. MTO treatment worsened boys’ mental health and mental health reduced the total effect of treatment on asthma diagnosis by 27%. Worse mental health in boys partially accounted for the harmful effect of MTO on asthma in this group. Although not statistically significant, this effect suggests a domain that warrants further investigation, particularly given the links between mental health and asthma (Katon et al., 2007, 2004; Miles et al., 1997; Richardson et al., 2006). Understanding how gender modifies the relationships between asthma, mental health, and housing mobility might contribute to our understanding of the high frequency at which asthma and mental health co-occur, and how they influence each other, particularly since moving to a new environment can be a stressor (DeLuca and Dayton, 2009) that may exacerbate asthma. It is important for future research to untangle these relationships.
Nonetheless, our answer is unsatisfying: our analysis did not account for the adverse effects of MTO on adolescent asthma, despite the testing of many promising potential mediators. It may be that the MTO evaluation did not measure the most relevant mediators linking housing mobility with asthma. For example, air pollution (Astell-Burt et al., 2013; Qian et al., 2004; Tabaku et al., 2011), outdoor pollen, and mold exposure (Creticos et al., 1996; O’Hollaren et al., 1991; Targonski et al., 1995) have been linked to neighborhoods, asthma, and respiratory health, but were not measured in MTO. Perhaps treatment group movers moved to neighborhoods with increased exposure to allergens through environmental pollutants and/or green space. We linked external neighborhood observational measures of tree canopy and community gardens to proxy for outdoor exposures; however, data was only available for one site and mediation models either would not converge or were non-significant. Future research should explore potential mediators detrimental for asthma outcomes that may have increased with moves away from concentrated poverty areas. For example, environmental samples that explicitly measure indoor allergen exposure, air pollution, and other toxic emissions, and measures such as proximity to highways and green space (e.g., parks, yard space), would provide indicators of allergen exposure that may exacerbate respiratory illnesses.
In contrast, moving to cleaner environments, like the better housing units to which MTO treatment group members moved, may disrupt the development of immunities to allergens, thereby exacerbating allergies and asthma (Brooks et al., 2013). Evidence for this hygiene hypothesis is mixed (Brooks et al., 2013; Ramsey and Celedón, 2005), and it is unclear how the timing of life course exposure to allergens may protect against asthma (Yan et al., 2013). The MTO data does not have information on early life exposures or exposure to specific allergens before baseline that may protect against asthma, so this is another potential avenue for future investigation. Ideally, a combination of in-depth qualitative interviews to probe specific, individual pre-randomization allergen exposures and larger-scale externally-measured quantitative data would help us untangle these harmful effects of MTO on asthma, and illuminate what, if any, role life course timing has on these relationships.
Measurement error of asthma (or indeed, of the mediators) may be operating. The gold standard for measuring asthma is to assess severity of symptoms, control of symptoms, and responsiveness to treatment (NHLBI, 2007), such as in the asthma control test (ACT) (Nathan et al., 2004). A measure of this nature was unavailable in the MTO data, and measures that were captured in MTO may be less sensitive to treatment effects. For example, relying on lifetime asthma diagnosis is not ideal for several reasons. First, we do not have measures of new asthma cases (incidence) since baseline, which would be more sensitive to picking up causal effects of interventions, since baseline asthma was not measured. Second, our measures may conflate asthma diagnosis with receipt of medical care. Because only individuals who have received medical care for asthma symptoms can be physician-diagnosed with the disease, we may be underestimating the prevalence of youth with asthma. One study estimated 30% of children in their sample exhibited asthma symptoms with no official diagnosis (Grant et al., 1999). Past-year asthma attack and past-year wheezing/whistling are intended to assess uncontrolled asthma, but they assess symptoms near the end of follow up, not the beginning, when the largest changes in neighborhood and housing environment were anticipated to have occurred. Despite these limitations, it is reassuring that we found a consistent pattern of total effects for all three outcomes, although we did not find a consistent pattern of mediation.
Our nonsignificant mediation findings may be an artifact of the IOW mediation method, which may be less efficient compared to parametric approaches. There is some indication of this, as several indirect effects amounted to a 20% or more change in the total effect (indicating the indirect effect is not close to zero), yet the effects remained nonsignificant. IOW is less efficient because, unlike the product method (Baron and Kenny, 1986), the relationship between the mediator and outcome is not explicitly modeled, but rather is incorporated in the weight, meaning IOW explains less variability in the mediator–outcome relationship.
The gender-specific IOW results especially are underpowered, because of smaller sample sizes, yet we find marginally significant indirect effects on asthma diagnosis for girls in the smoking and housing quality domains. This suggests that different pathways may operate for girls and boys, a notion the literature supports. A review of the impact of gender on asthma during childhood and adolescence noted that although boys report more wheezing and asthma than girls, the pattern reverses during adolescence, with girls experiencing more severe asthma (Almqvist et al., 2008). Potential reasons for the increased severity among adolescent girls include hormonal changes or a greater susceptibility to environmental exposures (Almqvist et al., 2008). To the extent that environmental exposures are more prevalent in poor quality housing, if girls in the MTO treatment group experienced better housing quality, this could explain why housing quality masks more harmful treatment effects. Household smoke exposure also has been linked with asthma attack among girls but not boys (Strong and Chang, 2013), indicating smoking as another possible gender-specific pathway.
4.1. Limitations
Our study has some limitations. The potential mediators were measured contemporaneously with asthma, so temporal ordering necessary for causal inference is not preserved. Yet even if our results suggest covariation, instead of mediation, this provides more information on how both were affected by MTO, since no prior studies have investigated why MTO generated these health effects. The experimental design of MTO allows us to estimate an unbiased causal total effect of housing mobility on asthma, and an unbiased effect of housing mobility on any mediator (Ludwig et al., 2008), but it does not allow us to estimate an unbiased mediator-outcome association, since the mediator was not randomized. Valid estimation of the mediator-outcome association, even in an RCT, requires controlling for all baseline confounders of this association. Residual confounding may bias our mediation estimation if MTO did not measure all baseline confounders.
The majority of our tested mediators were self-reported, in lieu of objective chemical or biological measures, which may have captured greater variability. We did have interviewer-observed housing quality measures, but even these generated few significant results. Environmental housing measures, such as dust samples to measure allergen levels, were unavailable in MTO. Moreover, we had few measures of the outdoor environment, which may be strong triggers of asthma. Although we tested potential mediators across different levels, including individual/behavioral characteristics, housing, and neighborhoods, to elucidate the black box effects of residential mobility (Susser and Susser, 1996), we have not elucidated these effects successfully. Therefore, there is room for improving the measurement of health-relevant housing and neighborhood quality in future housing mobility studies.
In closing, we found few explanations for why residential mobility caused increased asthma symptoms and diagnoses among adolescents in the MTO treatment group. The few significant mediation effects on asthma were gender-specific and countervailing; MTO improved housing, which masked what would have been more detrimental effects. Our results, and others, suggest that gender is a powerful modifier of housing and neighborhood effects on health (Osypuk et al., 2012a, 2012b), so gender-specific pathways should continue to be explored. Notably, despite any explicit health components built into the MTO program, health remains the predominant domain affected by the MTO program at both the interim (4–7 year) and final (10–15 year) follow-ups (Orr et al., 2003; Sanbonmatsu et al., 2011). Unlike MTO effects on asthma, some program effects have been positive, such as on obesity, diabetes, and girls’ mental health (Sanbonmatsu et al., 2011). The adverse effects of MTO on asthma or boys’ mental health should be assessed along with the beneficial effects on adult mental and physical health, and girls’ mental health. We need to better understand the pathways that led to these divergent health outcomes, so that policies can promote positive effects and mitigate adverse effects. This may require baseline health assessments of participants, and the integration of health (e.g., mental health counseling) and wrap around services across sectors into housing interventions. Ultimately, this could strengthen and enhance the positive health impacts for low-income populations receiving housing assistance via housing choice vouchers.
Supplementary Material
Acknowledgments
This work was supported by NIH grants R01MD006064 and R21HD066312 (Dr. Osypuk, PI). Funders did not have any role in design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. We thank Eric Tchetgen Tchetgen, PhD for his analytic guidance, and Megan Sandel, MD for her early contributions to this manuscript.
Abbreviations
- MTO
moving to opportunity
- RCT
randomized controlled trial
- MI
multiple imputation
- MICE
multiple imputation by chained equations
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.socscimed.2014.02.020.
References
- Agabiti N, Mallone S, Forastiere F, Corbo GM, Ferro S, Renzoni E, et al. The impact of parental smoking on asthma and wheezing. Epidemiology. 1999;10:692–698. doi: 10.1097/00001648-199911000-00005. [DOI] [PubMed] [Google Scholar]
- Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. NCHS Data Brief. 94. National Center for Health Statistics; Hyattsville, MD: 2012. Trends in Asthma Prevalence, Health Care Use, and Mortality in the United States, 2001–2010. [PubMed] [Google Scholar]
- Almqvist C, Worm M, Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy. 2008;63:47–57. doi: 10.1111/j.1398-9995.2007.01524.x. [DOI] [PubMed] [Google Scholar]
- Astell-Burt T, Maynard MJ, Lenguerrand E, Whitrow MJ, Molaodi OR, Harding S. Effect of air pollution and racism on ethnic differences in respiratory health among adolescents living in an urban environment. Health & Place. 2013;23:171–178. doi: 10.1016/j.healthplace.2013.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Brooks C, Pearce N, Douwes J. The hygiene hypothesis in allergy and asthma: an update. Current Opinion in Allergy and Clinical Immunology. 2013;13:70–77. doi: 10.1097/ACI.0b013e32835ad0d2. [DOI] [PubMed] [Google Scholar]
- CDC. Vital Signs. National Center for Environmental Health, Division of Environmental Hazards and Health Effects; Atlanta, GA: 2011. Asthma in the US: Growing Every Year. [Google Scholar]
- Chen E, Chim LS, Strunk RC, Miller GE. The role of the social environment in children and adolescents with asthma. American Journal of Respiratory and Critical Care Medicine. 2007;176:644–649. doi: 10.1164/rccm.200610-1473OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creticos PS, Reed CE, Norman PS, Khoury J, Adkinson NF, Buncher CR, et al. Ragweed immunotherapy in adult asthma. The New England Journal of Medicine. 1996;334:501–506. doi: 10.1056/NEJM199602223340804. [DOI] [PubMed] [Google Scholar]
- DeLuca S, Dayton E. Switching social contexts: the effects of housing mobility and school choice programs on youth outcomes. Annual Review of Sociology. 2009;35:457–491. [Google Scholar]
- Feins JD, McInnis D. The Interim Impact Evaluation for the Moving to Opportunity Demonstration, C-OPC-21484. Abt Associates Inc; Cambridge, MA: 2001. [Google Scholar]
- Fortson JG, Sanbonmatsu L. Child health and neighborhood conditions: results from a randomized housing voucher experiment. The Journal of Human Resources. 2010;45:840–864. [Google Scholar]
- Goering J, Kraft J, Feins J, McInnis D, Holin MJ, Elhassan H. Moving to Opportunity for Fair Housing Demonstration Program: Current Status and Initial Findings. US Department of Housing & Urban Development, Office of Policy Development and Research; Washington, DC: 1999. [Google Scholar]
- Grant EN, Daugherty SR, Moy JN, Nelson SG, Piorkowski JM. Prevalence and burden of illness for asthma and related symptoms among kindergartners in Chicago public schools. Annals of Allergy, Asthma & Immunology. 1999;83:113–120. doi: 10.1016/S1081-1206(10)62621-X. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Juniper EF, Griffith LE, Feeny DH, Ferrie PJ. Children and adult perceptions of childhood asthma. Pediatrics. 1997;99:165–168. doi: 10.1542/peds.99.2.165. [DOI] [PubMed] [Google Scholar]
- HUD. Expanding Housing Choices For HUD-Assisted Families: Moving to Opportunity. First Biennial Report to Congress, Moving to Opportunity for Fair Housing Demonstration Program.1996. [Google Scholar]
- Institute of Medicine. Clearing the Air: Asthma and Indoor Air Exposures. Committee on the Assessment of Asthma and Indoor Air, Division of Health Promotion and Disease Prevention; Washington, D.C. 2000. [Google Scholar]
- Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared to controls. Journal of Adolescent Health. 2007;41:455–463. doi: 10.1016/j.jadohealth.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W, Richardson L, Lozano P, McCauley E. The relationship of asthma and anxiety disorders. Psychosomatic Medicine. 2004;66:349–355. doi: 10.1097/01.psy.0000126202.89941.ea. [DOI] [PubMed] [Google Scholar]
- Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75:83–119. [Google Scholar]
- Krieger N. Genders, sexes, and health: what are the connections–and why does it matter? International Journal of Epidemiology. 2003;32:652–657. doi: 10.1093/ije/dyg156. [DOI] [PubMed] [Google Scholar]
- Ludwig J, Liebman JB, Kling JR, Duncan GJ, Katz LF, Kessler RC, et al. What can we learn about neighborhood effects from the moving to opportunity experiment? A comment on Clampet-Lundquist and Massey. American Journal of Sociology. 2008;114:144–188. [Google Scholar]
- Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, et al. Neighborhoods, obesity, and diabetes - a randomized social experiment. The New England Journal of Medicine. 2011;365:1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise, and measure them? Social Science & Medicine. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Mannino DM, Moorman JE, Kingsley B, Rose D, Repace J. Health effects related to environmental tobacco smoke exposure in children in the United States: data from the Third National Health and Nutrition Examination Survey. Archives of Pediatric and Adolescent Medicine. 2001;155:36–41. doi: 10.1001/archpedi.155.1.36. [DOI] [PubMed] [Google Scholar]
- Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ, et al. Asthma and wheezing in the first six years of life. The New England Journal of Medicine. 1995;332:133–138. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ. Asthma and cigarette smoking: a review of the empirical literature. Journal of Asthma. 2010;47:345–361. doi: 10.3109/02770900903556413. [DOI] [PubMed] [Google Scholar]
- Miles JF, Garden GMF, Tunnicliffe WS, Cayton RM, Ayres JG. Psychological morbidity and coping skills in patients with brittle and non-brittle asthma: a case-control study. Clinical & Experimental Allergy. 1997;27:1151–1159. doi: 10.1046/j.1365-2222.1997.1080961.x. [DOI] [PubMed] [Google Scholar]
- Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: a survey for assessing asthma control. Journal of Allergy and Clinical Immunology. 2004;113:59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- NHLBI. National Asthma Education and Prevention Program. US Department of Health and Human Services, National Institutes of Health; Bethesda, MD: 2007. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. [Google Scholar]
- O’Hollaren MT, Yunginger JW, Offord KP, Somers MJ, O’Connell EJ, Ballard DJ, et al. Exposure to an aeroallergen as a possible precipitating factor in respiratory arrest in young patients with asthma. The New England Journal of Medicine. 1991;324:359–363. doi: 10.1056/NEJM199102073240602. [DOI] [PubMed] [Google Scholar]
- Orr L, Feins JD, Jacob R, Beecroft E, Sanbonmatsu L, Katz LF, et al. Moving to Opportunity for Fair Housing Demonstration Program: Interim Impacts Evaluation. U.S. Department of Housing and Urban Development, Office of Policy Development and Research; Washington, DC: 2003. p. 341. [Google Scholar]
- Osypuk TL, Schmidt NM, Bates LM, Tchetgen-Tchetgen EJ, Earls FJ, Glymour MM. Gender and crime victimization modify neighborhood effects on adolescent mental health. Pediatrics. 2012a;130:472–481. doi: 10.1542/peds.2011-2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osypuk TL, Tchetgen Tchetgen EJ, Acevedo-Garcia D, Earls FJ, Lincoln A, Schmidt NM, et al. Differential mental health effects of neighborhood relocation among youth in vulnerable families. Archives of General Psychiatry. 2012b;69:1284–1294. doi: 10.1001/archgenpsychiatry.2012.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian Z, Chapman RS, Hu W, Wei F, Kom LR, Zhang JJ. Using air pollution based community clusters to explore air pollution health effects in children. Environment International. 2004;30:611–620. doi: 10.1016/j.envint.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Ramsey CD, Celedón JC. The hygiene hypothesis and asthma. Current Opinion in Pulmonary Medicine. 2005;11:14–20. doi: 10.1097/01.mcp.0000145791.13714.ae. [DOI] [PubMed] [Google Scholar]
- Richardson L, Lozano P, Russo J, McCauley E, Bush T, Katon W. Asthma symptom burden: relationship to asthma severity and anxiety and depression symptoms. Pediatrics. 2006:118. doi: 10.1542/peds.2006-0249. [DOI] [PubMed] [Google Scholar]
- Sanbonmatsu L, Ludwig J, Katz LF, Gennetian LA, Duncan GJ, Kessler RC, et al. Moving to Opportunity for Fair Housing Demonstration Program: Final Impacts Evaluation. U.S. Department of Housing and Urban Development, Office of Policy Development and Research; Washington, D.C: 2011. [Google Scholar]
- Sandel MT, Wright RJ. When home is where the stress is: expanding the dimensions of housing that influence asthma morbidity. Archives of Disease in Childhood. 2006;91:942–948. doi: 10.1136/adc.2006.098376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong C, Chang L-Y. Family socioeconomic status, household tobacco smoke, and asthma attack among children below 12 years of age: gender differences. Journal of Child Health Care. 2013:1–11. doi: 10.1177/1367493513496672. published online. [DOI] [PubMed] [Google Scholar]
- Suglia SF, Duarte CS, Sandel MT, Wright RJ. Social and environmental stressors in the home and childhood asthma. Journal of Epidemiology & Community Health. 2010;64:636–642. doi: 10.1136/jech.2008.082842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susser M, Susser E. Choosing a future for epidemiology: II. From black box to Chinese boxes and eco-epidemiology. American Journal of Public Health. 1996;86:674–677. doi: 10.2105/ajph.86.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabaku A, Bejtja G, Bala S, Toci E, Resuli J. Effects of air pollution on children’s pulmonary health. Atmospheric Environment. 2011;45:7540–7545. [Google Scholar]
- Targonski PV, Persky VW, Ramekrishnan V. Effect of environmental molds on risk of death drom asthma during the pollen season. Journal of Allergy and Clinical Immunology. 1995;95:955–961. doi: 10.1016/s0091-6749(95)70095-1. [DOI] [PubMed] [Google Scholar]
- Tchetgen Tchetgen EJ. Inverse odds ratio-weighted estimation for causal mediation analysis. Statistics in Medicine. 2014 doi: 10.1002/sim.5864. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan H, Ping L, Hai-chao L, Yue-dan W. The “time-window” effect of early allergen exposure on a rat asthma model. Chinese Medical Journal. 2013;126:2265–2269. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


