Figure 1.
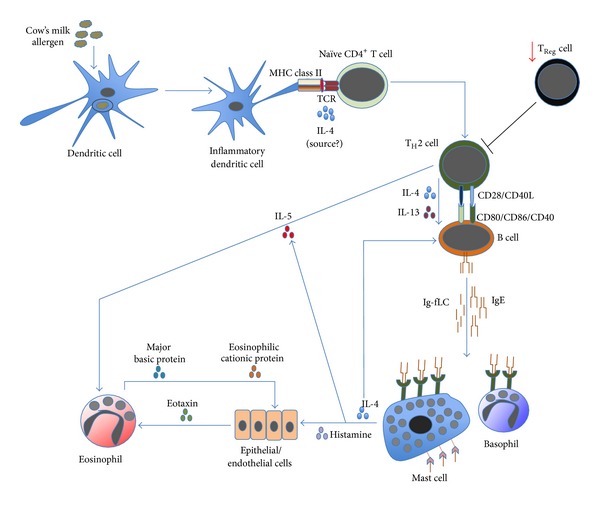
The cascade of allergic inflammation. Allergen's exposure to inflammatory DCs allows these cells to process and to present allergen-derived peptides to naïve CD4+ T cells. In the presence of IL-4 (from an unknown source), naïve CD4+ T cells differentiate into proallergic TH2 cells. Concurrently, it appears that there is an impairment of TReg-cell frequency and/or activity; hence, no suppression is exerted on TH2-cell activity. Subsequently, TH2 cells will drive B cells, via cell contact as well as IL-4 and IL-13, to undergo immunoglobulin class-switch recombination, in which they eventually produce IgE. Along with the antibody production, B cells also secrete significant amount of κ and λ Ig-free light chains (Ig-fLCs). IgE and Ig-fLCs will then bind to mast cells and basophils, causing sensitization (not shown). Following subsequent exposure to allergen, cross-linking of surface-bound antibodies occurs (not shown), causing mast cells and basophils to degranulate and release their biologically active substances, including histamine, IL-4, and IL-5. Released IL-4 amplifies the differentiation of TH2 and IgE-producing B cells, while released IL-5, also secreted by TH2 cells, causes accumulation and activation of eosinophils in the affected tissues. Similarly, histamine activates epithelial or endothelial cells to release eotaxin that also attracts eosinophils into the tissues. Activated eosinophils release active substances, including major basic and eosinophilic cationic proteins that are toxic to the surrounding cells, contributing to further inflammation.
