Abstract Abstract
Standardization of the diagnostic routine for children with congenital heart disease associated with pulmonary arterial hypertension (PAH-CHD) is crucial, in particular since inappropriate assignment to repair of the cardiac lesions (e.g., surgical repair in patients with elevated pulmonary vascular resistance) may be detrimental and associated with poor outcomes. Thus, members of the Congenital Heart Disease and Pediatric Task Forces of the Pulmonary Vascular Research Institute decided to conduct a survey aimed at collecting expert opinion from different institutions in several countries, covering many aspects of the management of PAH-CHD, from clinical recognition to noninvasive and invasive diagnostic procedures and immediate postoperative support. In privileged communities, the vast majority of children with congenital cardiac shunts are now treated early in life, on the basis of noninvasive diagnostic evaluation, and have an uneventful postoperative course, with no residual PAH. However, a small percentage of patients (older at presentation, with extracardiac syndromes or absence of clinical features of increased pulmonary blood flow, thus suggesting elevated pulmonary vascular resistance) remain at a higher risk of complications and unfavorable outcomes. These patients need a more sophisticated diagnostic approach, including invasive procedures. The authors emphasize that decision making regarding operability is based not only on cardiac catheterization data but also on the complete diagnostic picture, which includes the clinical history, physical examination, and all aspects of noninvasive evaluation.
Keywords: congenital heart disease, pulmonary hypertension, cardiac catheterization, pediatric cardiac surgery, postoperative care
It is estimated that congenital heart disease/defects (CHD) occur in approximately 1% of live births. Currently, in privileged communities, patients with CHD undergo repair early in life (first days, weeks, or months), with the aim of reducing the long-term sequelae of their heart disease, especially pulmonary vascular disease. Anomalies involving communications between the cardiac chambers or the great arteries, in the absence of significant pulmonary stenosis, are associated with increased pulmonary blood flow and pressure, leading to progressive remodeling of pulmonary arteries and increased pulmonary vascular resistance (PVR). In some patients, PVR fails to decrease properly after birth, and a real picture of increased pulmonary blood flow is never observed (frequently seen in high-altitude patients). These are the pathophysiological scenarios of pulmonary arterial hypertension associated with CHD (PAH-CHD). Anomalies associated with pulmonary stenosis or atresia may also present with developmental abnormalities of the pulmonary vasculature, which constitute limitations for complete repair. The Panamá classification of pulmonary hypertension in children includes not only PAH-CHD but also “no-shunt” cardiovascular abnormalities (developmental and acquired) and all pediatric disorders that can affect the pulmonary circulation at all ages.1 The position of PAH-CHD among the pediatric etiologies of pulmonary hypertension may be appreciated in a recent report of a Dutch registry including 3,263 patients.2
Many patients with CHD have simple communications between the systemic and the pulmonary circulation (atrial and ventricular septal defects [ASDs and VSDs, respectively] or patent ductus arteriosus [PDA]). More than 90% of these patients are subjected to percutaneous or surgical repair early in life on the basis of simple, noninvasive diagnostic evaluation. In these instances, the clinical history, physical examination, chest X-ray, and echocardiographic analysis show features of a typical hyperkinetic pulmonary circulation associated with congestive heart failure, pulmonary congestion, and failure to thrive. However, an estimated 5%–10% of patients do not present with these features, even in the presence of large, unrestrictive communications.3 These patients generally are subjected to invasive diagnostic evaluation (cardiac catheterization) prior to surgery, and a PVR above 3 Wood units m2 is detected (PAH-CHD). Although all large, unrestrictive communications may be associated with PAH, early development of severe pulmonary vasculopathy is particularly frequent in certain anomalies, such as truncus arteriosus, transposition of the great arteries with a VSD, and complete atrioventricular septal defects. Nearly 100% of unoperated patients with these anomalies will develop PAH. In a similar way, unoperated patients with large, unrestrictive VSDs or ASDs are also at risk (>50% and ∼10% risk, respectively).4-9 In addition to the size and type of the defect (for example, posttricuspid vs. pretricuspid communications), late referral, the presence of associated extracardiac syndromes (especially Down syndrome), and the degree of obstruction to the pulmonary venous flow (particularly in complex anomalies) are important risk factors.10
In contrast to patients with congenital cardiac septal defects and a hyperkinetic pulmonary circulation, PAH-CHD patients are at a higher risk of serious postoperative complications, including right cardiac failure and death.11,12 Those who survive surgery remain at risk of persistent PAH, which is sometimes diagnosed years after repair. Thus, it is critically important to decide whether the patient may undergo repair of the defect with an acceptable operative and perioperative risk and little chance of developing pulmonary vascular disease in the long term. This is particularly important because outcomes (survival curves) are considerably worse for patients with postoperative PAH than for those who remain unoperated and develop the Eisenmenger syndrome.2,13 However, because as yet there is no consensus on which patients should be classified as PAH-CHD patients and because sophisticated diagnostic tools are not available in many cardiac centers throughout the world, individuals are still frequently assigned to repair of their lesions at a high risk of complications.
There is a dearth of evidence to support definite recommendations in this field. Yet most specialists would agree that in the present era, it is not reasonable to assign patients with high PVR levels to surgery. We therefore decided to conduct a survey aimed at collecting the opinion of experts in many different countries on the management of PAH-CHD. The objective was to define minimal requirements for safely assigning patients to repair of their lesions (particularly surgical repair).
Survey preparation and discussion
The survey consisted of 11 questions with multiple alternatives as answers. At the end of each question, a space was given for free comments and suggestions on the subject. The survey covered many aspects of the management of PAH-CHD, from clinical recognition to complete diagnosis and essential requirements for immediate postoperative support. The questions focused on the management of patients with biventricular hearts. Decision making concerning patients destined to follow a cavopulmonary surgical pathway was not discussed.
Thirty-one pediatric cardiologists and pulmonologists from 14 different countries participated and expressed their opinions. During the year 2012, the initial questionnaire containing the 11 questions was sent to the participants. The answers were collected and summarized and served as the basis for a plenary discussion that was held on January 23, 2013, in Istanbul, Turkey, during the 6th Workshops and Debates meeting of the Pulmonary Vascular Research Institute. Then a text was prepared and sent to the participants for final approval. The final revised work was finished on December 15, 2013.
Evidence and strength of recommendations
The following classes of recommendation and levels of evidence for efficacy are used in the different topics throughout the text. In each of the topics, the strength of recommendation and the level of evidence correspond to the conclusions and statements that appear in boldface in the text.
Classes of recommendation
-
Class I
Strong recommendation.
-
Class II
Conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of the treatment.
-
Class IIa
Weight of evidence/opinion is in favor of usefulness/efficacy.
-
Class IIb
Usefulness/efficacy is less well established by evidence/opinion.
-
Class IIa
Levels of evidence for efficacy
-
A
Data derived from multiple randomized clinical trials or meta-analyses.
-
B
Data derived from a single randomized clinical trial, multiple trials with heterogeneous results, or observational studies.
-
C
Consensus of opinion of the experts and/or small studies, retrospective studies, registries.
The general concept of PAH-CHD
There was general agreement that some patients with congenital communications between the systemic and pulmonary circulation need a more individualized approach in terms of diagnosis and care management, as they do not have the typical features of increased pulmonary blood flow, leading to the assumption that PVR is at least moderately elevated. With respect to the decision to operate, these patients (especially pediatric patients) are often referred to as “borderline.” However, there has not been a precise definition of “borderline,” in particular because most specialists claim that such a concept should not be based on hemodynamic criteria only. Indeed, no clear associations have been demonstrated between preoperative pulmonary hemodynamics (including the acute response to vasodilators) and outcomes. Therefore, it is difficult to define a specific level or levels of PVR that allow safe assignment to cardiac operation or preclude it.14 The current view is that even before hemodynamic data are obtained, it is possible to identify this patient subpopulation on the basis of age (above 1 or 2 years, depending on the cardiac anomaly), type of the defect (truncus arteriosus, atrioventricular septal defects, transposition of the great arteries with a VSD), presence of large, nonrestrictive communications, complex or associated anomalies (particularly involving pulmonary venous drainage), bidirectional shunting with periods of systemic oxygen desaturation, absence of congestive heart failure or failure to thrive, and presence of extracardiac syndromes (particularly Down syndrome). Patients presenting with combinations of these features very likely have inappropriate elevation of pulmonary artery pressure and vascular resistance and need individualized diagnostic evaluation for proper management. Baseline hemodynamics and the acute response to vasodilators are then taken into consideration as part of the whole diagnostic scenario. It should be noted, however, that the response to acute vasodilator testing has no proven prognostic implications in CHD with pulmonary hypertension, as established in the 5th World Symposium on Pulmonary Hypertension in Nice, France, in 2013. Finally, the limits of the therapeutic actions (and therefore the decision as to whether a given patient should be assigned to surgery) are largely dependent on local experience and expertise at different institutions.
Initial approach to the patient with PAH-CHD
This is an important point, as the answer defines which patients can be safely assigned to repair of their cardiac lesions on the basis of noninvasive diagnosis and which ones will need a more sophisticated evaluation. Most participants agreed that late presentation, absence of pulmonary congestion, presence of associated syndromes, posttricuspid localization of the communications, bidirectional shunting, systemic oxygen desaturation, and the presence of complex anomalies (especially those involving obstruction to pulmonary venous flow) are features to be considered to start thinking about PAH. Patients with none of these features are likely candidates for repair on the basis of simple, noninvasive evaluation. Those with some of these features will probably need a more sophisticated diagnostic approach, and those presenting with all these features will likely be considered as unsuitable for repair of cardiac defects, at least at the first moment. There were suggestions in favor of including specific anomalies as risk factors (e.g., truncus arteriosus and transposition of the great arteries with a VSD). In addition, a loud second heart sound (pulmonic component) and the absence of murmur in posttricuspid communications should be looked on as indicative of elevated PVR, as should the complete absence of a dynamic precordium. Finally, with regard to the initial screening echocardiogram, in addition to the direction of flow across the communications (bidirectional flow indicative of elevated pulmonary artery pressure), the size of the left cardiac chambers helps in determining the magnitude of pulmonary blood flow in simple posttricuspid defects. Patients less than 2 years of age with an ASD, VSD, or PDA with normal oxygen saturations and signs of pulmonary over circulation, and only left-to-right shunting by echocardiography may undergo surgical repair without invasive hemodynamic evaluation. Strength of recommendation I; level of evidence C.
Assessment of oxygen saturation
Measurement of systemic oxygen saturation is a crucial diagnostic step in the evaluation of patients with CHD in general, particularly those suspected of having PAH-CHD.15-18 By adequately measuring systemic oxygen saturation, one can have an indirect idea of the magnitude of pulmonary blood flow (and therefore PVR). Even in cyanotic congenital cardiac defects, systemic oxygen saturation may be only mildly decreased if pulmonary flow is substantially increased. For example, oxygen saturation levels in the range of 85%–90% may be observed in patients with (1) transposition of the great arteries with large ASD and VSD or (2) double-outlet right ventricle in the absence of pulmonary stenosis or severe pulmonary vascular disease. Pulmonary blood flow and oxygen saturation progressively decrease as pulmonary vasculopathy advances. However, increased systemic oxygen saturation may occur with streaming or obligate shunts (e.g., left ventricle to right atrium) that are independent of the PVR and may result in erroneous clinical underestimation of this parameter.
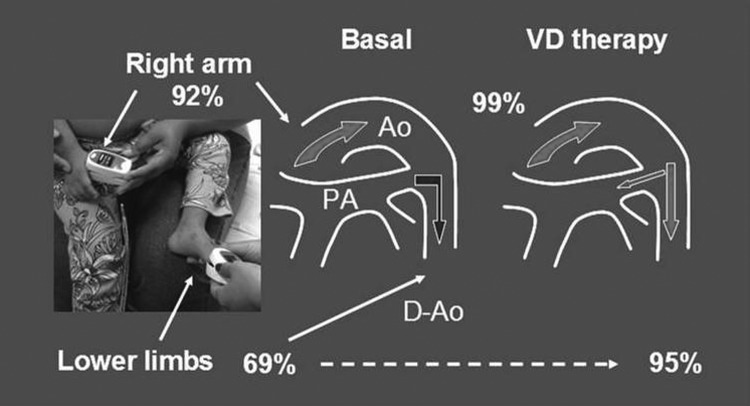
In acyanotic defects, systemic arterial oxygen saturation is expected to be >93%. Patients with moderate to severe pulmonary vasculopathy may have normal oxygen saturation at rest but decreased levels on exertion (young patients may become desaturated during feeding, for example). Bidirectional shunting across a PDA may be associated with a saturation gradient between the right arm and lower limbs, because of the presence of desaturated blood in the descending aorta (Fig. 1). Levels in lower extremities may be further decreased by physical activity. Therefore, during the 6-minute walk test in older children, adolescents, and adults, measurements in upper and lower extremities are mandatory at rest and peak exercise. The resting gradient may also increase transiently during episodes of pulmonary vasoconstriction (young children with dynamic PVR).
Figure 1.
Comparative pulse oximetry in the right arm and lower extremities in a young (2-year-old) patient with patent ductus arteriosus associated with pulmonary arterial hypertension. At baseline, heightened pulmonary vascular resistance causes right-to-left shunting from pulmonary arteries (PA) to the descending aorta (D-Ao), with decreased oxygen saturation in lower extremities compared to that in the ascending aorta (Ao) and the right arm. Successful pulmonary vasodilator therapy (VD therapy) is followed by a decrease in oxygen saturation gradient between the right arm and the lower limbs, indicating a change in the direction of flow across the ductus, from predominantly right-to-left to predominantly left-to-right. Such a response is unlikely to occur in older patients with patent ducts and right-to-left shunting due to pulmonary hypertension.
In the absence of respiratory or neurological disorders, decreased systemic oxygen saturation in patients with congenital cardiac septal defects (for example, oxygen saturation < 93% in acyanotic defects) is strongly suggestive of increased PVR associated with bidirectional shunting. In most instances, extensive and individualized diagnostic evaluation becomes necessary before assignment to surgery.
On the basis of these assumptions, the survey participants would like to recommend the following policies for an adequate assessment of systemic oxygen saturation and interpretation of possible abnormalities: (1) take careful and repeated measurements; (2) make comparisons between upper and lower extremities; (3) if possible, take measurements both at rest and on exertion (according to age); (4) consider the type of the cardiac anomaly; (5) take into account all other causes of systemic oxygen desaturation; (6) consider the altitude at which the evaluation is undertaken; and (7) differential oxygen saturation (lower extremity with saturations lower than the upper extremity) or desaturation with exercise mandates the need for invasive hemodynamic evaluation before consideration of complete surgical or catheter repair. Strength of recommendation I; level of evidence C.
Diagnostic testing in patients suspected of having PAH-CHD
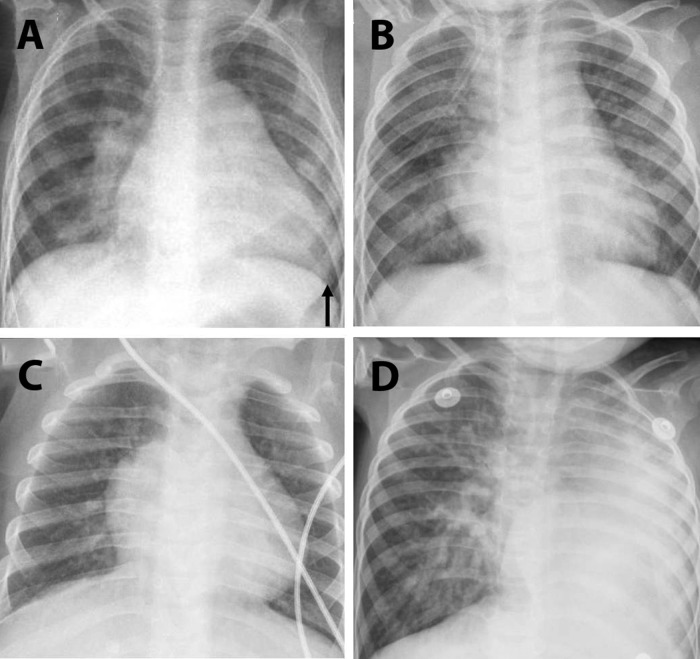
In order to adequately define the anatomy of heart defects, the overall cardiac function, and the status of the cardiopulmonary circulation, a number of diagnostic procedures/studies are required.19 Depending on the complexity of cardiovascular abnormalities, a simple or a more sophisticated diagnostic approach is considered (Table 1). However, a complete diagnostic evaluation may be unrealistic in terms of a global perspective and probably involves a high cost∶benefit ratio in many instances. Therefore, in terms of noninvasive cardiovascular evaluation in patients suspected of having PAH-CHD, an electrocardiogram, a chest X-ray (Fig. 2), and a transthoracic echocardiogram were considered by the task force members as essential and necessary in all instances. Table 2 summarizes parameters obtained during echocardiographic evaluation that have been shown to correlate with catheterization data in patients with congenital systemic-to-pulmonary shunts.20-24 Indirect observations that suggest a “high-flow/low-resistance” state of the pulmonary circulation are the pressure gradient across the defect (except for large, unrestrictive defects where the pressure is the same on both sides independently of the PVR) and the size of the left cardiac chambers. However, left atrial or ventricular dilation and pulmonary congestion due to increased pulmonary blood flow must be differentiated from atrioventricular (e.g., atrioventricular canal defect) or truncal valve regurgitation.
Table 1.
Noninvasive diagnostic workup in PAH-CHD
| Electrocardiograma |
| Chest X-raya |
| Echocardiogram |
| Transthoracica |
| Transesophagealb |
| Computed tomography angiographyb |
| Cardiac magnetic resonance imagingb |
| Nuclear perfusion scan for Qp∶Qs estimationb |
| Chest computed tomography (parenchymal lung disease)b |
| Bronchoscopyb |
| Blood work/serology |
| Red blood cell count, hematocrit, hemoglobin level, mean corpuscular volumea |
| Iron storesc |
| Screening for respiratory syncytial virus and other virusesd |
PAH-CHD: pulmonary arterial hypertension associated with congenital heart disease; Qp∶Qs: ratio of pulmonary to systemic blood flow.
Mandatory (all patients).
In select cases.
May be helpful in cyanotic patients with increased hematocrit, as iron depletion is associated with increased blood viscosity.
Although patients below the age of 2 years with cardiovascular disorders are particularly susceptible to viral infections (respiratory syncytial virus, adenovirus, and other aggressive agents), which may be associated with severe, life-threatening perioperative complications, the task force members acknowledge that specific diagnostic tests may be unavailable in many places.
Figure 2.
Chest X-rays in patients with systemic-to-pulmonary shunts. A, Marked cardiomegaly (arrow, enlarged left ventricle) with pulmonary congestion in a 2.6-year-old girl with atrioventricular septal defect and markedly increased pulmonary blood flow (pulmonary-to-systemic blood flow ratio [Qp∶Qs] of 4.0∶1). B, Moderately enlarged heart in a 14-month-old boy with patent ductus arteriosus and a small atrial septal defect (Qp∶Qs of 1.4∶1, no clinical features of pulmonary congestion). C, Enlarged but hypertrophic heart without pulmonary congestion in a 2-year-old girl with Down syndrome, large patent ductus arteriosus, and a small ventricular septal defect (Qp∶Qs of 1.4∶1). D, Increased vascular markings in the right lung in a 1.7-year-old boy with hypoplastic left lung and ventricular septal defect (Qp∶Qs of 1.8∶1, corresponding essentially to right-sided pulmonary blood flow).
Table 2.
Echocardiographic parameters that correlate with pulmonary hemodynamics in patients with congenital cardiac shunts
| Echocardiographic parameters | Increased PVR | Low PVR, increased Qp | ||
|---|---|---|---|---|
| Likely | Certainly | Likely | Certainly | |
| TRV, m/s | >2.5 | >3.7 | ||
| TRV/VTIRVOT | >0.11 | >0.20 | ||
| PAPsys/VTIRVOT | >1.91 | >1.94 | ||
| PAPsys/(VTIRVOT × HR) | >0.0095 | >0.025 | ||
| Qp∶Qs | <2.1 | <1.3 | >2.9 | >4.0 |
| MPIRV | >0.48 | >0.55 | ||
| VTIRVOT, cm | >22 | >27 | ||
| VTIPV, cm | >20 | >24 | ||
Based on references 20–24. PVR: pulmonary vascular resistance; Qp: pulmonary blood flow; TRV: tricuspid regurgitation velocity; VTIPV and VTIRVOT: respectively, velocity time integral in pulmonary veins and in right ventricular outflow tract; PAPsys: systolic pulmonary arterial pressure; HR: heart rate; Qp∶Qs: pulmonary-to-systemic blood flow ratio; MPIRV: right ventricular myocardial performance index.
Even patients with favorable hemodynamics associated with simple cardiac defects may require further diagnostic tests. For example, patients with increased pulmonary blood flow (e.g., a pulmonary-to-systemic blood flow ratio [Qp∶Qs] in the vicinity of 3.0∶1) may not have normalization of the PVR following successful cardiac repair if lung disease is present pre- and postoperatively.25 Furthermore, respiratory disorders are associated with an increased risk of serious postoperative complications. Thus, extended diagnostic evaluation, which includes high-resolution chest computed tomography for parenchymal lung disease, becomes necessary in expremature infants, patients with bronchopulmonary dysplasia, and selected patients with Down syndrome and other developmental or acquired disorders. Strength of recommendation I; level of evidence C.
Cardiac catheterization: policies for obtaining accurate data
We did not reach a consensus as to whether echocardiography alone without cardiac catheterization is sufficient to assign children to surgery if they have clinical features suggestive of increased PVR. Cardiac catheterization is a complicated diagnostic procedure, especially in young patients, with many potential sources of measurement errors.26,27 Measurements have to be made under stable and reproducible clinical conditions and in young children usually require either sedation or general anesthesia. In patients with systemic-to-pulmonary shunts, blood flow cannot be measured by thermodilution and is calculated using the Fick principle. Accurate blood flow measurements require a direct measurement of oxygen consumption, which is unavailable in many institutions. Ideally, the acute pulmonary vasodilator test should be performed with inhaled nitric oxide as the vasodilator stimulus. However, inhaled nitric oxide is relatively expensive and is unavailable in many institutions, including some tertiary centers. In these instances, it is acceptable to perform tests with prostacyclin analogs (iloprost, for example), intravenous sildenafil (if available), or oxygen at high concentrations (not the preferable method if the Fick principle is being considered for measurement of Qp and Qs).
In order to maximize the usefulness of the data obtained with cardiac catheterization, the following may be of value: (1) adequate discussion of the goals of the cardiac catheterization with involved professionals (including pediatric cardiologists, interventionists, cardiac surgeons, anesthesiologists, and nurses); (2) consideration of discontinuing, whenever possible, diuretics and systemic vasodilators prior to catheterization in order to avoid systemic hypotension; (3) ensuring that the hemoglobin level is adequate; (4) judicious use of sedatives and anesthetic drugs, avoiding in particular premade drug cocktails, bolus administration, and myocardial depressants; (5) maintaining stable hemodynamic, respiratory, and metabolic conditions during the procedure; (6) continuous monitoring of pulse oximetry and end-tidal CO2 with intermittent blood gas analysis, especially for pH; (7) well-functioning, optimally damped, and accurately zeroed pressure transducers; (8) retrograde catheterization is preferable; (9) blood samples for gas analyses (using the Fick principle to calculate flow) must be processed promptly; (10) if measured oxygen consumption is not available, it is preferable to rely on the Qp∶Qs and the vascular resistance ratio (PVR∶systemic vascular resistance [SVR]) rather than the absolute values of these parameters. Strength of recommendation I; level of evidence C.
How to interpret and use cardiac catheterization data
Three important issues must be considered regarding the interpretation and use of cardiac catheterization data in clinical practice. First, a PVR measurement that absolutely contraindicates surgery in PAH-CHD has not been established. Until recently, it was considered reasonable to “think about corrective surgery” for young patients with a PVR of <6 Wood units m2 (PVR∶SVR < 0.3). Second, the acute pulmonary vasodilator test has not been shown to predict outcome.11 Despite that, most colleagues would argue in favor of performing the test, because they believe that it is important to determine whether PVR is fixed or dynamic in individual cases. Third, there is a general agreement that hemodynamics and the results of acute vasodilator testing should be considered in the context of the clinical history, physical examination, and noninvasive diagnostic evaluation.
The use of a PVR of 6 Wood units m2 and a PVR∶SVR ratio of 0.3 as limits for considering operation in PAH-CHD was proposed in a previously published consensus28 and extensively discussed subsequently.29 A 20% decrease in PVR from baseline during the acute vasodilator test was considered sufficient to define a positive response but not to characterize operability. More recently, during the 5th World Symposium on Pulmonary Hypertension of the World Health Organization (Nice, France, February 2013), a PVR of 4 Wood units m2 was proposed as a limit for considering surgery, and a PVR of 4–8 Wood units m2 as the range in which patients should be discussed case by case. The Pediatric Task Force also concluded that at present, there is no established protocol for the vasodilator test in children and no evidence to use it for prognostic purposes.
There has been debate about what to do with patients with elevated PVR (e.g., PVR > 8–10 Wood units m2 and PVR∶SVR > 0.5), in particular since the answer will not be the same for patients at different ages. Furthermore, prospective studies involving large patient populations (children and adults analyzed separately) and long-term follow-up are not available. Some participants in the present survey would have a more flexible position if the PVR decreases to levels in the range of 4–6 Wood units m2 during the vasodilator challenge. Other participants, however, would feel uncomfortable with high PVR levels, regardless of the magnitude of the vasodilator response. Until further literature data become available, these situations will remain a matter of discussion on a very individual basis. The whole diagnostic scenario (not only cardiac catheterization data) and the local expertise at different institutions are important issues to be taken into consideration. Strength of recommendation IIa; level of evidence B.
What if catheterization is not available? Should patients be assigned to pulmonary arterial banding?
If cardiac catheterization is unavailable, most members of the task forces suggested referral of patients to another center or institution where the procedure can be done. However, there is general agreement that referral may be difficult or even impossible in certain areas of developing countries. Alternative solutions have been proposed when catheterization is not available as a diagnostic method and there are reasons to suspect that PVR is at least moderately elevated: (1) partial closure of the communication; (2) leaving a small ASD open while repairing posttricuspid defects; (3) placing a band on the pulmonary artery.
Decades ago, uncontrolled observations suggested that “plexogenic pulmonary arteriopathy,” by which was meant cellular intimal proliferation, could be reversed following pulmonary artery banding in patients with CHD.30 However, the small number of treated patients, the lack of complete catheterization data, and the variable time between banding and repair of the cardiac lesions (time between the two lung biopsies) constitute major limitations and make it difficult to make conclusions about the efficacy of the procedure. More recently, experimental animal data suggested that hemodynamic unloading of lungs with pulmonary vascular disease may induce progressive normalization of pulmonary artery structure.31
Until data from controlled studies in humans are available indicating that “reverse remodeling” of pulmonary arteries does occur following hemodynamic unloading of the lungs, the consensus is that pulmonary artery banding should not be used routinely in patients with elevated PVR. Thus, the general opinion recommended pulmonary artery banding to protect the pulmonary vasculature if there is increased pulmonary blood flow and corrective surgery is impossible. On the other hand, there are data to suggest that two-stage repair is accompanied by increased mortality in both developed and developing countries.32 Strength of recommendation IIa; level of evidence C.
Role of lung biopsy
Since the publication by Heath and Edwards33 in 1958 of a comprehensive classification of pulmonary vascular lesions in CHD, many investigators have looked at specimens obtained at autopsy or via lung biopsy (preoperative or intraoperative) for further understanding of the characteristics of vascular remodeling that occur in this disorder. This huge amount of information served as a basis for a better understanding of lung development under the abnormal conditions of CHD, provided us with data of prognostic significance, and added important contributions to current knowledge of vascular abnormalities that occur in PAH.34-37
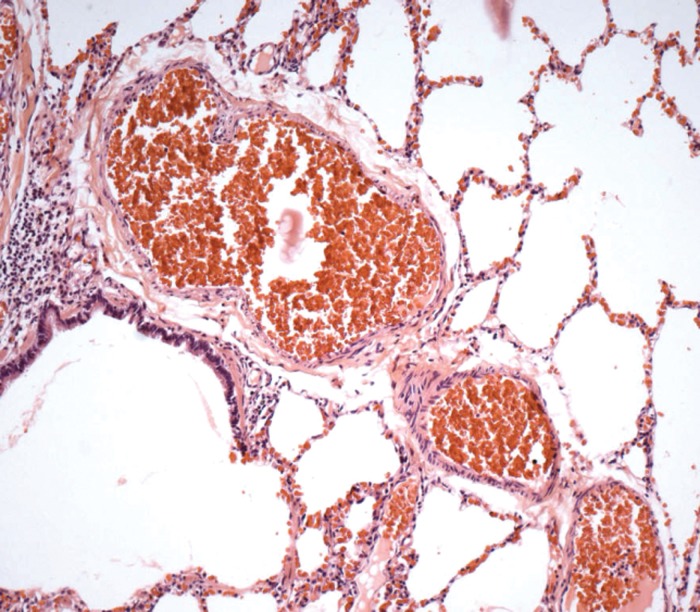
With continuous advances in noninvasive diagnosis (essentially echocardiography) and cardiac catheterization in young pediatric patients, lung biopsy for diagnostic and prognostic purposes became less usual. On the other hand, the argument that findings of biopsy specimens are not representative of the whole lung probably does not hold, as the interpretation of the observations depends largely on the quality of the collected tissue and the expertise of the pathologist (Fig. 3).38 Assessment of pulmonary vascular abnormalities by lung biopsy remains important in specific conditions, including cardiac shunts in the presence of unilateral lung hypoplasia, unilateral pulmonary arterial stenosis, systemic blood flow supply to the lungs, and suspicion of veno-occlusive disease or pulmonary vein stenosis. Thus, the current view is that in PAH-CHD, lung biopsy is not recommended routinely as part of diagnostic investigation. However, lung biopsy (preoperative or intraoperative) may provide helpful information in selected cases and may be considered for research purposes. Strength of recommendation IIa; level of evidence B.
Figure 3.
Photomicrograph of a lung biopsy taken intraoperatively from a 3-year-old patient with ventricular septal defect. Note the presence of thin-walled arteries at the entrance of the pulmonary acinus. This could lead to the interpretation that there is no structural pulmonary vascular disease. However, to the experienced pathologist, the apparent discrepancy between clinical and morphological data and the knowledge that distal dilatation occurs in severe pulmonary vascular disease indicate that a search for obstructive lesions is mandatory. In the case illustrated here, a plexiform lesion was found in another level of the same lung specimen, after semiseriated sections. Hematoxylin-eosin stain, objective magnification ×10. Photograph courtesy of Vera D. Aiello, Heart Institute, University of São Paulo, Brazil. Reproduced from reference 38, with permission.
Immediate postoperative care
Successful management of PAH-CHD patients who do undergo surgery also depends on the availability of expert perioperative care. Pulmonary hypertensive crisis (PHC) is a life-threatening hemodynamic disturbance associated with prolonged intensive care unit stay and significant mortality. It is different from simple, transient elevation of pulmonary artery pressure. Although one might consider PHC a typical postcardiopulmonary bypass complication, actually it may occur even following simple interventions (e.g., pulmonary artery banding). In the current era, the overall incidence of PHC following pediatric cardiac surgery is low (∼1%), but once a typical crisis is in course, the likelihood of a fatal outcome is high.39 Furthermore, there is no preoperative PVR that effectively predicts the occurrence of postoperative PHC. It should be emphasized, however, that this low incidence of PHC is reported for tertiary centers in developed countries, where inhaled nitric oxide and all other postoperative facilities are available, with prompt assistance at any remote suggestion of trouble. The incidence is expected to be considerably higher in areas where these tools are not available. Patients particularly at risk are those older at surgical treatment, those with a high degree of pulmonary vasoreactivity, those with an extracardiac syndrome, and those with an elevated pulmonary venous or left atrial pressure.40
In terms of postoperative management, the consensus was against the routine prophylactic use of pulmonary artery catheters and treatment with pulmonary vasodilators. However, a systemic arterial line (catheter) and central venous access are essential. Judicious use of pulmonary artery catheters maybe of value in individual cases. Recommended postoperative management includes avoiding the triggers of PHC. These include avoiding low cardiac output syndrome (with milrinone and low-dose epinephrine), hypoxia, and acidosis; adequate sedation with narcotics; and optimizing ventilation. Muscle relaxation may be indicated. Treatment of impeding or established PHC includes administration of inhaled nitric oxide, inhaled prostacyclin or analogs, moderate alkalosis, sedation, and muscle relaxation. A randomized controlled trial showed that the phosphodiesterase type 5 inhibitor sildenafil prevents rebound pulmonary hypertension after withdrawal of nitric oxide in children and reduces mechanical ventilation time and length of stay in the intensive care unit.41 Any child experiencing symptomatic postoperative pulmonary or right ventricular hypertension requires a thorough evaluation to exclude hemodynamically important residual or unappreciated cardiac lesions. Strength of recommendation IIa; level of evidence C.
Conclusion
Early repair of congenital cardiac lesions with improved postoperative care is the best strategy to prevent the development of severe pulmonary vasculopathy in CHD. However, even in developed nations, some infants/children are older at presentation or have yet-undiscovered genetic abnormalities that predispose to increased pulmonary vasoreactivity or early development of pulmonary vascular remodeling. The decision to operate on these patients with an acceptable risk of early and late postoperative complications is not easy, and the current view is that it should be not be based on single parameters. The consensus is that safe assignment to surgery in PAH-CHD should be based on “the full picture,” that is, a stepwise analysis of a series of clinical, noninvasive, and eventually invasive diagnostic procedures (summarized in Table 3). Hopefully, in the future, biological markers of prognosis (based on increased knowledge in terms of cellular biology, proteomics, and genomics) will be available for use in practice. Until then, careful analysis of multiple parameters on a very individual basis seems to be the best policy. Also, long-term postoperative follow-up is required, as residual (persistent) PAH may become evident years after surgery in some cases.
Table 3.
Recommended preoperative evaluation of pediatric patients with congenital systemic-to-pulmonary shunts, with the findings that may indicate a favorable or unfavorable response to correction of cardiac lesions
| Findings | ||
|---|---|---|
| Source, features/parameters | Favorable | Unfavorable |
| Clinical history | ||
| Age, years | <1 | >2 |
| Congestive heart failure/pulmonary congestion | Present | Absent |
| Tendency to respiratory disorders (inflammatory/infectious) | Yes | No |
| Failure to thrive | Yes | No |
| Use of anticongestive medication | Yes | No |
| Associated syndromes | No | Yes (Down syndrome) |
| Associated airway/lung disease | No | Yes |
| Physical examination | ||
| Dyspnea | Present/overt | Mild/absent |
| Dynamic precordium | Present | Absent |
| Precordial murmur | Present | Absent |
| Second heart sound (pulmonic area) | Mildly increased split present | Loud split absent |
| Peripheral oxygen saturation, % | >93 | <90 |
| Associated airway obstruction/lung disease | No | Yes |
| Chest X-ray | ||
| Size of the heart | Enlarged | “Hypertrophic” |
| Pulmonary vascular markings | Proeminent | Decreased distal markings |
| Congestion | Present | Absent |
| Parenchymal lung disease | Absent | Present |
| Transthoracic echocardiography | ||
| Direction of flow across the communication | Left-to-right or bidirectional, but predominantly left-to-right | Bidirectional, predominantly right-to-left |
| Size of left cardiac chambers (posttricuspid shunts) | Enlarged | Not enlarged |
| Pulmonary-to-systemic blood flow ratio (Qp∶Qs) | >3.0∶1 | >2.0∶1 |
| Right ventricular dysfunction | Absent | Present |
| Type of defectsa | Simple lesionsb | Complex anomaliesc |
| Cardiac catheterization | ||
| Pulmonary vascular resistance index, Wood units m2 | <6.0 (preferably, <4.0) | >8.0 |
| Pulmonary-to-systemic vascular resistance ratio (PVR∶SVR) | <0.3 | >0.5 |
Only biventricular physiology is considered.
Atrial and ventricular septal defects, patent ductus arteriosus (single or combined lesions). Total atrioventricular septal defects (cushion defects) may be considered moderately complex lesions (especially when associated with Down syndrome), particularly if full repair of the atrioventricular valve is unlikely to be possible and residual dysfunction is expected.
Transposition of the great arteries, especially when associated with a ventricular septal defect; persistent truncus arteriosus (particularly in older infants); systemic origin of pulmonary arteries; unilaterally stenotic or hypoplastic pulmonary arteries associated with intracardiac shunts; obstruction to the pulmonary venous flow; systemic-to-pulmonary shunts complicated by pulmonary vein stenosis; obstructed anomalous pulmonary venous drainage.
Acknowledgments
We express our gratitude to Pulmonary Circulation for permitting the reproduction of Figure 3 (corresponding to Fig. 1 of the original article).38
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Lammers AE, Adatia I, del Cerro MJ, Freudenthal AH, Freudenthal F, Harikrishnan S, Haworth SG, et al. Functional classification of pulmonary hypertension in children: report from the PVRI pediatric taskforce, Panama 2011. Pulm Circ 2011;1:280–285. [DOI] [PMC free article] [PubMed]
- 2.van Loon RL, Roofthooft MT, Hillege HL, ten Harkel ADJ, van Osch-Gevers M, Delhaas T, Kapusta L, et al. Pediatric pulmonary hypertension in the Netherlands: epidemiology and characterization during the period 1991 to 2005. Circulation 2011;124:1755–1764. [DOI] [PubMed]
- 3.Galiè N, Torbicki A, Barst R, Dartevelle P, Haworth S, Higenbottam T, Olschewski H, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension: the Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J 2004;25:2243–2278. [DOI] [PubMed]
- 4.Engelfriet PM, Duffels MG, Möller T, Boersma E, Tijssen JGP, Thaulow E, Gatzoulis MA, Mulder BJM. Pulmonary arterial hypertension in adults born with a heart septal defect: the Euro Heart Survey on adult congenital heart disease. Heart 2007;93:682–687. [DOI] [PMC free article] [PubMed]
- 5.Saha A, Balakrishnan KG, Jaiswal PK, Venkitachalam CG, Tharakan J, Titus T, Kutty R. Prognosis for patients with Eisenmenger syndrome of various aetiology. Int J Cardiol 1994;45:199–207. [DOI] [PubMed]
- 6.Vongpatanasin W, Brickner ME, Hillis LD, Lange RA. The Eisenmenger syndrome in adults. Ann Intern Med 1998;128:745–755. [DOI] [PubMed]
- 7.Steele PM, Fuster V, Cohen M, Ritter DG, McGoon DC. Isolated atrial septal defect with pulmonary vascular obstructive disease: long-term follow-up and prediction of outcome after surgical correction. Circulation 1987;76:1037–1042. [DOI] [PubMed]
- 8.Vogel M, Berger F, Kramer A, Alexi-Meshkishvili V, Lange PE. Incidence of secondary pulmonary hypertension in adults with atrial septal or sinus venosus defects. Heart 1999;82:30–33. [DOI] [PMC free article] [PubMed]
- 9.Simonneau G, Robbins IM, Beghetti M, Channick RN, Delcroix M, Denton CP, Elliott CG, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2009;54(Suppl.):S43–S54. [DOI] [PubMed]
- 10.Lopes AA. Pre-operative pulmonary hypertension in congenital heart disease and aspects of Eisenmenger’s syndrome in children. In: Beghetti M, ed. Pediatric pulmonary hypertension. Munich: Elsevier Urban & Fischer, 2011:187–207.
- 11.Balzer DT, Kort HW, Day RW, Corneli HM, Kovalchin JP, Cannon BC, Kaine SF, et al. Inhaled nitric oxide as a preoperative test (INOP Test I): the INOP Test Study Group. Circulation 2002;106:I76–I81. [PubMed]
- 12.Kannan BR, Sivasankaran S, Tharakan JA, Titus T, Kumar VKA, Francis B, Krishnamoorthy KM, Harikrishnan S, Padmakumar R, Nair K. Long-term outcome of patients operated for large ventricular septal defects with increased pulmonary vascular resistance. Indian Heart J 2003;55:161–166. [PubMed]
- 13.Haworth SG, Hislop AA. Treatment and survival in children with pulmonary arterial hypertension: the UK Pulmonary Hypertension Service for Children 2001–2006. Heart 2009;95:312–317. [DOI] [PubMed]
- 14.Giglia TM, Humpl T. Preoperative pulmonary hemodynamics and assessment of operability: is there a pulmonary vascular resistance that precludes cardiac operation? Pediatr Crit Care Med 2010;11(Suppl.):S57–S69. [DOI] [PubMed]
- 15.DeNicola LK, Kissoon N, Abram HS, Sullivan KJ, Delgado-Corcoran C, Taylor C. Noninvasive monitoring in the pediatric intensive care unit. Pediatr Clin North Am 2001;48:573–588. [DOI] [PubMed]
- 16.van Loon RL, Hoendermis ES, Duffels MG, Vonk-Noordegraaf A, Mulder BJM, Hillege HL, Berger RMF. Long-term effect of bosentan in adults versus children with pulmonary arterial hypertension associated with systemic-to-pulmonary shunt: does the beneficial effect persist? Am Heart J 2007;154:776–782. [DOI] [PubMed]
- 17.Limsuwan A, Wanitkul S, Khosithset A, Attanavanich S, Samankatiwat P. Aerosolized iloprost for postoperative pulmonary hypertensive crisis in children with congenital heart disease. Int J Cardiol 2008;129:333–338. [DOI] [PubMed]
- 18.Bergstra A, Hoendermis ES, Talsma MD, Mook GA, Zijlstra WG, Berger RM. Pulse densitometer indocyanine green dilution curves: a simple applicable and accurate method for determination of cardiac shunts. Congenital Heart Dis 2009;4:362–368. [DOI] [PubMed]
- 19.Suesaowalak M, Cleary JP, Chang AC. Advances in diagnosis and treatment of pulmonary arterial hypertension in neonates and children with congenital heart disease. World J Pediatr 2010;6:13–31. [DOI] [PubMed]
- 20.Ajami GH, Cheriki S, Amoozgar H, Borzouee M, Soltani M. Accuracy of Doppler-derived estimation of pulmonary vascular resistance in congenital heart disease: an index of operability. Pediatr Cardiol 2011;32:1168–1174. [DOI] [PubMed]
- 21.Cevik A, Kula S, Olgunturk R, Tunaoglu FS, Oguz AD, Pektas A, Saylan B. Quantitative evaluation of right ventricle function by transthoracic echocardiography in childhood congenital heart disease patients with pulmonary hypertension. Echocardiography 2012;29:840–848. [DOI] [PubMed]
- 22.de Sa Ribeiro ZV, Tsutsui JM, Miranda RdA, Mohry S, Mathias W, Lopes AA. Doppler echocardiography and hemodynamic parameters in congenital heart disease with increased pulmonary flow. Arq Bras Cardiol 2010;94:592–600. [DOI] [PubMed]
- 23.Alkon J, Humpl T, Manlhiot C, McCrindle BW, Reyes JT, Friedberg MK. Usefulness of the right ventricular systolic to diastolic duration ratio to predict functional capacity and survival in children with pulmonary arterial hypertension. Am J Cardiol 2010;106:430–436. [DOI] [PubMed]
- 24.Dyer KL, Pauliks LB, Das B, Shandas R, Ivy D, Shaffer SM, Valdes-Cruz, LM. Use of myocardial performance index in pediatric patients with idiopathic pulmonary arterial hypertension. J Am Soc Echocardiogr 2006;19:21–27. [DOI] [PMC free article] [PubMed]
- 25.Feinstein JA. Evaluation, risk stratification, and management of pulmonary hypertension in patients with congenital heart disease. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2009:106–111. [DOI] [PubMed]
- 26.Berger RM. Possibilities and impossibilities in the evaluation of pulmonary vascular disease in congenital heart defects. Eur Heart J 2000;21:17–27. [DOI] [PubMed]
- 27.Wilkinson JL. Haemodynamic calculations in the catheter laboratory. Heart 2001;85:113–120. [DOI] [PMC free article] [PubMed]
- 28.Lopes AA, Rabinovitch M, eds. Statements on the management of pulmonary hypertension associated with congenital heart disease. Cardiol Young 2009(Suppl. S1):1–53.
- 29.Beghetti M, Galiè N, Bonnet D. Can “inoperable” congenital heart defects become operable in patients with pulmonary arterial hypertension? dream or reality? Congenital Heart Dis 2012;7:3–11. [DOI] [PubMed]
- 30.Wagenvoort CA, Wagenvoort N, Draulans-Noë Y. Reversibility of plexogenic pulmonary arteriopathy following banding of the pulmonary artery. J Thorac Cardiovasc Surg 1984;87:876–886. [PubMed]
- 31.O’Blenes SB, Fischer S, McIntyre B, Keshavjee S, Rabinovitch M. Hemodynamic unloading leads to regression of pulmonary vascular disease in rats. J Thorac Cardiovasc Surg 2001;121:279–289. [DOI] [PubMed]
- 32.Brooks A, Geldenhuys A, Zuhlke L, Human P, Zilla P. Pulmonary artery banding: still a valuable option in developing countries? Eur J Cardiothorac Surg 2012;41:272–276. [DOI] [PubMed]
- 33.Heath D, Edwards JE. The pathology of hypertensive pulmonary vascular disease; a description of six grades of structural changes in the pulmonary arteries with special reference to congenital cardiac septal defects. Circulation 1958;18:533–547. [DOI] [PubMed]
- 34.Meyrick B, Reid L. Ultrastructural findings in lung biopsy material from children with congenital heart defects. Am J Pathol 1980;101:527–542. [PMC free article] [PubMed]
- 35.Rabinovitch M, Haworth SG, Castaneda AR, Nadas AS, Reid LM. Lung biopsy in congenital heart disease: a morphometric approach to pulmonary vascular disease. Circulation 1978;58:1107–1122. [DOI] [PubMed]
- 36.Rabinovitch M, Keane JF, Norwood WI, Castaneda AR, Reid L. Vascular structure in lung tissue obtained at biopsy correlated with pulmonary hemodynamic findings after repair of congenital heart defects. Circulation 1984;69:655–667. [DOI] [PubMed]
- 37.Haworth SG. Pulmonary vascular disease in different types of congenital heart disease: implications for interpretation of lung biopsy findings in early childhood. Br Heart J 1984;52:557–571. [DOI] [PMC free article] [PubMed]
- 38.Lopes AA. Is surgical treatment the cure for patients with congenital heart disease? Pulm Circ 2012;2:273–274. [DOI] [PMC free article] [PubMed]
- 39.Lindberg L, Olsson AK, Jögi P, Jonmarker C. How common is severe pulmonary hypertension after pediatric cardiac surgery? J Thorac Cardiovasc Surg 2002;123:1155–1163. [DOI] [PubMed]
- 40.Adatia I, Beghetti M. Immediate postoperative care. Cardiol Young 2009;19(Suppl. S1):23–27. [DOI] [PubMed]
- 41.Namachivayam P, Theilen U, Butt WW, Cooper SM, Penny DJ, Shekerdemian LS. Sildenafil prevents rebound pulmonary hypertension after withdrawal of nitric oxide in children. Am J Respir Crit Care Med 2006;174:1042–1047. [DOI] [PubMed]