Abstract
Objective:
To identify the determinants of misconceptions about diabetes in patients registered with a diabetes clinic at a tertiary care hospital in Eastern Saudi Arabia.
Materials and Methods:
This cross-sectional survey was carried out at a diabetes clinic of a tertiary care hospital in Eastern Saudi Arabia, from January to December 2012. A total of 200 diabetic patients were interviewed using a questionnaire comprising 36 popular misconceptions. The total misconception score was calculated and categorized into low (0-12), moderate (13-24) and high (25-36) scores. The association of misconception score with various potential determinants was calculated using Chi-square test. Step-wise logistic regression was applied to the variables showing significant association with the misconception score in order to identify the determinants of misconceptions.
Results:
The mean age was 39.62 ± 16.7 and 112 (56%) subjects were females. Type 1 diabetics were 78 (39%), while 122 (61%) had Type 2 diabetes. Insulin was being used by 105 (52.5%), 124 (62%) were self-monitoring blood glucose and 112 (56%) were using diet control. Formal education on diabetes awareness had been received by 167 (83.5%) before the interview. The mean misconception score was 10.29 ± 4.92 with 115 (57.5%) subjects had low misconception scores (<12/36). On the Chi-square test, female gender, rural area of residence, little or no education, <5 or >15 years since diagnosis, no self-monitoring, no dietary control and no diabetes education were all significantly (P < 0.05) associated with higher misconception scores. Step-wise logistic regression suggested that diabetes education, gender, education and time since diagnosis were significant (P < 0.05) predictors of misconception scores.
Conclusions:
The strongest determinants of misconceptions about diabetes in our study population were female gender, rural area of residence, illiteracy or little education, <5 or >15 years since diagnosis, no self-monitoring, no diet control and no education about diabetes.
Keywords: Diabetes, determinants, misconceptions, myths, Saudi Arabia
INTRODUCTION
Myths and misconceptions are part of any culture's identity. These misconceptions have a significant influence on the day-to-day life including the search for treatment in times of illness.[1] A number of studies have reported that misconceptions and inadequate knowledge present significant barriers to effective management of diabetes.[2,3] It is imperative for physicians to understand myths and misconceptions in a particular community about a disease to improve patient care, especially when dealing with chronic diseases like diabetes.
Diabetes mellitus (DM) is one of the most common noncommunicable diseases in the world and its prevalence is increasing dramatically. Currently, there are around 285 million diabetic patients around the world, and the numbers are predicted to rise to 439 million by 2030, with the largest increase in the developing rather than in the developed world.[4]
Diabetes is very common in the kingdom of Saudi Arabia. Its dramatic increase began a few decades ago with the rapid urbanization and development in the country. Studies in the 1980s showed a trend towards an increase among adult Saudis especially females.[5] A large study of Saudi patients from 1995 to 2000 revealed prevalence of 23.7%.[6] However, a study in 2011 showed a significant rise in prevalence reaching 34.1% in men and 27.6% in women.[7]
Correct knowledge about diabetes and its management has an enormous impact on attitude and practice of diabetic patients. A study of diabetic patients in New York, reported that patients with diabetes frequently had beliefs of the disease and medication that were false and even dangerous.[8] It is imperative that awareness of diabetes and its correct management be created and various myths and misconceptions surrounding its course and management be removed.[9]
A few excellent studies about prevailing misconceptions about diabetes have already been carried out in the Saudi population, more specifically in female diabetic teachers,[10] in the Eastern region,[11] Western region[12] and Qasim region.[9] However, no studies have examined in detail the determinants of the misconceptions of diabetic patients. Therefore, this study was undertaken to identify the determinants of prevailing misconceptions on diabetes and the management of diabetic patients registered at a diabetes clinic of a tertiary care hospital in the Eastern region of Saudi Arabia.
MATERIALS AND METHODS
This cross-sectional study was carried out at the diabetes clinic of a tertiary care hospital, in Eastern Saudi Arabia. Approval for the study was given by the Research and Ethical Committee. The data collection was carried out from January to December 2012.
This clinic has a registered patient population of 2000 diabetic patients. At a confidence level of 95%, response distribution of 50% and accepted margin of error of 10%, we calculated a sample size of 200. A table of random numbers was used to select patients from the medical record numbers of the registered patients of the diabetes clinic.
The inclusion criteria were all Saudi patients who had been registered at the diabetes clinic of the tertiary care hospital in Saudi Arabia for 6 months or more since diagnosis and on continuous treatment. No freshly diagnosed patient was included. In the same vein uncooperative or nonconsenting patients, as well as patients with any illness (physical or psychological) that was likely to influence reliable, valid responses to the interviewer's questions were excluded.
The same interviewer spoke to all the selected patients on their scheduled follow-up visits after taking their informed consent. When a prospective participant refused to take part, the next patient on the list of random numbers was asked until the sample size was completed. The interviewer was trained not to influence responses. The questionnaires were coded to ensure confidentiality. All attendees were interviewed in standardized conditions with prior information to ensure valid reliable responses.
The data collection instrument was an interviewer-filled questionnaire prepared in accordance with “Brief Illness Perception Questionnaire”[13] and “Belief About Medicines Questionnaire.”[14] All the questions were close-ended. The demographic and classification data included age categories (<20, 21-40, 41-60 or >60 years), gender (male and female), area of residence (urban or rural), education (primary, middle, high school, graduate and above), family history of diabetes (present or absent), type of diabetes (Type 1 or Type 2), time since diagnosis (<5, 6-10, 11-15 or >15 years), type of treatment (oral hypoglycemic or insulin), self-monitoring (yes or no) and diet control as per doctor's advice (yes or no). In order to establish validity and reliability of the questionnaire, a pilot study was conducted in a sub-sample of attendees who were not included in the study proper. Necessary changes were made in the questionnaire as well as the interview style as necessary.
Questions on the commonest reported misconceptions relating to etiology, types, pathogenesis, day-to-day life, diet and treatment of diabetes were included after a review of studies from Saudi Arabia,[9,10] USA,[8] India,[15,16] Nepal,[17] and Pakistan.[18] An answer in “yes” to a misconception question was considered a misconception and a score of one was given. The total misconception score of each patient was calculated. The total number of misconception questions was 36; therefore, the possible maximum score for any patient was 0-36. The scores were then arbitrarily divided into three equal categories of misconceptions. Low (scores 0-12), moderate (scores 13-24), and high (scores of 24-36). The highest misconception score represented the maximum number of misconceptions.
The data were analyzed by using IBM, SPSS-Version 19. Frequencies of all responses were calculated. Chi-square test was used to determine the association of the socio-demographic variables with the three categories of misconception scores. Stepwise logistic regression analysis was applied to the socio-demographic variables showing significant association with the misconception score by Chi-square test and values of β-coefficient, Chi-square, odds ratio, and confidence interval were reported.
RESULTS
A total of 200 responses for each item in the questionnaire were recorded from 200 subjects.
The mean age was 39.62 ± 16.70. The distribution of subjects in the age groups was 32 (16%) in <20 years, 62 (31%) in 21-40 years, 81 (40.5%) between 41 and 60 years and 25 (12.5%) in >60 years. The males were 88 (44%) and females 112 (56%). The subjects from urban areas were 168 (84%) and those from rural areas were 32 (16%). Those with the highest level of education were 7 (3.5%) who had up to postgraduation, 36 (18%) were university graduates, 76 (38%) high school, 43 (21.5%) middle, 29 (14.5%) primary and 9 (4.5%) illiterate. There was a family history of diabetes in 147 (73.5%) and no history in 53 (26.5%). Those with Type 1 diabetics were 78 (39%) while 122 (61%) had Type 2 diabetes.
The time since diagnosis was <5 years in 73 (36.5%), 6-10 years in 72 (36%), 11-15 years in 21 (10.5%) and >15 years in 34 (17%) subjects. The type of treatment was insulin in 105 (52.5%) and oral hypoglycemics in 95 (47.5%) indicating that many Type 2 diabetic patients were also on insulin. Self-monitoring of blood glucose was done by 124 (62%) of the subjects while 76 (38%) did not. Diet control was used by 112 (56%) subjects while 88 (44%) did not. A total of 167 (83.5%) had received formal “diabetes awareness education” while 33 (16.5%) had not.
The mean misconception score (n = 200) was 10.29 ± 4.92. The total misconception score was low (0-12) in 115 (57.5%), moderate (13-24) in 77 (38.5%) and high (24-36) in 8 (4%) respondents (n = 200).
Table 1 demonstrates the frequency distribution of respondents according to misconceptions about etiology, types and pathogenesis of diabetes. The most common misconceptions identified on etiology, types and pathogenesis were that “overweight causes diabetes” (89%), “diabetes is only a hereditary disease” (80.5%) and “eating too much sugar causes diabetes” (69%). In addition, this table shows the distribution of subjects with reference to misconceptions about daily life. The most frequent misconceptions about the daily life of diabetics were that “diabetics cannot lead a normal social life” (60%) and “one can feel an increase in blood sugar” (54.5%).
Table 1.
Frequency of respondents with misconceptions about etiology, types, pathogenesis and day-to-day life of diabetes (n=200)
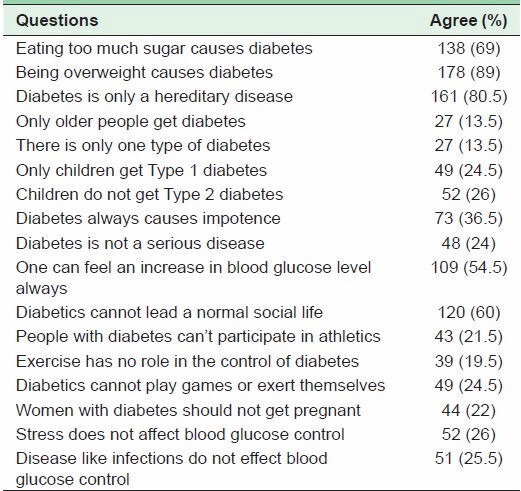
Table 2 illustrates the distribution of respondents according to misconceptions about diet. Similarly, the popular wrong beliefs regarding diet were that “diabetics must eat foods that are different from others” (47.5%) and “diabetics should never eat sweets” (47.5%). This table also depicts the distribution of diabetics with reference to misconceptions about treatment. The most common misconception on treatment was that “treatment of diabetes does not prevent complications” (89%). The second misconception on treatment was that “there is no need to take medicines when blood glucose is normal” (66.5%).
Table 2.
Frequency of respondents with misconceptions about diet and treatment (n=200)
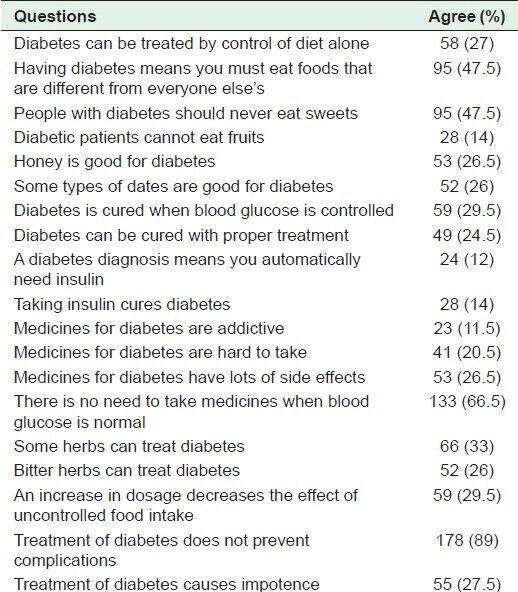
Table 3 shows the association of the selected socio-demographic variables on the misconception score. It shows that female gender, living in a rural area, little or no education, <5 or >15 years since diagnosis, lack of self-monitoring, poor compliance with dietary control and no diabetes education were significantly (P < 0.05) associated with moderate or high misconception score. However, age, family history of diabetes, type of diabetes and type of treatment were not significantly associated with the misconception score.
Table 3.
Association of misconception score category with sociodemographic variables
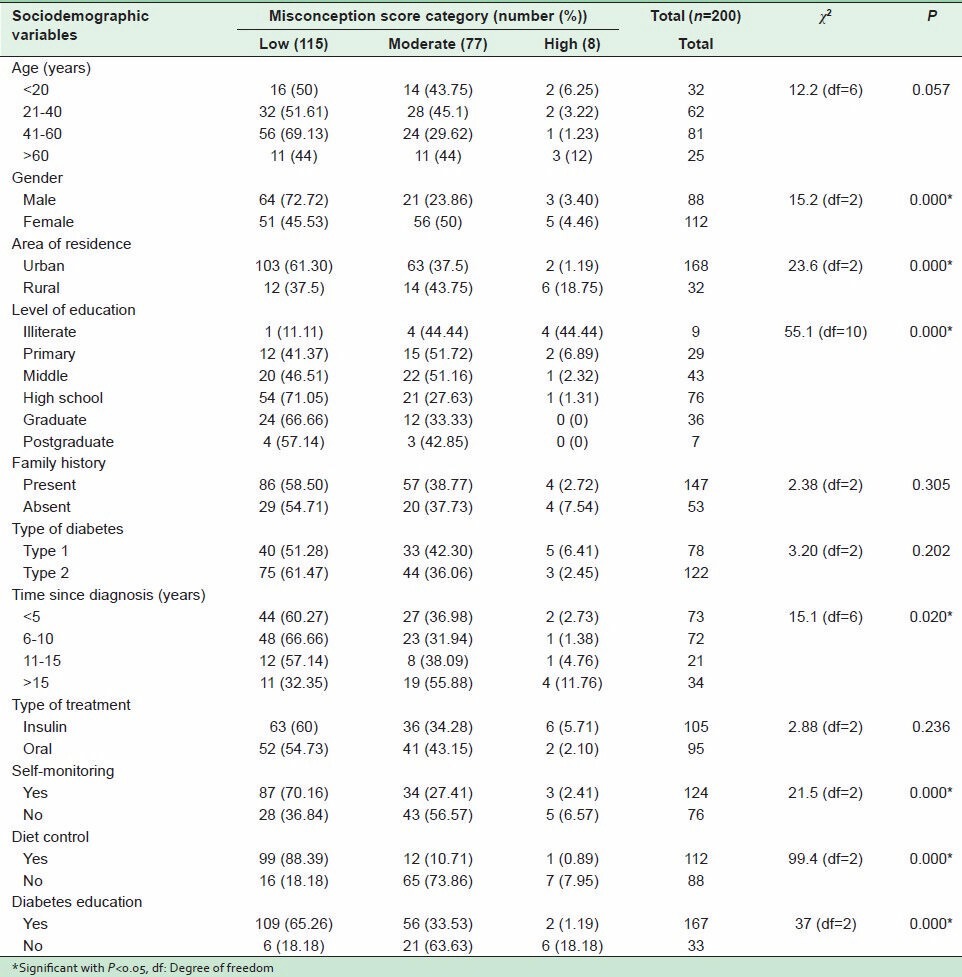
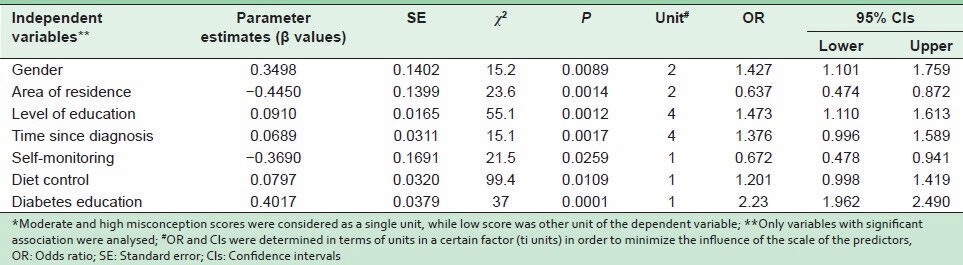
Table 4 gives stepwise logistic regression to determine the predictive value of independent variables [showing significant association as per Table 3] with the misconception score (dependent variable). It indicates that diabetes education, gender, education and time since diagnosis are good predictors of misconception score.
Table 4.
Logistic regression analysis of the determinants of misconceptions*
DISCUSSION
Every chronic disease necessitates long-term commitment from the patient, family and health care professionals. Health care is a full package that includes the proper education of society in general and the patient in particular, about all aspects of the disease in question.[19] A label of “no definitive cure” on chronic diseases generates many myths and misconceptions. These misconceptions are affected by socio-demographic factors and are propagated by opportunists who take advantage of patients to market their products. Understanding the myths and misconceptions about a disease, like DM, is important for the provision of excellent care and health education to both patients and healthy individuals.[1]
Myths and misconceptions related to diabetes are very common throughout the world. These myths and misconceptions are generally about forbidden foods, the use of herbs, life-style changes, side-effects of treatment and so-called “dependence on medicines.” They usually interfere with self-management plans for diabetic patients leading to undesirable complications.[20]
The frequency of common misconceptions reported by other studies is more or less similar to what our report presents. A previous study in Eastern Saudi Arabia that was carried out on adult male attendees of primary health centers found misconceptions about the etiology of diabetes in 21.2% of those studied, about general concepts of diabetes in 13.8% and diet in 10.7% of the patients.[11] However, our study population was different, in that all of them were diabetics. A study in Western Saudi Arabia reported that the top misconceptions that diabetic patients had were that “oral medications might be more effective than insulin,” “medications might cause habituation and serious complications,” “the efficacy of medications depends on their cost,” “cure is expected following a short course of treatment” and “a diabetic could eat anything as long as medications were taken.”[12]
The prevailing myths reported in the population of Qassim region of Saudi Arabia were that “consuming sugar results in diabetes,” “diabetics should avoid sweets,” “some type of dates do not increase sugar level,” “honey intake doesn't increase sugar level,” and “diabetes in its early stages can affect sexual performance.”[9]
Determinants of myths and misconceptions are the factors that are directly related to generation or propagation of these wrong beliefs. Knowledge of the determinants of any misconception, attitude or behavior is very important to the management of disease. This helps in the development of targeted education programs.[21]
Our results indicate that around 42.5% of the subjects had a moderate to high misconception score, indicating that there was much room for improvement in our patients' education. The mean misconception score was 10.29 ± 4.92, while 38.5% had moderate (1324) and 4% high (24-36) misconception scores. The factors which had a significant association with high misconception scores were female gender, rural residence, little or no education, <5 years or >15 years since diagnosis, no self-monitoring, poor diet control and no prior education about diabetes.
The relationships of different determinants of misconceptions studied in our study are discussed below. Female gender was found to be significantly (P < 0.05) associated with moderate to high misconception score. It was found to have a high predictive value of the misconceptions. This was not a totally unexpected finding due to social norms of a conservative society with significantly less exposure of women to information. This finding gave us a clear task to target our female patients to provide them with the correct knowledge about diabetes and its management.
A study carried out on female school teachers of Alkhobar showed that their understanding of diabetes was inadequate.[10] Similarly, a Sudanese study also found poor compliance to therapy, poor glycemic control and poor knowledge about diabetes in women as compared to men.[22] This association was also reported in misconception studies carried out in New York[8] and in India.[15] However, a study carried out in Qasim did not find gender to be associated with myths and misconceptions.[9]
The proportion of patients from rural areas was very low in our study as a result of the Saudi government's policy of ensuring that patients access health facilities nearest to their homes. However, the proportion of patients with moderate to high misconception scores was higher in patients from rural areas. This shows that certain socio-demographic factors render people from those areas more vulnerable to misconceptions. There is a need to develop special diabetes education programs for rural areas. However, there are other associated factors that can modify beliefs of urban populations as well.
In a study carried out in a low income population of New York, misconceptions about diabetes were common.[8] A survey carried out in the 4th largest city of India, Chennai, on around 26000 subjects concluded that even though there had been diabetes education campaigns from as far back as 1948, the level of lack of knowledge and misconceptions was unacceptable.[16]
The number of illiterate or highly educated persons was very low among our subjects. As expected, the proportion of subjects with moderate to high misconception was highest in the illiterate group, and this decreased as the level of education rose. The study by Sabra et al. in Eastern Saudi Arabia found high misconception scores in 23.5% of illiterate or those who could only read-and-write.[11] A study in New York found that participants with less than a high school education were more likely to have misconceptions.[8] A study of myths and misconceptions in the Qasim region also found significant differences in responses according to educational status.[9] A similar association with little education was reported from India.[15] This necessitates the identification of the less educated from the beginning in order to design special educational programs that suit their respective levels of education.
Time since diagnosis was found to be significantly associated (P < 0.05) with misconception scores. It also had a high predictive value for the misconception score. Patients who had been diagnosed with diabetes >15 years before were more prone to have a moderate to high misconception score, and the chances of having misconceptions decreased in categories as times since diagnosis lessened. This might be due to better current diabetes awareness programs as well as the ease of access to information for freshly diagnosed diabetics who are curious. The knowledge of the subjects presenting for the 1st time has generally been reported to be inadequate and other studies have indicated this relationship.[12,23]
The patients who reported that they were controlling their diabetes by self-monitoring of blood glucose had low misconception scores. This group comprised 62% of the total number of patients, about two-thirds of whom had low misconception scores. On the other hand, two-thirds of those who were not self-monitoring had moderate to high misconception scores. This shows that making the patient take charge of his or her diabetes control develops an interested attitude. In addition, a clear picture of alterations in blood sugar by medicines, diet control and life-style changes help in removing of unfounded baseless misconceptions. No other study has reported this association. However, a study from Western Saudi Arabia has shown an association of “discontinuity of treatment” with a high level of misconception.[12]
Noncompliance to the recommended diet control was found to be a major determinant of misconceptions. Surprisingly, most of patients with the highest misconception scores (7 out of 8) reported to have little or no diet control. This reflects a general carefree attitude of these patients to all aspects of life-style changes associated with the management of diabetes. However, most of the patients using the recommended diet control were found to have less misconception scores. This suggests that we must identify patients with a carefree attitude from the beginning and design proper education programs, with psychotherapy sessions if possible for them. No other study has reported this association.
The majority of the patients (83.5%) reported some formal instruction by health care professionals about diabetes and its management. As expected most of the subjects who had undergone a proper education about diabetes (presentation, management and life-style changes) had low misconception scores. Not surprisingly, this was the most significant single determinant of removing misconceptions about diabetes. The results also indicated that there was room for improvement in the education of the large proportion of patients with moderate to high misconception scores.
In our study, family history of diabetes, type of diabetes and type of treatment were not found to have any significant association with misconception scores. As in our study, the Qasim study did not find family history associated with myths and misconceptions.[9] Similarly, the age of our subjects did not show a significant association with misconception score. However, the proportion of subjects with moderate to high misconception scores was highest in the categories of the youngest and the oldest patients (<20 and >60 years). Though not statistically significant, it still shows that we must make an extra effort to educate these two vulnerable age groups about their disease.
Suboptimal knowledge and beliefs are potentially modifiable and are logical targets for educational interventions to improve diabetes self-management. Knowledge of all the identified determinants of moderate to high misconception scores will help in streamlining the awareness programs for patients in accordance with these factors. Similarly, it will act as a guideline for other units in our region to develop better patient education programs. If the patients are given proper guidance and education on diabetes care, there would be a significant improvement in their life-style which would in turn help in producing good glycemic control.
CONCLUSION
We conclude that myths and misconceptions about diabetes and its management are common in our patients. The strongest determinants of the misconceptions in our study population are female gender, rural area of residence, illiteracy or little education, <5 or >15 years since diagnosis, no self-monitoring of blood glucose, poor diet control and no education about diabetes. Therefore, diabetes educational programs should focus on individuals with one or more of these predictors.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Adler E, Paauw D. Medical myths involving diabetes. Prim Care. 2003;30:607–18. doi: 10.1016/s0095-4543(03)00032-0. [DOI] [PubMed] [Google Scholar]
- 2.Searle A, Wetherell MA, Campbell R, Dayan C, Weinman J, Vedhara K. Do patients' beliefs about type 2 diabetes differ in accordance with complications: An investigation into diabetic foot ulceration and retinopathy. Int J Behav Med. 2008;15:173–9. doi: 10.1080/10705500802212940. [DOI] [PubMed] [Google Scholar]
- 3.Aikens JE, Piette JD. Diabetic patients' medication underuse, illness outcomes, and beliefs about antihyperglycemic and antihypertensive treatments. Diabetes Care. 2009;32:19–24. doi: 10.2337/dc08-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Fatani HH, Mira SA, el-Zubier AG. Prevalence of diabetes mellitus in rural Saudi Arabia. Diabetes Care. 1987;10:180–3. doi: 10.2337/diacare.10.2.180. [DOI] [PubMed] [Google Scholar]
- 6.Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, Al-Harthi SS, Arafah MR, Khalil MZ, et al. Diabetes mellitus in Saudi Arabia. Saudi Med J. 2004;25:1603–10. [PubMed] [Google Scholar]
- 7.Alqurashi KA, Aljabri KS, Bokhari SA. Prevalence of diabetes mellitus in a Saudi community. Ann Saudi Med. 2011;31:19–23. doi: 10.4103/0256-4947.75773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mann DM, Ponieman D, Leventhal H, Halm EA. Misconceptions about diabetes and its management among low-income minorities with diabetes. Diabetes Care. 2009;32:591–3. doi: 10.2337/dc08-1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharaf FK, Naeem Z, Mohaimeed AA, Sawaf MN. Prevailing myths and misconceptions about diabetes mellitus in Qassim Region of Saudi Arabia. [Last accessed on 2013 Nov 10];Ann Alquds Med. 2006 6:i–viii. Available from: http://www.annalqudsmed.files.wordpress.com/2010/05/dm.myths.pdf . [Google Scholar]
- 10.Abahussain NA, El-Zubier AG. Diabetes knowledge among self reported diabetic female teachers: Al-Khobar, Saudi Arabia. J Family Community Med. 2005;12:43–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Sabra AA, Taha AZ, Al-Zubier AG, Al-Kurashi NY. Misconceptions about diabetes mellitus among adult male attendees of primary health care centers in Eastern Saudi Arabia. S Afr Fam Pract. 2010;52:344–9. [Google Scholar]
- 12.Al-Saeedi M, Elzubier AG, Bahnassy AA, Al-Dawood KM. Treatment-related misconceptions among diabetic patients in Western Saudi Arabia. Saudi Med J. 2002;23:1243–6. [PubMed] [Google Scholar]
- 13.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 14.Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14:1–24. [Google Scholar]
- 15.Rai M, Kishore J. Myths about diabetes and its treatment in North Indian population. Int J Diabetes Dev Ctries. 2009;29:129–32. doi: 10.4103/0973-3930.54290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohan D, Raj D, Shanthirani CS, Datta M, Unwin NC, Kapur A, et al. Awareness and knowledge of diabetes in Chennai - the Chennai Urban Rural Epidemiology Study [CURES-9] J Assoc Physicians India. 2005;53:283–7. [PubMed] [Google Scholar]
- 17.Upadhyay DK, Palaian S, Shankar PR, Mishra P. Knowledge, attitude and practice about diabetes among diabetes patients in Western Nepal. Rawal Med J. 2008;33:8–11. [Google Scholar]
- 18.Nisar N, Khan IA, Qadri MH, Sher SA. Myths about diabetes mellitus among non-diabetic individuals attending primary health care centers of Karachi subrubs. J Coll Physicians Surg Pak. 2007;17:398–401. [PubMed] [Google Scholar]
- 19.Rafique G, Shaikh F. Identifying needs and barriers to diabetes education in patients with diabetes. J Pak Med Assoc. 2006;56:347–52. [PubMed] [Google Scholar]
- 20.Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–67. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 21.WHO. Health Impact Assessment. (HIA) The determinants of health. [Last accessed on 2013 Nov 10]. Available from: http://www.who.int/hia/evidence/doh/en/
- 22.Ahmed AM, Hussein A, Kheir MM, Ahmed NH. Impact of diabetes mellitus on Sudanese women. Pract Diabetes Int. 2001;18:115–8. [Google Scholar]
- 23.Badruddin N, Basit A, Hydrie MZ, Hakeem R. Knowledge, attitude and practices of patients visiting a diabetes care unit. Pak J Nutr. 2002;1:99–102. [Google Scholar]


