Abstract
Background
This study examined the relationship between race and Hispanic ethnicity, maternal and child nativity, country of origin and asthma among 2,558 non-Hispanic white and Hispanic children across 65 Los Angeles neighborhoods.
Methods
A series of two-level multilevel models were estimated to examine the independent effects of race, ethnicity, and country of origin on childhood asthma.
Results
Lifetime asthma prevalence was reported among 9% of children, with no significant differences between Hispanics and non-Hispanic whites overall. However, in fully adjusted models, Hispanic children of non-Mexican origin reported higher odds of asthma compared to non-Hispanic white children. A protective nativity effect was also observed among children of foreign born mothers compared to US born mothers.
Discussion
Our study provides evidence in support of the heterogeneity of childhood asthma by Hispanic ethnicity and maternal nativity. These findings suggest moving beyond solely considering racial/ethnic classifications which could mask subgroups at increased risk of childhood asthma.
Keywords: childhood asthma, nativity, Hispanic, Latino paradox
BACKGROUND
The Hispanic Health Paradox also described as the Latino or Epidemiologic Paradox, refers to the relatively good health of Latinos within the US, despite what lower levels of socioeconomic status might predict [1]. The Hispanic health paradox has been well studied within the literature across a range of health outcomes including, mortality, cardiovascular diseases, and preterm birth [2–6]. Health advantage has particularly been observed among Hispanics of Mexican background, particularly Mexican immigrants.
Within the Hispanic health paradox literature, asthma has also been studied [7–12]. Nationally, asthma prevalence among Hispanic children overall has been comparable to that of non-Hispanic White children. Among California children, the prevalence of active asthma varies by racial and ethnic groups—with the highest prevalence among African Americans (17%) and American Indians/Alaska Natives (17%), followed by Whites (10%), then Hispanics (7%) and Asians (7%) [13]. However, substantially heterogeneity within Hispanic subgroups has also been observed; Hispanics of Puerto Rican origin have the highest prevalence of asthma (26%) while Hispanics of Mexican origin reported the lowest (10%) [14–16]. The wide variation in asthma prevalence among Hispanic subgroups challenges the notion of the Hispanic health paradox and has prompted investigation into other factors, including acculturation, nativity, and country of origin.
Within Hispanics of Mexican origin, a nativity effect has also been observed, with immigrant children reporting a lower prevalence of asthma compared to second generation or third generation children [12]. These differences have also been observed among Hispanics of Puerto Rican origin, when comparing mainland Puerto Rican children to Puerto Rican children within the US [17]. Further research is needed to help disentangle the influences of race/ethnicity, nativity, and country of origin on childhood asthma outcomes, which can potentially target interventions and inform policy to reduce asthma disparities. The present study was designed to explore heterogeneity in childhood asthma across Hispanic ethnic groups by country of origin and maternal and child nativity.
METHODS
Participants
The Los Angeles Family and Neighborhood Survey (L.A.FANS) is a longitudinal study of children and adolescents within Los Angeles neighborhoods designed to examine the influences of neighborhood, family, and individual factors on a range of health outcomes and behaviors [18]. Wave 1 of L.A.FANS, a stratified random sample of 65 neighbhorhoods (defined by census tracts), included children (ages 0–17) living within one of 65 neighborhoods and oversampled participants within very poor and poor neighborhoods. Characteristics of sampled tracts generally correspond to the tracts they represent, within each poverty strata. However, due to the oversampling of very poor and poor neighborhoods, there are more Hispanics, but fewer whites, blacks, and Asians than expected given census data [19].
Interviews were conducted in-person in English or Spanish by trained field interviewers using computer assisted personal interviewing technology; 89% of primary caregivers selected for the study completed interviews [18]. Households with children received $50 and participants without children received $25 upon completion of the interview. Within the interviews, completed between 2000 and 2002, participants provided a wide range of information on nativity, country of origin, socioeconomic measures, and health measures for children and primary caregivers. These data allowed us to examine differences in asthma prevalence, not only by overall racial/ethnic groupings, but also by Hispanic subgroups and child and maternal nativity.
We restricted our sample to children of Hispanic or non-Hispanic White racial/ethnic origin due to the small sample sizes and lack of data regarding nativity of children within non- Hispanic Black, Asian, Pacific Islander, and Native American/American Indian categories. Due to these limitations we would have been unable to examine the effects of child or maternal nativity, two of our primary variables of interest. Children who were of White origin and another racial group were also excluded from our analyses. Children who were of both Hispanic origin and another racial group were categorized as Hispanic including children who reported both Hispanic and White race. Our analyses included 2,558 children (ages 0–17 years) of non-Hispanic White or Hispanic race/ethnicity who also had data on our outcome of interest, of which Hispanic children comprised approximately 78% of our sample.
Measures
We ascertained child’s lifetime asthma status via the primary caregiver’s report of an asthma diagnosis within the parent module of L.A.FANS. Children were categorized as asthmatic if the primary caregivers reported a positive response to the following item: “has a doctor or other health professional ever told you that [child’s name] has asthma?” Similar questions to ascertain asthma prevalence have been used within the International Study of Asthma and Allergies in Childhood (ISAAC) survey [20].
Child’s race/ethnicity was provided by the primary caregiver within the roster module of L.A.FANS. Maternal nativity and country of origin was assessed within the parent module of L.A.FANS. Mother’s response to the country where she was born was used to categorize maternal nativity; response options were collapsed into two categories- born in the (1) born in the United States and (2) born elsewhere. These categories enabled us to ascertain the effect of maternal nativity on asthma independent of country of origin. To categorize ethnicity within Hispanics, we used mother’s response to the following questions:
Are you a Mexican/Mexicano?
Are you a Mexican American?
Are you a Central American?
Are you a Caribbean?
Are you an other Latin American?
Are you an other Hispanic?
Responses were further collapsed into the following categories- (1) Mexican or Mexican American; (2) Central American, Caribbean, Latin American, or other Hispanic. Approximately 20% of Hispanic respondents were of non-Mexican ethnicity.
The child’s nativity was provided by the primary caregiver’s response to the following question, “was the child born in the United States?” Although a considerable percentage of Hispanic children within L.A.FANS were foreign born (approximately 12%), the majority of foreign born children were born in Mexico. As such, we were unable to further categorize children by country of origin. In order to examine the interaction between country of origin and maternal nativity, we considered mother’s response to questions regarding ethnicity and country of birth. We categorized mothers into the following categories: (1) US born Non-Hispanic White, (2) Foreign born White, (3) US born Mexican, (4) Foreign born Mexican, (5) US born other Hispanics and (6) Foreign born other Hispanics.
Covariates were chosen for inclusion based on prior literature and availability of data. At the individual level, child’s age, gender, race/ethnicity, health insurance status, and place of care were included which were provided by the primary caregiver during the parent module. At the household level, we adjusted for primary caregiver’s education (years), receipt of public assistance within the past 12 months, maternal history of asthma, and the primary caregiver’s current smoking status. We reported both unadjusted and adjusted models to examine potential confounding due to observed covariates.
Analytic strategy
As our data have natural and sampling induced nesting, we conducted a series of two level multilevel logistic regression models of children at level 1 nested within census tracts at level 2. We first examined the overall effect of race/ethnicity of the log odds of reporting an asthma diagnosis among all Hispanic children compared to non-Hispanic Whites. This model enabled us to examine the contribution of Hispanic ethnicity overall on the log odds of reporting an asthma diagnosis compared to non-Hispanic Whites. We then modeled the unadjusted effect of maternal Hispanic country of origin (non-Hispanic White, Hispanics of Mexican origin, Hispanics of non-Mexican origin) on the log odds of reporting an asthma diagnosis and subsequently adjusted for child’s age, gender, primary caregiver’s education, receipt of public assistance, health insurance status and place of care, maternal smoking status and asthma history. Lastly, we modeled the unadjusted and adjusted effects of maternal nativity (foreign born vs. US born) and racial/ethnic groups on the log odds of reporting an asthma diagnosis within children. Together these series of models enabled us to test the heterogeneity within Hispanic subgroups and also the joint contributions of nativity and race/ethnicity on asthma outcomes [12]. Descriptive analyses were conducted using STATA v.11; multilevel models were implemented using MLwiN. The study was approved by the Office of Human Research Administration at the Harvard School of Public Health. Participants provided informed consent orally during the initial LAFANS interview; data were protected via a certificate of confidentiality. Reconsent was waived in order to avoid identification of study participants.
RESULTS
Lifetime asthma prevalence was reported among 9.7% of children within the sample. Table I displays the individual and household sociodemographic characteristics of participants among asthmatics and non-asthmatics as well as the unadjusted odds ratios for predictors of interest and covariates. Approximately 22% of children within the sample were non-Hispanic White; among non-Hispanic White children, 11% had a lifetime reported asthma diagnosis. Among Hispanic children overall, 9% had a lifetime reported asthma diagnosis. However, significant heterogeneity was found within Hispanic subgroups as children of Mexican origin had the lowest asthma prevalence (approximately 6.9%), while 11.4% of children of non-Mexican origin reported an asthma diagnosis.
Table I.
Distribution of lifetime reported asthma diagnosis by individual and primary caregiver characteristics among non-Hispanic White and Hispanic children within the Los Angeles Family and Neighborhood Survey
| Individual characteristics | Asthmatics (n = 247) | Non-asthmatics (n = 2311) |
Crude OR (95%CI) |
|---|---|---|---|
| Gender | |||
| Male | 137 (55.5) | 1151 (49.8) | 1 |
| Female | 110 (44.5) | 1160 (50.2) | 0.83 (0.64–1.09) |
| Age (years) | |||
| ≤5 | 68 (27.5) | 869 (37.6) | 1 |
| 6–10 | 71 (28.7) | 699 (30.3) | 1.35 (0.95–1.91) |
| 11–14 | 63 (25.5) | 433 (18.7) | 1.82 (1.26–2.63) |
| ≥15 | 45 (18.2) | 310 (13.4) | 1.82 (1.21–2.73) |
| Race/ethnicity | |||
| White | 65 (26.3) | 503 (21.8) | 1 |
| Hispanic | 182 (76.7) | 1808 (78.2) | 0.80 (0.57–1.14) |
| Child nativity | |||
| US born | 228 (92.3) | 2005 (86.8) | 1 |
| Foreign born | 19 (7.7) | 306 (13.2) | 0.58 (0.36–0.93) |
| Health Insurance | |||
| Insured | 197 (86.0) | 1659 (78.8) | 1.49 (1.08–2.07) |
| Partially or uninsured | 32 (14.0) | 447 (21.2) | 1 |
| Primary caregiver characteristics | |||
| Ethnicity (country of origin) | |||
| Non Hispanic White | 65 (32.3) | 503 (24.7) | 1 |
| Hispanic, Mexican origin | 82 (40.8) | 1,111 (54.6) | 0.53 (0.39–0.73) |
| Other Hispanic origin | 54 (26.9) | 420 (20.7) | 0.81 (0.54–1.22) |
| Maternal nativity | |||
| Foreign born | 130 (53.3) | 1578 (69.5) | 0.52 (0.39–0.69) |
| US born | 114 (46.7) | 692 (30.5) | 1 |
| Education (years) | |||
| < 12 | 86 (34.8) | 1152 (49.9) | 1 |
| 12 | 60 (24.3) | 389 (16.8) | 2.01 (1.41–2.88) |
| >12 | 101(40.9) | 770 (33.3) | 1.72 (1.24–2.40) |
| Public assistance | |||
| No | 210 (86.4) | 2025 (89.4) | 1 |
| Yes | 33 (13.6) | 239 (10.6) | 1.42 (0.96–2.11) |
| Current smoking status | |||
| No | 213 (87.3) | 2078 (92.0) | 1 |
| Yes | 30 (12.7) | 181 (8.0) | 1.56 (1.02–2.39) |
| Asthma history | |||
| No | 209 (84.9) | 2155 (95.4) | 1 |
| Yes | 34 (15.1) | 104 (4.6) | 3.39 (2.23–5.16) |
Children who were foreign born also had a lower prevalence of an asthma diagnosis compared to their US-born counterparts (5.8% versus 10.2% respectively. Children of foreign-born mothers also had a lower prevalence of reported asthma diagnosis (7.7%) compared to children of US born mothers (14.2%).
Examining additional sociodemographic variables, older children had higher odds of reporting an asthma diagnosis compared to those in younger age categories. Primary caregiver’s education was also significantly associated with asthma diagnosis; primary caregivers with a high school degree or equivalent as well as those with more than a high school education reported higher odds of child’s asthma diagnosis, compared to those with less than a high school education. Higher odds of reporting an asthma diagnosis among children were also seen among primary caregivers who were smokers as well as those who also had a history of asthma.
Effects of race/ethnicity and maternal and child nativity
Within Table II, we reported the mutually adjusted effects of race/ethnicity and child nativity, after controlling for individual and primary caregiver characteristics. Odds of reporting lifetime asthma among children did not differ between Hispanics and non-Hispanic Whites overall. In addition, no significant differences were observed between foreign-born children and US-born children. However, children of immigrant mothers had significantly lower odds of reporting an asthma diagnosis compared to children of non-immigrant mothers (odds ratio [OR] = 0.69; 95% confidence interval [CI] = 0.47–0.99). This effect persisted even after controlling for race/ethnicity (OR = 0.64; 95% CI = 0.44–0.94).
Table II.
Adjusted Odds Ratios (ORs) and 95% Confidence Intervals (CI) for Lifetime Reported Asthma among L.A.FANS Children by Race/Ethnicity and Mother and Child Nativity
| Model 1a | Model 2b | |
|---|---|---|
| Race/Ethnicity | ||
| White | 1.00 | 1.00 |
| Latino | 1.20 (0.78–1.83) | 1.34 (0.88–2.06) |
| Maternal nativity | ||
| US born | 1.00 | 1.00 |
| Foreign born | 0.69 (0.47–0.99)* | 0.64 (0.44–0.94)* |
| Child nativity | ||
| US born | 1.00 | 1.00 |
| Foreign born | 0.59 (0.39–1.11) | 0.59 (0.39–1.10) |
p < 0.05
Model 1 Adjusted for child’s age, gender, child’s health insurance status, primary caregiver’s education, receipt of public assistance, primary caregiver’s current smoking status, and maternal asthma history
Model 2 Adjusted for all covariates in model 1 and mutually adjusted for race/ethnicity and nativity
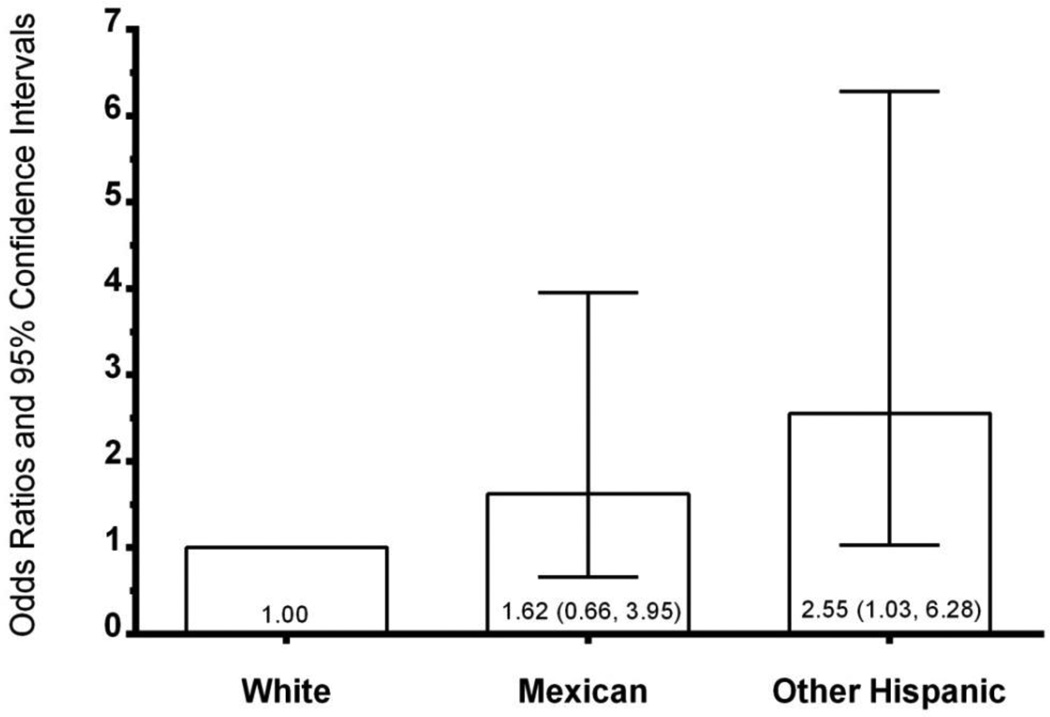
Significant heterogeneity was found within Hispanic subgroups, even after controlling for all covariates and maternal and child nativity (Figure 1). The odds of lifetime reported asthma were not significantly different between children of Mexican ethnicity compared to non-Hispanic Whites. Non-Mexican Hispanic children had a substantially increased risk of reported asthma diagnosis compared to non-Hispanic White children (OR = 2.55; 95% CI = 1.03–6.28), even after controlling for maternal and child nativity.
Figure 1. Odds ratios and 95% confidence intervals for lifetime asthma diagnosis among LA FANS children by race/ethnicity.
Note: The results reflect adjustment for children’s age, gender, health insurance status, primary caregiver’s education, receipt of public assistance, current smoking status, maternal asthma history, and maternal and child nativity.
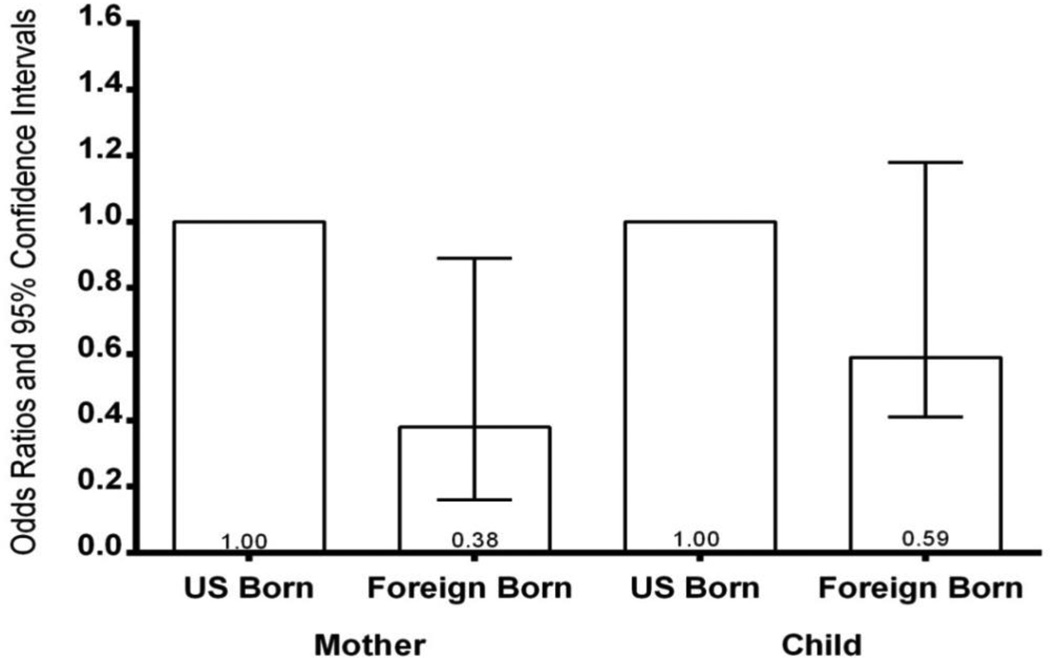
In Figure 2, we reported the effects of maternal and child nativity, adjusted for individual and primary characteristics, as well as Hispanic ethnicity. Maternal nativity was significant where children of mothers who were born outside of the United States had lower odds of reporting an asthma diagnosis compared to children born within the United States (OR = 0.38; 95% CI = 0.16–0.89). This effect persisted after controlling for all covariates and regardless of Hispanic ethnicity. No significant differences were observed with respect to child nativity (0.59; 0.41–1.18). Table III displayed the adjusted results for various combinations of race, Hispanic/ethnicity and maternal nativity. In unadjusted models, children of immigrant Mexican mothers were significantly less likely to report an asthma diagnosis compared to non-Hispanic white children (OR = 0.59; 95% CI = 0.31–0.70). Children of immigrant white mothers were also significantly less likely to report an asthma diagnosis compared children of US-born white mothers (OR = 0.44; 95% CI = 0.21–0.94). These effects did not persist in fully adjusted models.
Figure 2. Odds ratios and 95% confidence intervals for lifetime asthma diagnosis among LA FANS children by maternal and child nativity.
Note: The results reflect adjustment for children’s age, gender, health insurance status, primary caregiver’s education, receipt of public assistance, current smoking status, maternal asthma history, and ethnicity.
Table III.
Unadjusted and Adjusted Odds Ratios (ORs) and 95% Confidence Intervals (CI) for Lifetime Reported Asthma among L.A.FANS Children by Race/Ethnicity and Maternal Nativity
| Model 1a | Model 2b | |
|---|---|---|
| Nativity and Race/Ethnicity | ||
| US born White | 1.00 | 1.00 |
| Foreign born White | 0.44 (0.21–0.94)* | 0.50 (0.22–1.08) |
| US born Mexican | 1.01 (0.63–1.61) | 1.05 (0.61–1.81) |
| Foreign born Mexican | 0.59 (0.31–0.70)* | 0.59 (0.44–1.27) |
| US born other Hispanic | 1.36 (0.65–2.84) | 1.69 (0.73–3.92) |
| Foreign born other Hispanic | 0.59 (0.51–1.27) | 1.22 (0.70–2.11) |
p < 0.05
Model 1 Unadjusted model
Model 2 Adjusted for child’s age, gender, child’s health insurance status, primary caregiver’s education, receipt of public assistance, primary caregiver’s current smoking status, and maternal asthma history
DISCUSSION
Our study had several important findings. First, consistent with other literature examining asthma prevalence among Hispanic subgroups, our research demonstrated that classification of Hispanics as one ethnic group overall masked significant heterogeneity between groups. Overall, children of Hispanic ethnicity did not report different rates of asthma diagnosis compared to non-Hispanic White children; however this result may have been masked by lower prevalence among children of Mexican origin as further disaggregation by country of origin demonstrated that children of non-Mexican Hispanic origin reported an increased risk of asthma diagnosis compared to non-Hispanic white children.
Several studies of asthma prevalence, morbidity, and mortality have found significant variation among Hispanic ethnic groups [14–16]. Consistently, asthma prevalence has been highest among Puerto Ricans, followed by Dominicans and Cubans, and lowest among Central Americans and Mexicans [21–24]. Results from the ISAAC study indicated a wide variation of asthma prevalence between Latin American countries and within Latin American countries. Lifetime asthma prevalence ranged from 1.2% in the Mexicali Valley in Mexico to 33.1% in Lima Peru [25]. Researchers searching for potential explanations for this observed variation have examined the independent contributions of genetic, socioeconomic, and environmental factors as well as their potential interactions. Gene-environmental studies have yielded mixed results; while some studies have found evidence in support of the interplay of socioeconomic and ancestry markers among Hispanic subgroups [26], others have found no significant associations between ancestry and asthma prevalence and morbidity among Puerto Rican and Mexican groups [27,28].
Within Hispanics, a nativity effect was clearly observed for maternal nativity. Children of foreign born mothers had significantly lower odds of reporting an asthma diagnosis compared to their US-born counterparts, even after controlling for socioeconomic factors, smoking, maternal asthma history, and race/ethnicity. The nativity effect was also demonstrated among children of non-Hispanic origin; in unadjusted models, children of foreign born White mothers also demonstrated lower odds of an asthma diagnosis compared to children of US born white mothers. The effect of nativity on childhood asthma has been confirmed in prior studies as well [7, 10, 12, 29–31].
Several potential explanations for the protective effect of nativity among foreign born mothers and children have been offered in the literature. One potential explanation for the observed nativity effect has been referred to as the “healthy migrant effect,” which posits that individuals who have the health resources (general health with lower prevalence of various chronic diseases) to migrate are more likely to do so compared to their less healthy counterparts [32, 33]. However, research examining selective migration is scarce and results have been mixed [3, 17, 34]. While migrant effects may contribute to variation in asthma outcomes among foreign born and US born groups, it is unlikely to completely explain observed differences [35].
Limitations
Our study did have several limitations which should be considered. First, our classification of child’s asthma status was derived from maternal reports. There may have been potential for diagnostic bias for asthma, particularly among households of lower socioeconomic status and racial/ethnic minority groups. In addition, Hispanic participants of Mexican-descent may be less likely to receive an asthma diagnosis (particularly among foreign-born Mexicans), given evidence lower health care use [36]. While we attempted to account for this by not only controlling for household SES, but also by adjusted for the health insurance status, we were unable to include additional factors on health care use (such as having a usual place of care or primary care physician). Prior studies examining diagnostic bias among children with asthma symptoms have not found evidence of under diagnosis among minority children compared to non-Hispanic white children [37]. Additional studies have also observed a nativity advantage with respect to physician-diagnosed asthma among children of Mexican descent [10]. In addition, although response rates were generally high among participants selected into the study, there may have been potential for response bias based on country of origin or nativity status among Hispanics. There also could have been differences by country of origin or nativity status among Hispanics which could have influenced parents to seek health care for asthmatic children, which we were unable to account for in our study.
Our study did not include measures of acculturation, including language preference, length of stay, or other assessments of cultural beliefs. While much of the literature regarding the Hispanic health paradox focuses on acculturation, explanations for the paradox remain elusive [7]. Although nativity and country of origin have often been used as proxies for acculturation, our study have examined these factors as distinct constructs. Studying nativity and country of origin separate from acculturation enabled us to examine the contributions of immigrating to the United States from various native countries, prompting future research to utilize a cross-national perspective and focus on the environmental and social conditions of native countries. While the examination of acculturation may help highlight the processes by which conditions and characteristics of the host country influence the asthma outcomes of immigrants and subsequent generations, they are distinct questions and should be examined independently of one another. The second wave of the Los Angeles Family and Neighborhood Survey (L.A.FANS-2), which re-interviewed participants from the first wave and included a sample of new entrants into the neighborhoods, includes measures of acculturation. Future studies utilizing L.A.FANS-2 may be able to examine the relative contributions of nativity, country of origin, and acculturation within a similar population and context.
Lastly, our study was restricted to Los Angeles County and may limit generalizability to other populations and contexts. However, comparing our results to additional similar studies conducted within Midwestern and Northeastern cities, we found similar results for the effects of nativity and country of origin. However, our study population may have been ideally suited to examine the Hispanic Health paradox, due to the large proportion of Hispanics within our sample and our ability to disaggregate by both country of origin and assess maternal and child nativity status.
CONCLUSIONS
Our study provides evidence in support of the heterogeneity of childhood asthma across Hispanic ethnic groups and child and maternal nativity, prompting future research to reconsider the use of the term Hispanic Health paradox. The term misleadingly implies that Hispanic ethnic groups exhibit the same health outcome; our study provides support of the existing literature demonstrating that the prevalence of chronic disease may vary widely across Hispanic ethnic groups, particularly in the context of asthma. As the body of literature supporting the heterogeneity of health outcomes among Hispanic subgroups continues to increase, researchers should consider a nuanced approach to account for the paradox [38–40]. Future studies should further examine the effects of nativity within diverse racial/ethnic groups and across a variety of contexts, with a particular focus on multilevel strategies and examining the interplay between individual genetic, socioeconomic, and cultural factors and social and structural explanations [41–43]. Together, current and future studies can potentially inform programs and policies that may reduce childhood disparities in asthma within the United States.
What is already known on this subject.
Although overall asthma prevalence is low among Hispanic children, significant heterogeneity exists between subgroups. Although acculturation has been examined as a potential explanation for differences within Hispanics, few studies have explicitly examined the contributions of maternal and child nativity, country of origin, and their potential interactions.
What this study adds.
Our study provides evidence in support of the heterogeneity of childhood asthma across Hispanic ethnic groups and child and maternal nativity, prompting future research to reconsider the use of the term Hispanic Health paradox. Future studies should further examine the effects of nativity within diverse racial/ethnic groups and across a variety of contexts.
Acknowledgements
This study was supported by a National Institutes of Health Career Development Award NHLBI K25 HL081275 and a US Department of Health and Human Services (HRSA) Public Health Traineeship Grant. We thank RAND Corporation for the use of data from the Los Angeles Family and Neighborhood Survey.
Contributor Information
Marlene Camacho-Rivera, Department of Population Health, North Shore-Long Island Jewish Health System, Great Neck, NY, USA.
Ichiro Kawachi, Department of Social and Behavioral Sciences, Harvard School of Public Health, Boston, MA, USA.
Gary G Bennett, Department of Psychology and Neuroscience, Duke University, Durham, NC, USA.
S.V. Subramanian, Department of Social and Behavioral Sciences, Harvard School of Public Health, Boston, MA, USA.
REFERENCES
- 1.Abraido-Lanza AF, Armbrister AN, Florez KR, et al. Toward a theory-driven model of acculturation in public health research. Am J Public Health. 2006;96(8):1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Acevedo-Garcia D, Soobader MJ, Berkman LF. Low birthweight among US Hispanic/Latino subgroups: the effect of maternal foreign-born status and education. Soc Sci Med. 2007;65(12):2503–2516. doi: 10.1016/j.socscimed.2007.06.033. [DOI] [PubMed] [Google Scholar]
- 3.Ceballos M, Palloni A. Maternal and infant health of Mexican immigrants in the USA: the effects of acculturation, duration, and selective return migration. Ethn Health. 2010;15(4):377–396. doi: 10.1080/13557858.2010.481329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Creighton MJ, Goldman N, Pebley AR, et al. Durational and generational differences in Mexican immigrant obesity: is acculturation the explanation? Soc Sci Med. 2012;75(2):300–310. doi: 10.1016/j.socscimed.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Wieren AJ, Roberts MB, Arellano N, et al. Acculturation and cardiovascular behaviors among Latinos in California by country/region of origin. J Immigr Minor Health. 2011;13(6):975–981. doi: 10.1007/s10903-011-9483-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cagney KA, Browning CR, Wallace DM. The Latino paradox in neighborhood context: the case of asthma and other respiratory conditions. Am J Public Health. 2007;97(5):919–925. doi: 10.2105/AJPH.2005.071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eldeirawi K, McConnell R, Freels S, et al. Associations of place of birth with asthma and wheezing in Mexican American children. J Allergy Clin Immunol. 2005;116(1):42–48. doi: 10.1016/j.jaci.2005.03.041. [DOI] [PubMed] [Google Scholar]
- 9.Gold DR, Acevedo-Garcia D. Immigration to the United States and acculturation as risk factors for asthma and allergy. J Allergy Clin Immunol. 2005;116(1):38–41. doi: 10.1016/j.jaci.2005.04.033. [DOI] [PubMed] [Google Scholar]
- 10.Eldeirawi K, McConnell R, Furner S, et al. Associations of doctor-diagnosed asthma with immigration status, age at immigration, and length of residence in the United States in a sample of Mexican American School Children in Chicago. J Asthma. 2009;46(8):796–802. [PubMed] [Google Scholar]
- 11.Eldeirawi KM, Persky VW. Associations of physician-diagnosed asthma with country of residence in the first year of life and other immigration-related factors: Chicago Asthma School Study. Annals of Allergy, Asthma & Immunology. 2007;99(3):236–243. doi: 10.1016/S1081-1206(10)60659-X. [DOI] [PubMed] [Google Scholar]
- 12.Subramanian SV, Jun HJ, Kawachi I, et al. Contribution of race/ethnicity and country of origin to variations in lifetime reported asthma: evidence for a nativity advantage. Am J Public Health. 2009;99(4):690–697. doi: 10.2105/AJPH.2007.128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis AM, Kreutzer R, Lipsett M, et al. Asthma prevalence in Hispanic and Asian American ethnic subgroups: results from the California Healthy Kids Survey. Pediatrics. 2006;118(2):e363–e370. doi: 10.1542/peds.2005-2687. [DOI] [PubMed] [Google Scholar]
- 14.Lara M, Akinbami L, Flores G, et al. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117(1):43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 15.Canino G, Koinis-Mitchell D, Ortega AN, et al. Asthma disparities in the prevalence, morbidity, and treatment of Latino children. Soc Sci Med. 2006;63(11):2926–2937. doi: 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 16.Hunninghake GM, Weiss ST, Celedon JC. Asthma in Hispanics. Am J Respir Crit Care Med. 2006;173(2):143–163. doi: 10.1164/rccm.200508-1232SO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen RT, Canino GJ, Bird HR, et al. Area of residence, birthplace, and asthma in Puerto Rican children. Chest. 2007;131(5):1331–1338. doi: 10.1378/chest.06-1917. [DOI] [PubMed] [Google Scholar]
- 18.Sastry N, Ghosh-Dastidar B, Adams J, et al. The design of a multilevel survey of children, families, and communities: The Los Angeles Family and Neighborhood Survey. Soc Sci Res. 2006;35(4):1000–1024. [Google Scholar]
- 19.Peterson CE, Sastry N, Pebley AR, Ghosh-Dastidar B, Williamson S, Lara-Cinisomo S. The Los Angeles Family and Neighborhood Survey Codebook. RAND Labor and Population Working Paper. 2004 Mar; Available at: http://www.rand.org/pubs/drafts/DRU2400z2-1.html. [Google Scholar]
- 20.Asher MI, Keil U, Anderson HR, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8(3):483–491. doi: 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- 21.Koinis-Mitchell D, Sato AF, Kopel SJ, et al. Immigration and acculturation-related factors and asthma morbidity in Latino children. J Pediatr Psychol. 2011;36(10):1130–1143. doi: 10.1093/jpepsy/jsr041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dumanovsky T, Matte TD. Variation in adult asthma prevalence in Hispanic subpopulations in New York City. J Asthma. 2007;44(4):297–303. doi: 10.1080/02770900701344140. [DOI] [PubMed] [Google Scholar]
- 23.Carter-Pokras OD, Gergen PJ. Reported asthma among Puerto Rican, Mexican-American, and Cuban children, 1982 through 1984. Am J Pub Health. 1993;83(4):580–582. doi: 10.2105/ajph.83.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacobson JS, Mellins RB, Garfinkel R, et al. Asthma, body mass, gender, and Hispanic national origin among 517 preschool children in New York City. Allergy. 2008;63(1):87–94. doi: 10.1111/j.1398-9995.2007.01529.x. [DOI] [PubMed] [Google Scholar]
- 25.Mallol J, Sole D, Baeza-Bacab M, et al. Regional variation in asthma symptom prevalence in Latin American children. J Asthma. Aug;47(6):644–650. doi: 10.3109/02770901003686480. [DOI] [PubMed] [Google Scholar]
- 26.Choudhry S, Burchard EG, Borrell LN, et al. Ancestry-environment interactions and asthma risk among Puerto Ricans. Am J Respir Crit Care Med. 2006;174(10):1088–1093. doi: 10.1164/rccm.200605-596OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lind DL, Choudhry S, Ung N, et al. ADAM33 is not associated with asthma in Puerto Rican or Mexican populations. Am J Respir Crit Care Med. 2003;168(11):1312–1316. doi: 10.1164/rccm.200306-877OC. [DOI] [PubMed] [Google Scholar]
- 28.Salari K, Choudhry S, Tang H, et al. Genetic admixture and asthma-related phenotypes in Mexican American and Puerto Rican asthmatics. Genet Epidemiol. 2005;29(1):76–86. doi: 10.1002/gepi.20079. [DOI] [PubMed] [Google Scholar]
- 29.Martin MA, Shalowitz MU, Mijanovich T, Clark-Kauffman E, Perez E, Berry CA. The Effects of Acculturation on Asthma Burden in a Community Sample of Mexican American Schoolchildren. Am J Pub Health. 2007;97(7):1290–1296. doi: 10.2105/AJPH.2006.092239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Joseph SP, Borrell LN, Shapiro A. Self-reported lifetime asthma and nativity status in U.S. children and adolescents: results from the National Health and Nutrition Examination Survey 1999–2004. J Health Care Poor Underserved. 2010;21(2 Suppl):125. doi: 10.1353/hpu.0.0286. [DOI] [PubMed] [Google Scholar]
- 31.Holguin F, Mannino DM, Anto J, et al. Country of birth as a risk factor for asthma among Mexican Americans. Am J Respir Crit Care Med. 2005;171(2):103–108. doi: 10.1164/rccm.200402-143OC. [DOI] [PubMed] [Google Scholar]
- 32.Bostean G. Does Selective Migration Explain the Hispanic Paradox? A Comparative Analysis of Mexicans in the U.S. and Mexico. J Immigr Minor Health. 2013;15(3):624–635. doi: 10.1007/s10903-012-9646-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ceballos M. Simulating the effects of acculturation and return migration on the maternal and infant health of Mexican immigrants in the United States: a research note. Demography. 2011;48(2):425–436. doi: 10.1007/s13524-011-0017-4. [DOI] [PubMed] [Google Scholar]
- 34.Landale NS, Gorman BK, Oropesa RS. Selective migration and infant mortality among Puerto Ricans. Matern Child Health J. 2006;10(4):351–360. doi: 10.1007/s10995-006-0072-4. [DOI] [PubMed] [Google Scholar]
- 35.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11(3):496–518. [PubMed] [Google Scholar]
- 36.Javier JR, Wise PH, Mendoza FS. The relationship of immigrant status with access, utilization, and health status for children with asthma. Ambul Pediatr. 2007 Nov-Dec;7(6):421–430. doi: 10.1016/j.ambp.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 37.Akinbami LJ, Rhodes JC, Lara M. Racial and ethnic differences in asthma diagnosis among children who wheeze. Pediatrics. 2005;115(5):1254–1260. doi: 10.1542/peds.2004-0897. [DOI] [PubMed] [Google Scholar]
- 38.Patel MI, Schupp CW, Gomez SL, Chang ET, Wakelee HA. How do social factors explain outcomes in non-small-cell lung cancer among Hispanics in California? Explaining the Hispanic paradox. J Clin Oncol. 2013 Oct 1;31(28):3572–3578. doi: 10.1200/JCO.2012.48.6217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thomson EF, Nuru-Jeter A, Richardson D, Raza F, Minkler M. The Hispanic paradox and older adults’ disabilities: is there a healthy migrant effect? Int J Environ Res Public Health. 2013 May 3;10(5):1786–1814. doi: 10.3390/ijerph10051786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dinwiddie GY, Zambrana RE, Garza MA. Exploring risk factors in Latino cardiovascular disease: The role of education, nativity, and gender. Am J Public Health. 2013 Sep 12; doi: 10.2105/AJPH.2013.301280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Acevedo-Garcia D, Sanchez-Vaznaugh EV, Viruell-Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: a cross-national framework. Soc Sci Med. 2012;75(12):2060–2068. doi: 10.1016/j.socscimed.2012.04.040. [DOI] [PubMed] [Google Scholar]
- 42.Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol. 2009;123(6):1209–1217. doi: 10.1016/j.jaci.2009.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132(5 Suppl):757S–769S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]