Abstract
Background:
Health science students are at an increased risk of hepatitis A virus (HAV) infection even under accidental infection. The aims of this study were to assess the seroprevalence of HAV in 1st year medical students and to determine the risk factors of HAV vaccination program among this population.
Materials and Methods:
A cross-sectional study was conducted in autumn 2010. A total of 1028 newly admitted medical students in Isfahan, Kermanshah and Hamedan were included in the study. Participant data were obtained through predesigned data collection sheets. A serum sample was obtained for serologic testing for the presence of IgG anti-HAV using a commercially available enzyme-linked immunosorbent assay kit. Descriptive statistics, Chi-square and logistic regression tests were performed for statistical analysis and P < 0.05 was considered as significant.
Results:
The prevalence of HAV was detected in Isfahan, Hamedan, and Kermanshah newly admitted students 67.5%, 79.2%, and 50.6% respectively. There were significant relations between anti-HAV (IgG) positivity in drinking water and medical students provinces (P < 0.001, RR = 0.58 and 0.65 respectively). The household size did not significantly influence the anti-HAV (IgG) positivity in studied subjects (P = 0.09, RR = 1.26).
Conclusion:
Our results indicate that more than one-third of the medical students in all three faculties were seronegative for IgG anti-HAV and hence at an increased risk of developing HAV infection as a result of occupational exposure. Therefore, we suggest students in a health care set up should undergo vaccination against HAV after prevaccination immunity screening.
Keywords: Hepatitis A virus infection, medical students, seroprevalence
INTRODUCTION
Hepatitis A virus (HAV) is continues to be a serious health problem worldwide with an estimated 1.5 million cases annually.[1] HAV is a self-limited disease in adults that causes significant morbidity, with long absence from work for several weeks. Fulminant hepatitis leads to possible hospitalization and occasionally mortality.[2] Due to its widely asymptomatic forms of infection that is not reported, true incidence of the disease remains underestimated.[3] Different geographical distribution of HAV infection exists that correlates strictly with sanitary conditions and development indicators.[4] Prevalence of HAV rises along with aging and mainly effects lower socioeconomically population.[5]
Nosocomial hepatitis A infection is not common, but can easily spread by person to person contact in hospital conditions. The main causes of HAV infection risks in health care workers (HCW) and patients are transfusion of HAV infected blood products, infected food or water, contact of infected patients with HCW and through invasive procedures.[1,6] Medical students are at increased risk to get HAV from infected patients before acquiring awareness about safe-guarding themselves and expertness in many procedures; also these infected medical school students have contact with different patients during training.[1,7] Consequently seronegative or nonvaccinated medical school students are at increased risk for HAV infection. HAV vaccination defends HCW from this infection with potentially acute complications when acquired as an adult and prevents them from serving as a source for infecting patients.[8] In accordance with the reports of World Health Organization, Iran is an endemic region for this infection and the prevalence of hepatitis A disease is high.[4] In Iran, no proper periodic and age-specific seroprevalence data are available throughout the country and accurate epidemiological characteristics of HAV infection are unknown.[9,10]
Other various recent studies of HAV infection among seemingly healthy populations in different parts of Iran such as Tehran (85%), Golestan (99%) and Hormozgan (96%) were showed high prevalence of anti-HAV therefore; there was no need to prescribe immunoglobulin in the general population.[5] However, data collected in some recent studies exhibited lower rates of infection especially among children and adolescents.[9,10] In a similar recent study seroprevalence of HAV in 1st-3rd year Korean medical school students was 11.4% and the prevalence was increased with year of medical school, from 5.9% for 1st year to 14.5% for the 3rd year.[1] In other study that was performed on newly admitted students of Medical College in Bangladesh a total of 78% were seropositive for anti-HAV IgG.[11] Seroprevalence of anti-HAV among medical students of Turkey was detected 64%.[2]
In our country, the seroprevalence of hepatitis A disease among 1st year medical students, in relation with socio-economic status and hygiene has not yet been studied and recommendation or acceptable procedure for vaccination against HAV has not been provided. Therefore, this study was conducted to investigate the prevalence of HAV infection among 1st year medical school students of Isfahan, Hamedan, and Kermanshah universities of Iran and as a secondary objective, to determine the risk factors for acquisition of this infection.
PATIENTS AND METHODS
A cross-sectional study was conducted in autumn 2010. The target population was selected randomly from the newly admitted medical school students of three Iranian provinces at the time of registration. The three provinces were Isfahan central, Kermanshah western, and Hamedan north-central of Iran. The research protocol was approved by the Ethical Committee of Isfahan University of Medical Sciences in Iran (project numbers: 287269-71). Contributing in the study was voluntarily and subjects filled out consent forms. Subjects’ characteristics such as age, gender, source of drinking water and household size were also recorded in predesigned data collection sheets.
Laboratory procedures
Approximately, a volume of 5 ml of venous blood was collected from each participant. After separation by centrifugation, serum was stored in the laboratory at −20°C. IgG anti-HAV antibody was evaluated by enzyme-linked Immunosorbent Assay (DIAPRO Kit, Diagnostic Bio probes s.r.j). The principle of the assay is an indirect immunoenzymatic method of the sandwich type and steps of the test was performed according to the manufacturer recommendations. Any specimen with an absorbance more than the cut-off value (NP+NC/3) is considered as positive.
Statistical analysis
Statistical analysis was performed using SPSS software (Version 19, 2010, SPSS Inc., Chicago, IL, USA). Descriptive statistics and Chi-square were applied to assess the association between medical students’ characteristics and HAV seroprevalence. Mean and standard deviation were calculated for quantitative variables. Three studied variables (Province, Household, and source of drinking water) put into a logistic regression model with backward conditional method. Relative risks (RR) and 95% confidence intervals (CI) were calculated for each variable factor.
RESULTS
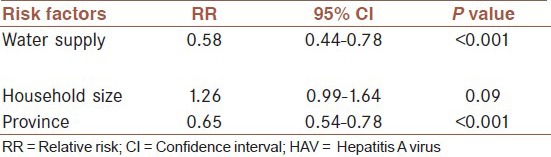
A total of 1028 newly admitted medical students from Isfahan University (n = 403) Hamden University (n = 365), and Kermanshah University (n = 260) were included in the study. The mean age of the participants was 19.6 ± 2.27 years (range: 17-27). The seropositivity of HAV in Isfahan, Hamedan, and Kermanshah newly admitted students were 67.5%, 79.2%, and 50.6% respectively. The prevalence of IgG anti-HAV in participants according to their characteristics is shown in Table 1. There were significant relation between anti-HAV (IgG) positivity with the source of drinking water and medical students provinces (P < 0.001). The household size did not significantly influence the anti-HAV (IgG) positivity in studied subjects (P = 0.09). Risk factors associated with anti-HAV IgG (+) in Logistic regression analysis, RR and 95% CI are shown in Table 2.
Table 1.
Prevalence of IgG anti-HAV in participants according to their characteristics
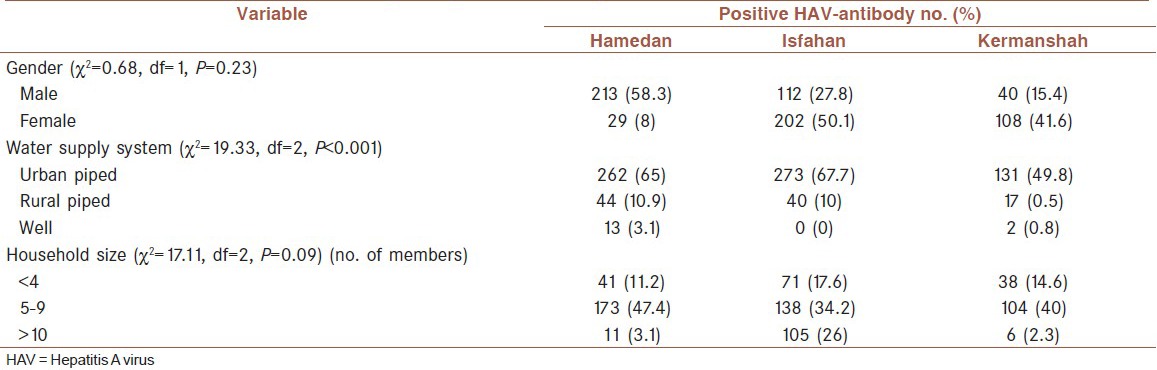
Table 2.
Risk factors associated with anti-HAV IgG (+) in logistic regression analysis
DISCUSSION
Several nosocomial HAV infection onsets are reported and the number of occupational cases of HAV infection is progressively expanding.[2] Some of the outbreaks have been reported from general wards.[12] Outbreaks are often related to collapse in infection control protocols. Close patient contact, suboptimal sanitary working situations, imperfect hand washing, abandoned glove use throughout exposure to body fluids and fecal incontinence of children can put HCW and medical students at increased risk for the illness.[7,13]
In our study, total antibodies against HAV were used as a representative marker for HAV infection among medical students. In compared seroprevalence of HAV among Medical College students of three cities, Kermanshah significantly showed the lowest (50.6%). Our results showed that large number of students, especially students of Kermanshah faculty, lacked natural immunity to HAV infection and were susceptible to the virus RR = 0.65. HAV vaccine is not included in the routine vaccination program in Iran; we guess that the average age for naturally acquired HAV infection will shift to older ages with changing incrementally life standard in our country. Therefore, the number of susceptible students in the next years might be increased.[2]
Entirely a slightly less seroprevalence was observed almost 2 decades in the Iranian general population.[5] HAV epidemiology is changing in the Middle East and Asia then prevalence patterns are shifting to lower rates of endemicity.[4] There is scanty data on HAV infection in medical students in our country. Previous findings indicates an epidemiological transition to lower rates of infection among the general population in some parts of the country (for instance a declining rate of HAV infection in Mazandaran from >90% in 2005 in the age group 18-30 year to 68.5% in 2012).[4,14] Most of the medical students of Kermanshah were native (urbanization). Such differences in seroprevalence might well be attributed to the wide variations in living situations (urbanization, health education, access to clean drinking water, improved sanitation, and lifestyle).[15] Drinking water is an important source of HAV transmission and the prevalence of anti-HAV IgG positivity in three faculties of Isfahan, Kermanshah, and Hamedan was detected with significantly lower rate in the students who were applied piped water in accordance with rural piped or well water (RR = 0.58; P < 0.001). In other previous studies source of drinking water and contaminated foods are considered as an important risk factor in hepatitis A infection.[14] In our study, the large number of household in medical students of these faculties were not associated with HAV seropositivity (RR = 1.26; P = 0. 09). The probable reason may be a considerable improvement in the standard of quality life and general health, even in distant rural regions with a large number household.[5] Although, in another similar study that was performed on students of Turkey a significant relation was shown between anti-HAV IgG positivity and an increasing number of family.[2] In our study, gender was not associated with anti-HAV positivity in three faculties. Furthermore, previous studies from Iran have not reported such an association in the general population.[5]
Our findings showed that more than 30% of the medical students are susceptible to HAV infection. Vaccination may be considered as a helpful restricted plan where a large part of adolescents or adults remain susceptible to HAV infection. Differently other preventative strategies, such as improving sanitation and health education along should be performed.[4] Other similar studies that were performed among 1st-3rd year medical students of Bangladesh and Korea showed about 80% and 11% seropositivity, respectively.[1,11] Making decisions for arrangement a HAV vaccination guideline is difficult. It depends on various variables such as disease burden, cost-benefit, cost-effectiveness, and vaccine efficacy.[14] Although universal vaccination of 12-16 year old children prior serologic testing is a cost-effective option.[16] The HAV seroprevalences of Isfahan (67.5%), and Kermanshah (50.6%) which we have observed in this study is not high and might justify a general vaccination program in newly admitted medical students. Nevertheless, the number of susceptible subjects who have no immunity also probability of hepatitis A among them might be increased in future.[4]
Since medical students and HCW are at high danger for nosocomial acute HAV infection because of long work hours and possible expose to HAV infected patients screening of medical students for seropositivity (especially in Kermanshah faculty) and vaccination of the nonimmune students should be considered before medical clerkship begins. However, additional studies on risk assessment for nosocomial HAV in hospitals and a cost-effectiveness analysis of HAV vaccination for medical school students are warranted.
Furthermore, it would be a useful source to establish the strategy of vaccination in this high risk group.
The restrictions of this study included assessment of hepatitis A infection only in newly admitted medical students, locally sample of students, information bias related to the use of the questionnaire and absence of information about the vaccination rate of HAV in our country.
CONCLUSION
This study revealed that more than one-third of the new entrants in three medical colleges were not immune to HAV infection and a decreased trend in this age group was shown. HAV vaccination after preimmunity screening should also be considered. Investigation of other risk factors of HAV infection such as a habit of taking food outside and hygienic practice will be more enlightening.
We suggest that mass screening of medical students for seropositivity and vaccination of the nonimmune students should be considered before medical clerkship begins. However, additional studies on risk assessment for nosocomial HAV in hospitals and a cost-effectiveness analysis of HAV vaccination for medical school students are warranted.
AUTHORS’ CONTRIBUTION
All authors have contributed in designing and conducting the study. BV, HR, PS, and MY collected the data and BA, MJ, and FKh did the analysis. All authors have assisted in preparation of the first draft of the manuscript or revising it critically for important intellectual content. All authors have read and approved the content of the manuscript and are accountable for all aspects of the work.
Footnotes
Source of Support: Nil
Conflict of Interest: The authors have no conflict of interest.
REFERENCES
- 1.Kim S, Lee JH, Hwang JH, Lee CS. Hepatitis A antibody seroprevalence among medical school students. Am J Infect Control. 2011;39:889–90. doi: 10.1016/j.ajic.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Oncu S, Oncu S, Sakarya S. Hepatitis A and B seropositivity among medical students. Health Policy. 2005;74:39–45. doi: 10.1016/j.healthpol.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Saberifiroozi M. Hepatitis A virus infection: Is it an important hazard to public health?: Hazards of HAV for public health. Hepat Mon. 2011;11:235–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Saffar MJ, Abedian O, Ajami A, Abedian F, Mirabi AM, Khalilian AR, et al. Age-specific seroprevalence of anti-hepatitis a antibody among 1-30 years old population of Savadkuh, Mazandaran, Iran with literature review. Hepat Mon. 2012;12:326–32. doi: 10.5812/hepatmon.6035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merat S, Rezvan H, Nouraie M, Abolghasemi H, Jamali R, Amini-Kafiabad S, et al. Seroprevalence and risk factors of hepatitis A virus infection in Iran: A population based study. Arch Iran Med. 2010;13:99–104. [PubMed] [Google Scholar]
- 6.Park JY, Lee JB, Jeong SY, Lee SH, Lee MA, Choi HJ. Molecular characterization of an acute hepatitis A outbreak among healthcare workers at a Korean hospital. J Hosp Infect. 2007;67:175–81. doi: 10.1016/j.jhin.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 7.Chodick G, Ashkenazi S, Aloni H, Peled T, Lerman Y. Hepatitis A virus seropositivity among hospital and community healthcare workers in Israel-the role of occupation, demography and socioeconomic background. J Hosp Infect. 2003;54:135–40. doi: 10.1016/s0195-6701(03)00124-5. [DOI] [PubMed] [Google Scholar]
- 8.Bonanni P, Bonaccorsi G. Vaccination against hepatitis B in health care workers. Vaccine. 2001;19:2389–94. doi: 10.1016/s0264-410x(00)00460-6. [DOI] [PubMed] [Google Scholar]
- 9.Montazam S, Kafshounchi M, Tanoumand A. Age-specific prevalence of antibodies to hepatitis A in rural and urban population of Malekan city. Med Sci J Islamic Azad Univ Tehran Med Branch. 2007;7:41–4. [Google Scholar]
- 10.Alian SH, Farhanian A, Noorani S. Sari: Mazandaran University Medical Sciences; 2006. Seroepidemiological evaluation of HAV among 1-25 years old general population in Sari of Mazandaranprovice [These for Medical Doctor] [Google Scholar]
- 11.Ahmed MS, Chowdhury OA, Khatoon M, Kabir F, Chowdhury AR, Jahan H. Seroprevalence of hepatitis virus antibodies in newly admitted students of Sylhet MAG Osmani Medical College. Bangladesh J Med Microbiol. 2009;3:20–6. [Google Scholar]
- 12.Skidmore SJ, Gully PR, Middleton JD, Hassam ZA, Singal GM. An outbreak of hepatitis A on a hospital ward. J Med Virol. 1985;17:175–7. doi: 10.1002/jmv.1890170210. [DOI] [PubMed] [Google Scholar]
- 13.Watson JC, Fleming DW, Borella AJ, Olcott ES, Conrad RE, Baron RC. Vertical transmission of hepatitis A resulting in an outbreak in a neonatal intensive care unit. J Infect Dis. 1993;167:567–71. doi: 10.1093/infdis/167.3.567. [DOI] [PubMed] [Google Scholar]
- 14.Jindal M, Rana SS, Gupta RK, Das K, Kar P. Serological study of hepatitis A virus infection amongst the students of a medical college in Delhi & evaluation of the need of vaccination. Indian J Med Res. 2002;115:1–4. [PubMed] [Google Scholar]
- 15.Movahedi M, Haghdoost AA, Pournik O, Hajarizadeh B, Fallah MS. Temporal variations of health indicators in Iran comparing with other Eastern Mediterranean Region countries in the last two decades. J Public Health (Oxf) 2008;30:499–504. doi: 10.1093/pubmed/fdn071. [DOI] [PubMed] [Google Scholar]
- 16.de Alencar Ximenes RA, Martelli CM, Merchán-Hamann E, Montarroyos UR, Braga MC, de Lima ML, et al. Multilevel analysis of hepatitis A infection in children and adolescents: A household survey in the Northeast and Central-west regions of Brazil. Int J Epidemiol. 2008;37:852–61. doi: 10.1093/ije/dyn114. [DOI] [PMC free article] [PubMed] [Google Scholar]


