Abstract
Given the FDA’s warning regarding the potential connection between suicidal behavior and antiepileptic drugs, this study examined methods by which to detect suicidal ideation in children with epilepsy. It compared the sensitivity, specificity, and area under the curve for identifying children with suicidal behavior using the Child Behavior Checklist (CBCL) and a structured psychiatric interview. Parent completed CBCLs provided behavior problem scores on 177 children with epilepsy, aged 5–16 years. Psychiatric diagnoses were made based on separate child and parent structured psychiatric interviews about the child. Children answered questions on suicidal behaviors during the interview. The clinically elevated CBCL Total Problems scale and having more than one psychiatric diagnosis, irrespective of type of diagnosis, were significant predictors and correctly classified children with suicidal ideation in 79% of the cases based on the CBCL and 80% of the cases with more than one psychiatric diagnosis. These findings indicate that elevated CBCL Total Problems scores, a commonly used instrument, can screen and identify risk for suicidal behavior in children with epilepsy. Additionally, irrespective of diagnosis, if a child with epilepsy has more than one psychiatric diagnosis, further assessment of suicidal behavior is warranted. Importantly, the results underscore the utility of having parents complete a questionnaire in the waiting room in order to identify children with epilepsy at risk for suicidal behavior.
Keywords: pediatric epilepsy, suicide, psychiatric disorders, behavior problems
1.0 INTRODUCTION
Among youth and young adults (aged 15–24 years) in the United States in 2010, suicide was the third leading cause of death, and approximately 4600 suicides were completed [1]. In children (aged 10–14 years) suicide was also the third leading cause of death; however, suicides in this age range continue to be rare (267 suicides in 2010 [1]). Since, suicide in youth is a significant public health problem, screening and identifying modifiable risk factors for suicidal behavior is a primary focus of efforts to reduce the number of suicides in youth [2]. A number of studies examined suicidal behavior among children and adolescents with physical disabilities or other chronic health conditions. Barnes et al. [3] reported that there was approximately a 20% increase in suicidal behavior (suicidal ideation and attempts) among children and adolescents with a chronic physical condition compared to healthy peers. Additionally, youth with a mental health condition alone and youth with both a physical condition and a mental health condition had similar rates of suicidal ideation. However, youth with both a mental health and physical condition were more likely to have a suicide attempt compared to those with a mental health condition alone. Everett-Jones and Lollar [4] found that high school students in the United States with physical disabilities or long-term health issues were 2.7 times more likely to seriously consider a suicide attempt, and 3.5 times more likely to make a suicide attempt compared to healthy high school students. In Denmark, Christiansen and Stenager [5] examined the association between attempted suicide in children and adolescents and a number of health conditions. These authors reported that epilepsy, asthma, insulin dependent diabetes mellitus, and malformations were significant medical condition risk factors for suicide attempts. After adjusting for confounding variables, they further concluded that children with a psychiatric history, low socioeconomic status, previous suicide attempts, and unstable medical conditions that resulted in hospital visits were primary risk factors for suicide attempts.
Suicidal behavior in adults with epilepsy has been studied more frequently, and there are very few studies examining suicidal behavior in children with epilepsy [6]. Caplan et al. [7] reported that children aged 5–16 years with either absence epilepsy (CAE) or complex partial seizures (CPS) endorsed suicidal ideation in 20% of the sample, and among those with suicidal ideation, 37% had a suicide plan, but there were no suicide attempts. Children with a combined disruptive disorder and an affective/anxiety disorder were 12 times more likely to endorse suicidal ideation. Rates of anxiety and depression alone were similar in the suicidal ideation group compared to the no suicidal ideation group. Additionally, only one third of the children with suicidal ideation ever received mental health treatment.
As a result of the FDA’s [8] recent warning regarding the potential connection between suicidal behavior and epilepsy medications, it is important to identify children with epilepsy at risk for suicidal behaviors. Utilizing the sample from Caplan et al. [7], this study examined methods by which to detect suicidal ideation in children with epilepsy. This study investigated the utility of detecting children at risk for suicidal ideation via a common parent completed behavioral questionnaire compared to the number of psychiatric diagnoses based on a structured psychiatric interview. This study examined the sensitivity, specificity, and area under the curve (AUC) of the questionnaire and number of psychiatric diagnoses based on a psychiatric interview about the child that was administered separately to the child and parent.
2.0 MATERIALS AND METHODS
2.1 Participants
The study included 177 children, aged 5–16 years, with a mean duration of epilepsy of 4.6 (SD 3.2) years. All children had IQ scores in the average range. Among the children with epilepsy, 36 (20.3%) reported suicidal ideation based on a semi-structured interview (See Procedures). Of the 36 children with epilepsy and suicidal ideation, 11 (30.56%) also had a suicide plan. None of the children had made a suicide attempt. Notably, 171 of these children were described in a previous paper on depression and anxiety in children with epilepsy [7].
Participants were recruited from tertiary and community sources; 49.2% of children from tertiary centers (e.g., University of California Los Angeles and University of Southern California clinics) and 50.8% of children from community sources (i.e. Los Angeles and Anaheim Kaiser Permanente, Los Angeles and San Diego Chapters of the Epilepsy Foundation of America, private practices). A pediatric neurologist at each recruitment site made a diagnosis of complex partial seizures (CPS) or childhood absence epilepsy (CAE) according to the International Classification of Epilepsy [9]. To be included in the study, each CPS participant had to have localization-related epilepsy and clinical manifestations of CPS. In addition to absence seizures induced by hyperventilation, each CAE participant had electroencephalogram (EEG) evidence of 3 Hz spike and wave. One pediatric neurology investigator (W.D.S.) from the University of California Los Angeles reviewed the history, EEG records, and diagnosis of each epilepsy participant from the recruitment sites. If there was no agreement with the diagnosis or EEG findings, the child was excluded from the study. We also excluded individuals with a mixed seizure disorder, previous epilepsy surgery, atypical spike and wave complexes, juvenile myoclonic epilepsy, structural MRI abnormality other than mesial temporal sclerosis (MTS), a neurological illness in addition to epilepsy, chronic medical illness, a metabolic disorder, a hearing disorder, mental retardation based on school/classroom placement or IQ < 70, and bilingual speakers of American English attending non-English speaking schools or not speaking English at home. None of the participants had MRI evidence of MTS.
The parents’ report and children’s medical records provided information on seizure frequency, AEDs, age of onset, illness duration, as well as the number of febrile convulsions and prolonged seizures (i.e., > 5 minutes).
Of the 107 children with CPS, 29 had no focal epileptic activity on EEGs conducted at the time of the initial epilepsy diagnosis; 25 had left, 21 right, 21 bilateral epileptic activity; and 59 had epileptic activity in the fronto-temporal region. EEGs were unavailable for 11 children with CPS; 28 children with CPS had background slowing, and 37 had secondary generalization. Of the 70 children with CAE, 11 had generalized tonic clonic convulsions, and 6 had background slowing.
Socioeconomic status was based on the parental occupational and educational status, using the Hollingshead two factor index [10]. Hollingshead levels I and II were classified as high and levels III-V were classified as low.
2.2 Procedures
After the procedures were fully explained, written informed consent and assent were obtained from parents and children, respectively. This study was approved by the Human Subjects Protection Committees of the University of California, Los Angeles.
Please see Caplan et al. [7] for a more detailed description of the study’s procedures. Children and parents were scheduled for a study visit, separate from an epilepsy or psychiatric clinic visit. Structured psychiatric interviews were administered separately to each child and parent about the child, and parents completed the CBCL questionnaires during the same visit.
2.2.1 Psychopathology
Kiddie Schedule for Affective Disorders and Schizophrenia–Present and Lifetime Version (K-SADS-PL) [11] was administered by a psychiatrist (RC) or a trained research assistant separately to each child and parent about the child. The child and parent often talked about the child’s seizures during the interview; as a result, the interviewers were not blinded with regard to seizure disorder diagnosis. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [12] were made based on information obtained both in the child and parent interviews. Current and lifetime diagnoses were examined.
A research assistant blind to the study goals abstracted the presence or absence of suicidal acts and ideation, both current and past, from the children’s responses to questions on suicidal acts and thoughts about death and dying (e.g., active and passive thoughts) in the depression section of the K-SADS-PL interview. Parents’ responses on the KSADS-PL to the suicide items were not examined, and only current suicidal ideation reported by the children was examined.
Due to findings reported in Caplan et al. [7] that indicated children with both disruptive and affective/anxiety diagnoses were more likely to have suicidal ideation compared to those with only one diagnosis, this study examined the presence or absence of any diagnosis as well as total number of psychiatric diagnoses as a primary indicator of severity of psychopathology.
2.2.2 Behavior/Emotional Problems
Parents completed the Childhood Behavioral Checklist (CBCL) [13] which is comprised of 20 social competence and 113 behavioral problem items. The CBCL generates a Total Problems scale as well specific narrow-band behavioral subscales (i.e., withdrawn, anxious/depressed, somatic complaints, attention problems, thought problems, social problems, delinquent behavior and aggressive behavior). The selected cut off point for borderline/clinically significant scores was 60 for the Total, Internalizing and Externalizing and 67 for the narrow band scores.
2.2.3 Data Analyses
Prior to statistical analyses, all data were inspected for outliers, skewness, and homogeneity of variance to ensure their appropriateness for parametric statistical tests. Children with and without suicidal ideation were compared on demographic and seizure-related measures using ttests for continuous variables and chi-square tests for categorical variables.
Controlling for those demographic and seizure-related variables that were significant between groups (children with and without suicidal ideation), separate logistic regressions were used to determine the association of CBCL scores and KSADS-PL measures with current presence of suicidal ideation in children with epilepsy. For CBCL scores, first the Total Problems score, then the broad band (Externalizing, Internalizing), followed by all the narrow-band scores (Anxious/Depressed, Withdrawn, Somatic Complaints, Social Problems, Thought Problems, Attention Problems, Aggressive Behavior, Delinquent Behavior) were investigated. For KSADS-PL, presence or absence of a psychiatric diagnosis current and lifetime, as well as number of KSADS-PL diagnoses were examined. Results were presented in terms of adjusted odds ratios and 95% confidence intervals, as well as areas under the ROC curve (AUC), sensitivity, and specificity. Area under the ROC curve (AUC) measures the ability of the instrument to correctly classify those with and without the condition as follows [14]: when one subject with the condition and one without the condition are drawn at random and the test is performed on both, the subject with the more abnormal test result should be the one with the condition. The area under the ROC curve is the percentage of randomly drawn pairs for which the test correctly classifies the two subjects in the random pair.
The sensitivity and specificity values presented were chosen to minimize the false negative rate while requiring the specificity to be at least 50%. The false negative rate was minimized as much as possible due to the clinical importance of “oversampling” when identifying a potentially lethal behavior. All tests were two-tailed and a significance level of 0.05 was adopted for all inferences.
3.0 RESULTS
Demographic information including IQ and seizure-related variables of children with and without suicidal ideation are presented in Tables 1 and 2 respectively. Gender, IQ, socioeconomic status, and ethnicity were not predictors of suicidal ideation. Children with suicidal ideation were more likely to be older (t (175) = 2.73, p=0.007) with a longer duration of epilepsy (t (173) = 2.81, p=0.005; controlling for age, t (172) = 1.79, p = .08). Children with suicidal ideation were in the following age ranges: 5 (13.9%) early childhood (aged 6–8 years), 23 (63.9%) middle childhood (aged 9–12), and 8 (23.2%) early adolescence (aged 13–16). The 11 children who indicated a plan were an average of 11.1 (SD 2.7; range 6.9–16.2) years old, with 2 (18.2%) in early childhood, 6 (54.5%) in middle childhood and 3 (27.3%) in early adolescence groups. Additionally, other seizure variables, including number of AEDs, were not significantly different in those with and without suicidal ideation.
Table 1.
Demographic Characteristics of Children with Epilepsy With and Without Suicidal Ideation
| Suicidal Ideation (N=36) |
No Suicidal Ideation (N=141) |
|
|---|---|---|
| Age (years; mean SD) | 11.31 (2.15)* | 9.94 (2.80) |
| Gender (n; %) | ||
| Male | 20 (55.56) | 60 (42.55) |
| Female | 16 (44.44) | 81 (57.45) |
| Socioeconomic Status (n; %) | ||
| High | 20 (55.56) | 80 (56.74) |
| Low | 16 (44.44) | 61 (43.26) |
| Ethnicity | ||
| Caucasian | 16 (44.44) | 77 (54.61) |
| Noncaucasian | 20 (55.56) | 64 (45.39) |
| IQ (mean ± SD) Full Scale | 93.1 (14.7) | 94.3 (14.5) |
t(175) = 2.73, p=0.007
Table 2.
Seizure Related Variables
| Suicidal Ideation (N=36) |
No Suicidal Ideation (N=141) |
|
|---|---|---|
| Duration (yrs.) | 5.88 (3.39)* | 4.22 (3.07) |
| Onset (yrs.) | 5.43 (3.25) | 5.66 (3.21) |
| Seizure Type | ||
| Complex Partial | 24 (66.67) | 83 (58.87) |
| Primary Generalized | 12 (33.33) | 58 (41.13) |
| Anti-epileptic drugs (n; %) | ||
| No Meds | 1 (2.78) | 12 (8.51) |
| Monotherapy | 28 (77.78) | 94 (66.67) |
| Polytherapy | 7 (19.44) | 35 (24.82) |
| Seizure Frequency (n; %) | ||
| =< 1 per year | 10 (27.78) | 47 (34.81) |
| 2–10 per year | 6 (16.67) | 27 (20.00) |
| > 10 per year | 20 (55.56) | 61 (45.19) |
| Prolonged seizures (n; %) | ||
| Yes | 14 (38.89) | 37 (26.62) |
| No | 22 (61.11) | 102 (73.38) |
| Febrile Seizures (n; %) | ||
| Yes | 8 (22.22) | 28 (20.29) |
| No | 28 (77.78) | 110 (79.71) |
t(173) = 2.81, p =.005; controlling for age, t(172) = 1.79, p = .08
3.1 Child Behavior Checklist
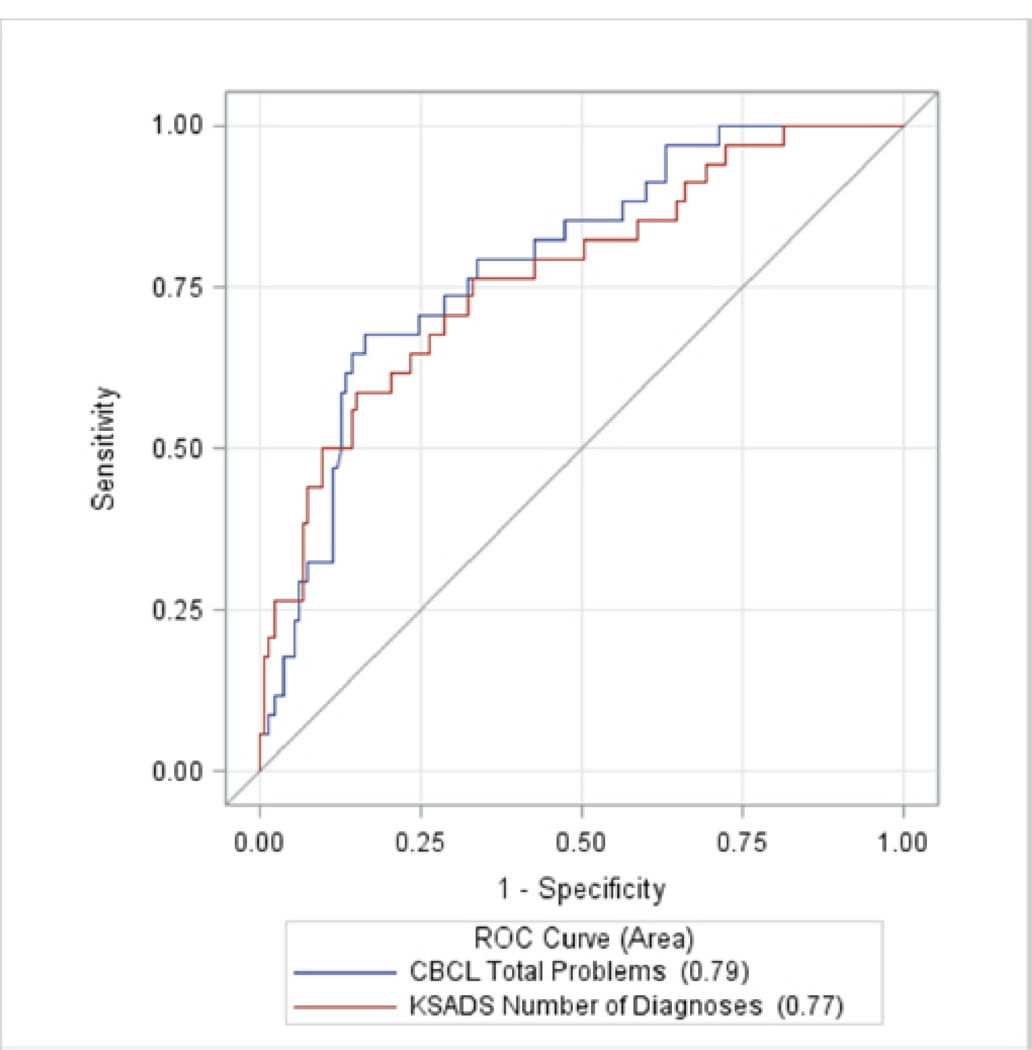
Logistic regression revealed that controlling for age and duration of epilepsy, children with an elevated Total Problems scale were over 5 times more likely to report suicidal ideation (OR, 5.6; 95% CI, 2.3–13.3). The area under the ROC curve (AUC) was 0.79 (sensitivity = 79.4 and specificity = 63.9) (Table 3, Figure 1). Using CBCL Externalizing and Internalizing Problems, the AUC was 0.77 (sensitivity = 70.6 and specificity = 67.7). Only the Internalizing scores were found to be significantly associated with suicidal ideation (OR = 3.6, 95% CI, 1.5–8.5). When examining all the narrow band scores simultaneously in the same model, the AUC was 0.84 (sensitivity = 79.4, specificity = 62.1). Only Thought Problems scaled scores were found to identify suicidal ideation (OR, 6.5; 95% CI, 1.8– 23.0). However, it should be noted that the narrow band scales were highly inter-related, with correlation coefficients ranging from r = .32 to .66 (p=.01 to <.0001). Hence, it was not valid to draw inferences regarding individual predictors from this model. Examining each of the narrow band scores individually, all of the scales except the Aggressive Behavior scale, were found to be significantly associated with suicidal ideation (ORs ranging from 2.5 to 12.3, AUCs ranging from 0.70 to 0.82, see Table 3). Importantly, item 91 of the CBCL, which asks parents if the child has talked of suicide, was also a significant predictor of suicidal ideation (OR = 14.0, 95%CI, 4.4–43.9), with AUC = .78 (sensitivity = 75.0 and specificity = 53.0).
Table 3.
Predictive Ability of CBCL and KSADS Models
| Instrument/Measures | AUC* | False Negative |
Sensitivity | Specificity |
|---|---|---|---|---|
| CBCL | ||||
| Total Problems | 0.79 | 7.6 | 79.4 | 63.9 |
| Broad-band Scores | ||||
| Internalizing | 0.77 | 9.2 | 79.4 | 51.9 |
| Externalizing | 0.72 | 13.0 | 64.7 | 60.2 |
| Internalizing & Externalizing | 0.77 | 10.0 | 70.6 | 67.7 |
| Narrow-band Scores | ||||
| All | 0.84 | 7.9 | 79.4 | 62.1 |
| Withdrawn/Depressed | 0.79 | 10.4 | 76.5 | 52.3 |
| Somatic Complaints | 0.72 | 13.1 | 67.6 | 55.3 |
| Anxious/Depressed | 0.75 | 12.8 | 70.6 | 51.5 |
| Delinquent Behavior | 0.73 | 12.7 | 70.6 | 52.3 |
| Thought Problems | 0.83 | 7.4 | 79.4 | 65.9 |
| Attention Problems | 0.74 | 11.5 | 73.5 | 52.3 |
| Social Problems | 0.74 | 11.3 | 67.6 | 65.2 |
| DSM-IV Diagnosis | ||||
| Any Diagnosis | 0.72 | 10.9 | 72.2 | 59.0 |
| Number of Diagnoses | 0.77 | 10.7 | 75.0 | 54.0 |
AUC (Area under ROC Curve)
Figure 1.
Area Under the ROC Curves for CBCL Total Problems and Number of KSADS-PL Diagnoses
3.2 KSADS-PL Diagnoses
Children with epilepsy and a KSADS-PL psychiatric diagnosis were significantly more likely to have suicidal ideation (OR = 2.9, 95% CI, 1.2–6.7, controlling for age and duration of epilepsy). AUC for this model was 0.72 (sensitivity = 72.2 and the specificity = 59.0). Taking into account the number of diagnoses, for each additional diagnosis, the likelihood of suicidal ideation increases by 80% (OR=1.8 (95%CI, 1.3–2.4). The AUC utilizing number of diagnoses was 0.77 (sensitivity = 75.0 and the specificity = 54.0) (Figure 1).
4.0 DISCUSSION
The CBCL parent report form is commonly used to screen children with epilepsy for behavior problems for clinical purposes and in research [15–20]. The results of this study indicated that clinically elevated scores on the CBCL Total Problems (AUC = .79) were a significant predictor of suicidal ideation in these children. These findings suggested that utilizing a screening tool that parents complete in the waiting room, was a reliable and valid way to identify children with epilepsy with significant suicidal risk. In a similar study of predictors of suicidal ideation and self-harm in adolescents in the general population, Shin et al. [21] found that suicidal ideation was related to Total Problems on the CBCL rather than to the broadband Externalizing or Internalizing Problems or to the narrowband scales. The authors hypothesized that the risk for suicidal ideation was related to an accumulation of problems and distress. Our findings also suggested that the CBCL provided information on a wide range of psychopathology related to suicidal ideation.
Psychiatric disorders are a prevalent complication for both children [7, 22–37] and adults [38–40] with epilepsy. The study findings highlight that those children with epilepsy who have more than one psychiatric diagnosis, based on a psychiatric interview, were at significant risk for suicidal ideation. When the number of psychiatric diagnoses were examined, for each additional diagnosis, the likelihood of suicidal ideation increased by 80%. As part of the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A), Nock et al. [41] reported that psychiatric disorders are a risk factor for suicidal behaviors. The NCS-A [41] study findings sound a warning by demonstrating that one third of adolescents with suicidal ideation went on to have a plan within 12 months and 60% of those with a plan made an attempt within 12 months.
Additionally the NCS-A [41] study demonstrated that major depression and/or dysthymia were the primary predictors of a suicide plan in adolescents who initially presented with suicidal ideation. The literature indicated that depressive disorders were quite prevalent among adults and youth with epilepsy [42–44]. Importantly, Barnes et al. [3] found that youth with both a mental health diagnosis plus physical condition were more likely to have a suicide attempt compared to a mental health condition alone. The combination of suicidal ideation and psychiatric diagnoses in the context of epilepsy may increase the vulnerability of youth with epilepsy for suicidal behavior.
Similarly, the adult epilepsy research literature identified the association among suicidal outcomes, epilepsy, and psychopathology. Pompili et al. [45] conducted a meta-analysis that indicated that suicide attempts and completed suicides are more prevalent among individuals with epilepsy compared to the general population. The authors identified risk factors that included psychiatric comorbidity, temporal lobe resections, anger, interictal dysphoric disorder, and previous suicide attempts. Interestingly, Hesdorffer et al. [46] reported that a suicide attempt increased the risk of an unprovoked seizure by 5 fold in adults and children over the age of 10. Harris and Barraclough [47] estimated that there was a fivefold increased risk for suicidal behavior if a person was diagnosed with epilepsy. The lifetime prevalence of suicide attempts and ideation ranges from 5% to 14% [48]. These findings clearly indicate that suicidal risk does not disappear in adulthood, but instead remains a significant issue in adulthood [6, 49, 50]
A significant implication of the FDA warning that AEDs increase the risk of suicidal ideation and behavior among people with epilepsy was that suicidal risk should be assessed in order to determine if medications should be discontinued and/or if a psychiatric evaluation and treatment is warranted [8]. The strong association between psychopathology, chronic illness, and suicidal ideation may reflect underdiagnosed and undertreated mental health issues in children and adolescents with epilepsy [43, 51]. Therefore, when youth with epilepsy are diagnosed with more than one psychiatric disorder and/or clinically elevated scores on the CBCL Total Problems are detected, an essential component of the evaluation should include an assessment of suicidal behavior.
Suicide remains the 3rd leading cause of death in the children aged 10–14, highlighting the importance of identifying and preventing suicidal behavior at younger age ranges [1]. Additionally, the findings of the NCS-A [41] study also indicate that providing assistance and interventions/treatment in the first year that the symptoms of suicidal behavior occur is of the utmost importance [41]. Until now, little was known about the initial presentation of suicidal behaviors in childhood epilepsy. Our study, however, provides evidence of sensitive predictors of suicidal ideation present in one quarter of children with chronic epilepsy. Given the short-term [41] and long term [52] potential for lethality, early identification of suicidal ideation and associated psychiatric disorders is essential to adequately treat and improve functioning and quality of life in children with epilepsy. Our findings demonstrate that the CBCL Total Behavior Problems scale is a useful tool for the detection of children with epilepsy with suicidal ideation.
4.1 Limitations
There are several limitations of this study. This study was not a population based study, and the sample was selected from tertiary care and community epileptologists, limiting its generalizability. The version of the CBCL [13] utilized in this study is not the most recent version as new norms and 6 items were changed in the most recent version [53]; however, the 1991 version has been used in a number of studies in epilepsy [54, 55]. Additionally, the CBCL has a significant cost barrier; however, there are opportunities available to utilize a computer based questionnaire with automatic scoring at a significantly reduced cost. This sample was young and none of the children had ever made a suicide attempt; as a result, the lethality of the suicidal information obtained in this study was quite low, making it impossible to link suicidal ideation to suicide attempts. However, suicidal thoughts are reported to be precursors to suicide attempts [56, 57]. Additionally, we did not examine family systems or suicidal behavior in family members behaviors [21, 38–40, 58–61], social and school problems, poor problem solving skills, and poor coping which are significant risk factors for suicidal behaviors [21, 58–60, 62].
5.0 CONCLUSIONS
Our findings demonstrate that children with clinically relevant CBCL Total Problems scale and more than one psychiatric diagnosis, irrespective of type of diagnosis, should be assessed to rule out suicidal ideation. In addition, the results underscore that a well-established easily administered questionnaire, correctly identified about three-fourths of children with epilepsy and suicidal ideation and missed one tenth of the children at risk. It is important to remember that suicidal ideation predicts subsequent suicidal behavior within a year in the general population of youth [41], and the high prevalence of suicidal behavior in adults with epilepsy emphasizes the importance of the identification and treatment of children with epilepsy at risk for suicidal behavior.
Highlights.
Suicidal ideation was present in 20% of children with chronic epilepsy.
Parent completed Child Behavior Checklist (CBCL) can be used to identify children with suicidal ideation.
CBCL Total Problems scale and/or more than one psychiatric diagnosis correctly identify children with suicidal ideation in 80% of the cases.
ACKNOWLEDGMENTS
The authors would like to thank the support of Erin Lanphier, PhD, Amy Mo, Caroline Bailey, PhD, Kimberly Smith, MA, Joanna Wu, and Sona Hovsepian. This study was supported by an NIH grant NS32070 (R. Caplan).
Abbreviations
- AED
Antiepileptic drug
- AUC
Area under the ROC Curve
- CAE
Childhood Absence Epilepsy
- CBCL
Child Behavior Checklist
- CPS
Complex Partial Seizures
- KSADS-PL
Kiddie Schedule for Affective Disorders and Schizophrenia–Present and Lifetime
- OR
Odds Ratio
- ROC
Receiver Operating Characteristic
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.CDC. Web-based Injury Statistics Query and Reporting Systerm (WISQARS) [Accessed June 7];2013 Available from: www.cdc.gov/ncipc/wisqars.
- 2.Summary of the practice parameters for the assessment and treatment of children and adolescents with suicidal behavior. J Am Acad Child Adolesc Psychiatry. 2001;40:495–499. doi: 10.1097/00004583-200104000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Barnes AJ, Eisenberg ME, Resnick MD. Suicide and self-injury among children and youth with chronic health conditions. Pediatrics. 2010;125:889–895. doi: 10.1542/peds.2009-1814. [DOI] [PubMed] [Google Scholar]
- 4.Everett Jones S, Lollar DJ. Relationship between physical disabilities or long-term health problems and health risk behaviors or conditions among US high school students. J Sch Health. 2008;78:252–257. doi: 10.1111/j.1746-1561.2008.00297.x. quiz 298-9. [DOI] [PubMed] [Google Scholar]
- 5.Christiansen E, Stenager E. Risk for attempted suicide in children and youths after contact with somatic hospitals: a Danish register based nested case-control study. J Epidemiol Community Health. 2012;66:247–253. doi: 10.1136/jech.2009.103887. [DOI] [PubMed] [Google Scholar]
- 6.Bell GS, Gaitatzis A, Bell CL, Johnson AL, Sander JW. Suicide in people with epilepsy: how great is the risk? Epilepsia. 2009;50:1933–1942. doi: 10.1111/j.1528-1167.2009.02106.x. [DOI] [PubMed] [Google Scholar]
- 7.Caplan R, Siddarth P, Gurbani S, Hanson R, Sankar R, Shields WD. Depression and anxiety disorders in pediatric epilepsy. Epilepsia. 2005;46:720–730. doi: 10.1111/j.1528-1167.2005.43604.x. [DOI] [PubMed] [Google Scholar]
- 8.FDA. Statistical Review and Evaluation: Antiepileptic drugs and suicidality. [Accessed June 6];2013 Available from: http://www.fda.gov/downloads/Drugs/Drugsafety/PostmarketDrugSafetyInformationforPatientsandProviders/UCM192556.pdf.
- 9.Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1989;30:389–399. doi: 10.1111/j.1528-1157.1989.tb05316.x. [DOI] [PubMed] [Google Scholar]
- 10.Hollingshead AB. Medical sociology: a brief review. Milbank Mem Fund Q Health Soc. 1973;51:531–542. [PubMed] [Google Scholar]
- 11.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Diagnostic and statistical manual of mental disorders: 4th (DSM-IV) ed. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- 13.Achenbach T. Manual for the Child Behavior Checklist and revised Child Behavior Profile. Burlington: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- 14.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 15.Oostrom KJ, Schouten A, Kruitwagen CL, Peters AC, Jennekens-Schinkel A. Behavioral problems in children with newly diagnosed idiopathic or cryptogenic epilepsy attending normal schools are in majority not persistent. Epilepsia. 2003;44:97–106. doi: 10.1046/j.1528-1157.2003.18202.x. [DOI] [PubMed] [Google Scholar]
- 16.Pinquart M, Shen Y. Behavior problems in children and adolescents with chronic physical illness: a meta-analysis. J Pediatr Psychol. 2011;36:1003–1016. doi: 10.1093/jpepsy/jsr042. [DOI] [PubMed] [Google Scholar]
- 17.Austin JK, Harezlak J, Dunn DW, Huster GA, Rose DF, Ambrosius WT. Behavior problems in children before first recognized seizures. Pediatrics. 2001;107:115–122. doi: 10.1542/peds.107.1.115. [DOI] [PubMed] [Google Scholar]
- 18.Austin JK, Perkins SM, Johnson CS, Fastenau PS, Byars AW, deGrauw TJ, Dunn DW. Behavior problems in children at time of first recognized seizure and changes over the following 3 years. Epilepsy & Behavior. 2011;21:373–381. doi: 10.1016/j.yebeh.2011.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oostrom KJ, van Teeseling H, Smeets-Schouten A, Peters AC, Jennekens-Schinkel A. Three to four years after diagnosis: cognition and behaviour in children with 'epilepsy only'. A prospective, controlled study. Brain. 2005;128:1546–1555. doi: 10.1093/brain/awh494. [DOI] [PubMed] [Google Scholar]
- 20.van Mil SG, Reijs RP, van Hall MH, Snoeijen SM, de la Parra NM, Aldenkamp AP. Behavior in children with cryptogenic localization related epilepsy: a follow-up study. Pediatr Neurol. 2010;42:107–110. doi: 10.1016/j.pediatrneurol.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 21.Shin YM, Chung YK, Lim KY, Lee YM, Oh EY, Cho SM. Childhood predictors of deliberate self-harm behavior and suicide ideation in korean adolescents: a prospective population-based follow-up study. J Korean Med Sci. 2009;24:215–222. doi: 10.3346/jkms.2009.24.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adewuya AO, Ola BA, Okeniyi JAO. Psychiatric morbidity in Nigerian adolescents with epilepsy. Journal of Pediatric Neurology. 2005;3:153–158. [Google Scholar]
- 23.Alwash RH, Hussein MJ, Matloub FF. Symptoms of anxiety and depression among adolescents with seizures in Irbid, Northern Jordan. Vol. 9. Seizure: The Journal Of The British Epilepsy Association; 2000. pp. 412–416. [DOI] [PubMed] [Google Scholar]
- 24.Baki O, Erdogan A, Kantarci O, Akisik G, Kayaalp L, Yalcinkaya C. Anxiety and depression in children with epilepsy and their mothers. Epilepsy & Behavior. 2004;5:958–964. doi: 10.1016/j.yebeh.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 25.Dunn DW, Austin JK, Huster GA. Symptoms of depression in adolescents with epilepsy. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1132–1138. doi: 10.1097/00004583-199909000-00017. [DOI] [PubMed] [Google Scholar]
- 26.Caplan R, Siddarth P, Gurbani S, Ott D, Sankar R, Shields WD. Psychopathology and pediatric complex partial seizures: seizure-related, cognitive, and linguistic variables. Epilepsia. 2004;45:1273–1281. doi: 10.1111/j.0013-9580.2004.58703.x. [DOI] [PubMed] [Google Scholar]
- 27.Caplan R, Siddarth P, Stahl L, Lanphier E, Vona P, Gurbani S, Koh S, Sankar R, Shields WD. Childhood absence epilepsy: Behavioral, cognitive, and linguistic comorbidities. Epilepsia. 2008;49:1838–1846. doi: 10.1111/j.1528-1167.2008.01680.x. [DOI] [PubMed] [Google Scholar]
- 28.Ettinger AB, Weisbrot DM, Nolan EE, Gadow KD, Vitale SA, Andriola MR, Lenn NJ, Novak GP, Hermann BP. Symptoms of depression and anxiety in pediatric epilepsy patients. Epilepsia. 1998;39:595–599. doi: 10.1111/j.1528-1157.1998.tb01427.x. [DOI] [PubMed] [Google Scholar]
- 29.Gonzalez-Heydrich J, Dodds A, Whitney J, MacMillan C, Waber D, Faraone SV, Boyer K, Mrakotsky C, DeMaso D, Bourgeois B, Biederman J. Psychiatric disorders and behavioral characteristics of pediatric patients with both epilepsy and attention-deficit hyperactivity disorder. Epilepsy & Behavior. 2007;10:384–388. doi: 10.1016/j.yebeh.2007.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones JE, Siddarth P, Gurbani S, Shields WD, Caplan R. Cognition, academic achievement, language, and psychopathology in pediatric chronic epilepsy: Short-term outcomes. Epilepsy & Behavior. 2010;18:211–217. doi: 10.1016/j.yebeh.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jones JE, Watson R, Sheth R, Caplan R, Koehn M, Seidenberg M, Hermann B. Psychiatric comorbidity in children with new onset epilepsy. Developmental Medicine & Child Neurology. 2007;49:493–497. doi: 10.1111/j.1469-8749.2007.00493.x. [DOI] [PubMed] [Google Scholar]
- 32.Loney JC, Wirrell EC, Sherman EM, Hamiwka LD. Anxiety and depressive symptoms in children presenting with a first seizure. Pediatr Neurol. 2008;39:236–240. doi: 10.1016/j.pediatrneurol.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 33.Margalit M, Heiman T. Anxiety and self-dissatisfaction in epileptic children. International Journal of Social Psychiatry. 1983;29:220–224. doi: 10.1177/002076408302900308. [DOI] [PubMed] [Google Scholar]
- 34.Oğuz A, Kurul S, Dirik E. Relationship of epilepsy-related factors to anxiety and depression scores in epileptic children. Journal of Child Neurology. 2002;17:37–40. doi: 10.1177/088307380201700109. [DOI] [PubMed] [Google Scholar]
- 35.Ott D, Caplan R, Guthrie D, Siddarth P, Komo S, Shields WD, Sankar R, Kornblum H, Chayasirisobhon S. Measures of psychopathology in children with complex partial seizures and primary generalized epilepsy with absence. Journal Of The American Academy Of Child And Adolescent Psychiatry. 2001;40:907–914. doi: 10.1097/00004583-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Roeder R, Roeder K, Asano E, Chugani HT. Depression and mental health help-seeking behaviors in a predominantly African American population of children and adolescents with epilepsy. Epilepsia. 2009;50:1943–1952. doi: 10.1111/j.1528-1167.2009.02046.x. [DOI] [PubMed] [Google Scholar]
- 37.Williams J, Steel C, Sharp GB, DelosReyes E, Phillips T, Bates S, Lange B, Griebel ML. Anxiety in children with epilepsy. Epilepsy & Behavior: E&B. 2003;4:729–732. doi: 10.1016/j.yebeh.2003.08.032. [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Lane MC, Shahly V, Stang PE. Accounting for comorbidity in assessing the burden of epilepsy among US adults: results from the National Comorbidity Survey Replication (NCS-R) Mol Psychiatry. 2011 doi: 10.1038/mp.2011.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.LaFrance WC, Jr, Kanner AM, Hermann B. Psychiatric comorbidities in epilepsy. International Review Of Neurobiology. 2008;83:347–383. doi: 10.1016/S0074-7742(08)00020-2. [DOI] [PubMed] [Google Scholar]
- 40.Swinkels WAM, Kuyk J, van Dyck R, Spinhoven P. Psychiatric comorbidity in epilepsy. Epilepsy & Behavior. 2005;7:37–50. doi: 10.1016/j.yebeh.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 41.Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fiest KM, Dykeman J, Patten SB, Wiebe S, Kaplan GG, Maxwell CJ, Bulloch AG, Jette N. Depression in epilepsy: a systematic review and meta-analysis. Neurology. 2013;80:590–599. doi: 10.1212/WNL.0b013e31827b1ae0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics. 2012;129:256–264. doi: 10.1542/peds.2010-1371. [DOI] [PubMed] [Google Scholar]
- 44.Maryam S, Parviz B. Depression in children and adolescents with epilepsy: a 15 year research review of prevalence, and demographic and seizure related correlates. Iran J Pediatr. 2013;23:1–7. [PMC free article] [PubMed] [Google Scholar]
- 45.Pompili M, Girardi P, Ruberto A, Tatarelli R. Suicide in the epilepsies: a meta-analytic investigation of 29 cohorts. Epilepsy Behav. 2005;7:305–310. doi: 10.1016/j.yebeh.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 46.Hesdorffer DC, Hauser WA, Olafsson E, Ludvigsson P, Kjartansson O. Depression and suicide attempt as risk factors for incident unprovoked seizures. Ann Neurol. 2006;59:35–41. doi: 10.1002/ana.20685. [DOI] [PubMed] [Google Scholar]
- 47.Harris EC, Barraclough B. Suicide as an outcome for mental disorders: A meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 48.Robertson M. Suicide, parasuicide, and epilepsy. In: Engel J, Pedley TA, editors. Epilepsy: A comprehensive textbook. Philadelphia: Lippincott Raven; 1997. pp. 2141–2151. [Google Scholar]
- 49.Hesdorffer DC, Ishihara L, Mynepalli L, Webb DJ, Weil J, Hauser WA. Epilepsy, suicidality, and psychiatric disorders: a bidirectional association. Ann Neurol. 2012;72:184–191. doi: 10.1002/ana.23601. [DOI] [PubMed] [Google Scholar]
- 50.Pompili M, Girardi P, Tatarelli R. Death from suicide versus mortality from epilepsy in the epilepsies: a meta-analysis. Epilepsy Behav. 2006;9:641–648. doi: 10.1016/j.yebeh.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 51.Ott D, Siddarth P, Gurbani S, Koh S, Tournay A, Shields WD, Caplan R. Behavioral disorders in pediatric epilepsy: unmet psychiatric need. Epilepsia. 2003;44:591–597. doi: 10.1046/j.1528-1157.2003.25002.x. [DOI] [PubMed] [Google Scholar]
- 52.Brezo J, Paris J, Barker ED, Tremblay R, Vitaro F, Zoccolillo M, Hebert M, Turecki G. Natural history of suicidal behaviors in a population-based sample of young adults. Psychol Med. 2007;37:1563–1574. doi: 10.1017/S003329170700058X. [DOI] [PubMed] [Google Scholar]
- 53.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families; 2001. [Google Scholar]
- 54.Drewel EH, Bell DJ, Austin JK. Peer difficulties in children with epilepsy: association with seizure, neuropsychological, academic, and behavioral variables. Child Neuropsychol. 2009;15:305–320. doi: 10.1080/09297040802537646. [DOI] [PubMed] [Google Scholar]
- 55.Rodenburg R, Stams GJ, Meijer AM, Aldenkamp AP, Dekovic M. Psychopathology in children with epilepsy: a meta-analysis. J Pediatr Psychol. 2005;30:453–468. doi: 10.1093/jpepsy/jsi071. [DOI] [PubMed] [Google Scholar]
- 56.Beck AT, Brown GK, Steer RA, Dahlsgaard KK, Grisham JR. Suicide ideation at its worst point: a predictor of eventual suicide in psychiatric outpatients. Suicide Life Threat Behav. 1999;29:1–9. [PubMed] [Google Scholar]
- 57.Miller TR, Taylor DM. Adolescent suicidality: who will ideate, who will act? Suicide Life Threat Behav. 2005;35:425–435. doi: 10.1521/suli.2005.35.4.425. [DOI] [PubMed] [Google Scholar]
- 58.Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: risks and protectors. Pediatrics. 2001;107:485–493. doi: 10.1542/peds.107.3.485. [DOI] [PubMed] [Google Scholar]
- 59.Peter T, Roberts LW, Buzdugan R. Suicidal ideation among Canadian youth: a multivariate analysis. Arch Suicide Res. 2008;12:263–275. doi: 10.1080/13811110802100882. [DOI] [PubMed] [Google Scholar]
- 60.Sourander A, Klomek AB, Niemela S, Haavisto A, Gyllenberg D, Helenius H, Sillanmaki L, Ristkari T, Kumpulainen K, Tamminen T, Moilanen I, Piha J, Almqvist F, Gould MS. Childhood predictors of completed and severe suicide attempts: findings from the Finnish 1981 Birth Cohort Study. Arch Gen Psychiatry. 2009;66:398–406. doi: 10.1001/archgenpsychiatry.2009.21. [DOI] [PubMed] [Google Scholar]
- 61.Keilp JG, Gorlyn M, Oquendo MA, Burke AK, Mann JJ. Attention deficit in depressed suicide attempters. Psychiatry Res. 2008;159:7–17. doi: 10.1016/j.psychres.2007.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dervic K, Brent DA, Oquendo MA. Completed suicide in childhood. Psychiatr Clin North Am. 2008;31:271–291. doi: 10.1016/j.psc.2008.01.006. [DOI] [PubMed] [Google Scholar]