Abstract
Rabies remains endemic in Peru. In 1983, Latin America and the Caribbean promised to eliminate canine-transmitted rabies from the continent. This led to Peru introducing a multidisciplinary public health system for controlling and managing rabies across the country. The system consists of mass canine vaccination campaigns, post exposure prophylaxis and monitoring aggressor animals for signs of rabies. The Peruvian city of Trujillo, La Libertad, is an urban area where dogs are the principal reservoir for rabies. The disease burden of rabies in Trujillo, La Libertad is currently minimal, with no rabies cases in humans for over 10 years, and only three canine cases. No human deaths due to rabies have occurred for several decades. From this it can be inferred that antirabies systems such as this do have real effects in reducing cases of human rabies at a grass roots level.
Keywords: Rabies, Trujillo, Peru, Public Health, canine vaccination, post-exposure prophylaxis, aggressor animal observation
Introduction
Trujillo, in the district of La Libertad, is Peru’s third largest city1 (Figure 1). Rabies is historically endemic here,2 as it remains in parts of Peru today.3 In 1983 Latin America and the Caribbean (LAC), aided by the Pan American Health Organisation (PAHO: the regional office of the World Health Organisation) pledged to eliminate canine transmitted rabies from the continent by 2005.3,4 This led to the introduction of national programmes for the management and control of rabies in LAC. Peru’s programme was implemented nationally, including in Trujillo, La Libertad. Here we examine this system, and discuss its effects in Trujillo, as well as in Peru and LAC.
Figure 1.

Map of Trujillo, La Libertad, Peru (produced by C Seneschall).
Background Information on Rabies
Worldwide, the disease burden of rabies remains significant. Rabies is listed as one of the World Health Organisation’s (WHO) Neglected Tropical Diseases.5 It results in around 55 000 deaths worldwide annually,5 chiefly in Asia and Africa,5 and is present in over 150 countries and territories around the world.
The causative agent of rabies is the rabies virus (RABV), which itself has several genotypes.6,7 This is a single, negative sense strand RNA virus of the Lyssavirus genus and Rhabdoviridae family.6 In humans, it results in an encephalomyelitis that is usually fatal.5 This presents chiefly in two ways: furious rabies (80% of cases) and paralytic rabies (20%).8 In furious rabies, the patient develops the ‘classical’ symptoms of rabies, which include fluctuating consciousness, hyperexcitability, and signs of autonomic stimulation.7,8 In paralytic rabies, a flaccid paralysis ascending from the bitten limb develops.8
Rabies is a zoonotic disease, transmitted only by and within mammals.6,9 In the majority of cases the transmission of the rabies virus between animals occurs via bites.6 Worldwide, over 90% of rabies transmitted to humans is due to bites from infected dogs.8 Other animals involved in transmitting rabies to humans include haematophagous bats, foxes and raccoons.8
Rabies and its Management in Trujillo
Due to Trujillo’s urban setting and its climate, canine transmitted rabies is historically the sole significant cause of human rabies in the area.2 As in other developing countries, stray dogs in particular serve as an important reservoir. Rabies can be transmitted from a stray dog to a human either by biting a human directly, or by biting a domestic dog which then bites a human. This is known as rabies ‘spilling’ into the domestic dog population.10 In developing countries in general, the domestic dog is the main direct source of rabies for humans.10 Due to this, and to clear practical difficulties with controlling rabies within the stray dog population, any public health programme seeking to control rabies in Trujillo must therefore seek to control rabies in the domestic dog population.
The protocol for rabies management in Peru is described in the Guidelines for the Prevention and Management of Rabies in Peru, 20082 (‘Norma Técnica de Salud para la Prevención y Control de Rabia Humana en el Perú; 2008’). An overview of this programme can be seen in Figure 2. Rabies is managed in Trujillo according to these guidelines, which are produced by the Peruvian Ministry of Health (Ministerio de Salud).
Figure 2.
Rabies management in Peru, both in the immediate aftermath of a dog bite, and the multidisciplinary public health approach to control the total amount of rabies in the population.2
Managing the aftermath of a dog bite
Managing the human victim
After suffering a dog bite, the human victim is advised to attend the emergency department of a local hospital. In Trujillo, these hospitals include Hospital Regional Docente de Trujillo (HRDT) and Hospital Belén. Here, the wound is washed liberally with saline or water. This decreases the viral load, and hence the risk of rabies transmission. Unless blood loss from the wound is very severe, it is not sutured, as suturing has been shown to increase the risk of contracting rabies.11 Instead the wound is covered. The need for rabies post-exposure prophylaxis and if so what type is then considered.
Wound assessment regarding the need for rabies immunoglobulin administration
The patient’s need for rabies immunoglobulin (RIG) is assessed by an epidemiology specialist. There are four independent factors which determine this. The first is the time since the dog bite. Peruvian guidelines state that RIG should be administered as soon as possible, but only if the bite has occurred within the past 7 days.5 The second is the wound itself: that is, its location, size, and the number of bites. Large, deep or multiple bites, or those located on the head, neck or finger tips carry increased risk for rabies transmission.2 The third factor is the risk of the aggressor animal being infected with the rabies virus. A full history taken from the patient and/or another witness is used to assess this. Stray animals and those reported as displaying signs of rabies are considered high risk. Finally, the individual risk of the patient contracting rabies is considered. Previous history of rabies vaccination or RIG administration decrease the patient’s risk. If the bite has occurred in the past week, both the wound and the animal are considered high risk of transmitting rabies, and the patient has had no previous rabies prophylaxis, then RIG is given.2 In Trujillo, only HRDT administers RIG, whereas the active rabies post exposure prophylaxis vaccinations are available more widely. The one week window for receiving RIG helps minimise risks resulting from this limited availability.
Two preparations of RIG are used: equine rabies immunoglobulin (ERIG), at a dose of 40 IU/kg body weight or human rabies immunoglobulin (HRIG), at 20 IU/kg body weight.12 Exceeding this dose may interfere with the body’s immune response to the rabies vaccine.3 Both preparations are given as a single dose, directly inside the wound(s) where possible. If this is not possible, or if there is any vaccine leftover, then RIG should be given intramuscularly (IM) into the gluteal region.12
Rabies Post Exposure Prophylaxis
Patients with high risk bites also receive active rabies post-exposure prophylaxis vaccination, in addition to the anti-rabies immunoglobulin.2 Two vaccine preparations are used: the lactating rat brain (LRB) vaccine and the cell culture (CC) vaccine. Despite recent guidance from the WHO stating that the LRB vaccine should no longer be used, due to increased risk of disability,13 it is included in the 2008 Peruvian guidelines and is currently still used in Trujillo. Health professionals in Trujillo report that they consider both vaccine preparations to be equivalent. The protocol for the LRB vaccine is 14 doses of 2 ml (20 mg), uninterrupted and daily starting on the day of initial presentation to the hospital, followed by 2 refresher doses 10 and 20 days after the last vaccination. All doses are given subcutaneously into the periumbilical region. The regimen for the cell culture vaccine is 5 doses given on days 0, 3, 7, 14 and either 21 or 28. These are given intramuscularly into the deltoid. If the patient has finished a course of rabies vaccination within the past 12 months, the patient is given a refresher dose of the vaccine. For the LRB vaccine this is 3 doses, one every 3 days. For the CC vaccine this is 2 doses, the first on day 0 and the second on day 3.2
Post-exposure prophylaxis in lower risk rabies wounds
For patients who received wounds considered lower risk of rabies transmission, RIG is not given. Instead, the patient receives only the rabies vaccine. For the cell culture vaccination, this is the same as the protocol above. For the LRB vaccine, this is a reduced regimen of 7 doses, 1 given each consecutive day and then three refresher doses 10, 20 and 60 days after the last vaccination.2
Patients who solely came into contact with the saliva of an animal, but were not bitten, have an even lower risk of contracting rabies.2 If the animal is not suspected of having rabies, no post-exposure prophylaxis is given. If the animal is stray or shows signs of rabies, then the patient is started on the regimen of the rabies post-exposure prophylaxis vaccination detailed for lower risk bites.2
Managing the aggressor animal
After biting a human, the aggressor animal (if known) is observed for ten days. This can occur in quarantine. More often, a trained veterinarian is sent to see the aggressor animal in its home environment. There are three visits: immediately, and five and ten days after the attack. These intervals are chosen as the rabies virus can be found in the salivary glands of an animal up to 7 days before the animal becomes symptomatic,2,14 and the symptomatic phase of the illness generally lasts 2–6 days.2 If the animal dies whilst under surveillance, its brain is removed for laboratory examination. If there are no signs of rabies, the dog is released back to its owner after receiving a pre-exposure prophylaxis vaccination.
Clear documentation is kept of all incidents of dog bites; both details of the human victim, the aggressor dog and any vaccinations/other treatments given.2,3
Public Health Measures for Limiting Transmission of Rabies from Dogs to Humans
As discussed above, most rabies in developing countries is transmitted via domestic dogs and it is difficult to control rabies within the stray dog population. To prevent the domestic dog population from serving either as a reservoir or as a vector between the stray dog reservoir and humans, domestic dogs are mass vaccinated. Mass vaccinations occur during annual vaccination campaigns.2 In Trujillo, these last between 8 and 10 days. Centres are set up for members of the public to bring their dogs, and officials travelling door-to-door also give vaccinations. An estimation of the canine population is made prior to the campaign. In order to ensure adequate protection against rabies from a public health perspective, 80% of the dogs in the area must be vaccinated.2 In Trujillo, this is closer to 90%. The vaccination is either a LRB vaccine or a cell culture vaccine made from baby hamster kidney (BHK) cells. The vaccine has been shown to last one year,15 meaning that annual vaccination is essential regardless of prior prophylaxis. It can be given to all dogs greater than three months of age. Each dog which receives a pre-exposure prophylaxis receives a certificate to prove their immunity.
It should be noted that Peru’s national campaign for controlling rabies does not include the culling of stray dogs.2 In Trujillo, anecdotal evidence from local epidemiologists reports that culling did occur until 1988, but is no longer practiced.
Pre-exposure prophylaxis in humans
Pre-exposure vaccination of humans against rabies is not a routine public health measure.2 Members of the public who are at an increased risk of contracting rabies are given pre-exposure rabies prophylaxis. These include doctors, vets, and those who work in the antirabies centres, where aggressor animals are quarantined. The pre-exposure prophylaxis is 4 subcutaneous doses of the LRB vaccine. If these humans are later bitten by a possibly rabid animal, only the reduced dose of the vaccine is required.2
Costs
All vaccines mentioned above are supplied free of charge to the patient or dog owner and to the distributor, from the government. Vaccinations are ordered from the government, and are readily available.2,3
Reporting
Human rabies is a Group 1 notifiable disease in Peru.2 Immediate notification is obligatory, and this must occur within 24 hours of gaining knowledge about a case. Information is passed in a hierarchical chain to a superior authority until it reaches PAHO’s Regional Information System for Epidemiological Surveillance of Rabies16 (SIRVERA - Sistema de Informação Regional para a Vigilância Epidemiológica da Raiva). Regarding human rabies, either a clinically suspected or laboratory confirmed case is reported. Rabies in other animals also requires obligatory notification, but a confirmed laboratory diagnosis is needed before it can be reported.
Current Disease Burden of Rabies in Trujillo, La Libertad, Peru and Lac
Rabies is currently controlled in Trujillo
When regarding the outcome measure of human mortality due to rabies, patient records show that no humans have died of rabies in Trujillo in decades. Anecdotal evidence states that in 1986, when a rabid dog bit 6 people in Trujillo, all survived due to appropriate wound management and timely post-exposure prophylaxis. This provides evidence of how the programme’s rabies management protocol can be effective in reducing human mortality.
According to SIRVERA,16 there have been no reported cases of rabies in humans in Trujillo or the entire region of La Libertad in the past 10 years. Similarly, there have only been three cases of canine rabies in La Libertad within the past 10 years (1 case in 2003 and 2 in 2004). There have been no cases of rabies in any other animals within the past 10 years (Figure 3). These data show that rabies in La Libertad is successfully controlled. As rabies was previously endemic in La Libertad2 it suggests that this decrease is at least in part due to the introduction of the public health programme, providing evidence that in urban areas like Trujillo, La Libertad, where dogs are the sole significant reservoir for rabies,2 the mass canine vaccination campaigns of the domestic dog population are successful at limiting rabies cases in both humans and animals. In addition to this, Trujillo – and the whole of La Libertad – is currently classed as a non-productive area for rabies (Área no productiva) by the Peruvian Ministry of Health,2 as there have been no rabies cases in either humans or domestic animals for the past 2 years.
Figure 3.
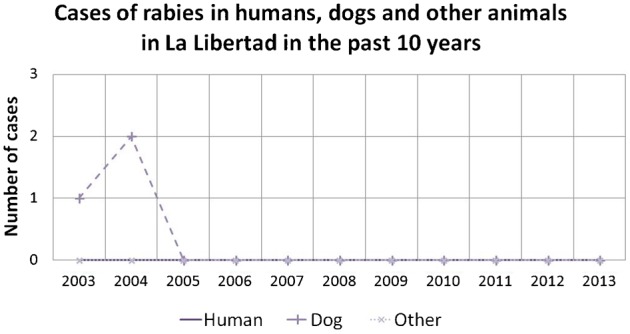
Cases of rabies in humans and other animals in La Libertad have been negligible in the past 10 years. Data: SIRVERA (Panaftosa–PAHO/WHO).16
Figure 4.
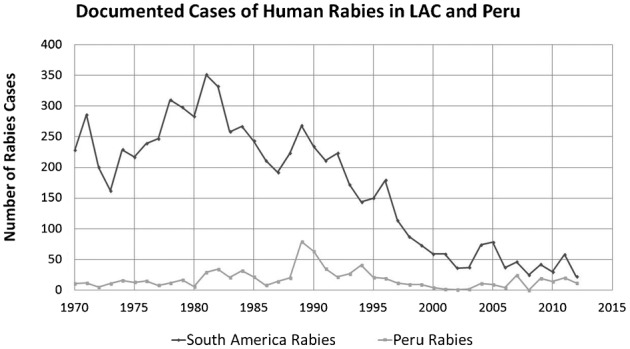
Human rabies cases in Latin America and the Caribbean (LAC) have decreased since 1970, whilst remaining constant in Peru. Data: SIRVERA (Panaftosa–PAHO/WHO).16
Human Rabies remains endemic and problematic in Peru, despite the national antirabies campaign
Human rabies cases in Peru have remained relatively constant since prior to the programme’s introduction. Despite the public health system implemented in Peru, documented annual cases of human rabies have remained at around 15 cases per year since 1970. Possible explanations for this include the impact of rural rabies transmission in Peru, chiefly via haematophagous bats,3 which has prevented human rabies cases from falling. Equally, there were other interventions in Peru to control rabies prior to 1983, possibly lowering the number of rabies cases prior to 1983 and obscuring the national programme’s effect. These interventions included the culling of stray dogs until 1988 and a vaccination programme of dogs in Lima between 1970–1973.15 Peru is one of only 8 Latin America and Caribbean (LAC) countries where canine-transmitted rabies has resulted in human deaths since 2009.2 It is possible that the decreased administration of RIG compared to the WHO recommendations has a role in this.
Human rabies has fallen considerably in LAC
Since 1970, documented cases of human rabies in LAC have fallen by over 90%16,17 (Figure 4). This suggests that the international commitment to control rabies has had a great effect. Despite this, canine-transmitted rabies has yet to be successfully eliminated from LAC.3 Reasons for this may include the different anti-rabies campaigns and their successes in the individual countries of the continent. Haiti, for example, has a higher incidence of dog transmitted rabies. Haiti also has less mass canine vaccination, insufficient reporting and decreased amounts of post-exposure prophylaxis.3 Equally, dogs may now be serving more as a vector than a reservoir – with other mammals (such as the haematogenous bats) infecting them before they in turn infect humans, and thus preventing the elimination of canine-transmitted rabies in LAC.
Cases of canine rabies have decreased considerably in both Peru and LAC
Cases of canine rabies have fallen drastically in both Peru and LAC on the whole. In Peru, this decrease has occurred since 1983, when the PAHO first pledged to eliminate canine-transmitted rabies (Table 1), after which mass canine vaccination was introduced. These data suggest that mass vaccination of the domestic dog population is key to eliminating canine rabies, possibly due in part to effects on herd immunity.
Table 1. Canine rabies cases across Peru and LAC have strongly decreased since 1970, with the largest fold reduction since 1983. Data: SIRVERA (Panaftosa–PAHO/WHO)16.
| 1970 | 1983 | 2012 | % change 1970–2012 | % change 1970–1983 | % change 1983–2012 | |
| Peru | 1048 | 2566 | 14 | 98.7% ↓ | 144.8% ↑ | 99.5% ↓ |
| LAC | 21413 | 11205 | 293 | 98.6% ↓ | 47.7% ↓ | 97.4% ↓ |
Many Factors are Needed to Allow Implementation of a Programme to Control and Manage Rabies
The programme detailed above represents the end of a long process and a multitude of different factors. Firstly, international cooperation and commitment was needed to recognise rabies as a major public health hazard and to pledge to eradicate it.3,4 In addition WHO/PAHO support was necessary17 to set up organisations, such as SIRVERA16 to monitor and report on the number of rabies cases and discuss nations’ progress.3,16 Money and investment were required to purchase the vaccines. These vaccinations then needed to be obtained and supplied around the separate countries, requiring adequate infrastructure, including roads such as the Pan American Highway.3 Additionally, many personnel had to be trained and provided with the appropriate equipment.2 Currently the chief disease burden of rabies is in Africa and Asia.5 It is likely that similar arrangements will be needed in order to introduce programmes to control rabies in these parts of the world.
Conclusion
The example of Trujillo has leant evidence to the view that national public health measures to control rabies by mass canine vaccination of the domestic dog population can help to limit the incidence of rabies at a local level in both humans and animals, especially in areas like Trujillo where dogs are the most significant reservoir. Equally, it suggests that appropriate management of a human victim as detailed in national guidelines can be effective at saving lives at a grassroots level. It is hoped, that with a similar set-up to that described above, programmes for controlling rabies may be implemented in other parts of the world, where the current disease burden of rabies is greater.
List of Abbreviations
- BHK
Baby hamster kidney
- CC
Cell culture
- ERIG
Equine rabies immunoglobulin
- GDP
Gross domestic produce
- HRDT
Hospital Regional Docente de Trujillo
- HRIG
Human rabies immunoglobulin
- LAC
Latin America and the Caribbean
- LRB
Lactating Rat Brain
- PAHO
Pan American Health Organisation
- RIG
Rabies Immunoglobulin
- SIRVERA
Sistema de Informação Regional para a Vigilância Epidemiológica da Raiva (Regional information system for epidemiological surveillance of rabies)
- WHO
World Health Organisation
Acknowledgments
We would like to thank Tamara Hornik, Gabriel Adams, Marianne Comparet, the International Society for Neglected Tropical Diseases and Selwyn College, Cambridge for their support.
References
- 1. Instituto Nacional de Estadística e Informática Evolución de la Población Censada Urbana, Según departamento y Año Censal (2012). Available from http://www.inei.gob.pe/estadisticas/indice-tematico/poblacion-y-vivienda/ [Google Scholar]
- 2. Ministerio de Salud [del Perú], Norma Técnia de Salud para la Prevención y Control de la Rabia en el Perú (2008). Available from http://www.minsa.gob.pe/portada/est_san/archivo/2011/NTS_DE_RABIA.pdf. [Google Scholar]
- 3.Vigilato MA, Clavijo A, Knobl T, Silva HM, Cosivi O, Schneider MC, Leanes LF, Belotto AJ, Espinal MA. Progress towards eliminating canine rabies: policies and perspectives from Latin America and the Caribbean. Philos Trans R Soc Lond B Biol Sci. 2013 Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Organización Panamericana de La Salud. 1983 Estrategia y Plan de acción para la eliminación de la rabia humana en América Latina para el final de la de cada 1980. Guayaquil, Ecuador: Organización Panamericana de la Salud. [Google Scholar]
- 5. WHO Rabies information available at http://www.who.int/rabies/en/ [Google Scholar]
- 6.Hatz CF, Kuenzli E, Funk M. Rabies: relevance, prevention, and management in travel medicine. Infect Dis Clin North Am. 2012 Sep;26(3):739–53. doi: 10.1016/j.idc.2012.05.001. doi: 10.1016/j.idc.2012.05.001. Epub 2012 Jul 5. [DOI] [PubMed] [Google Scholar]
- 7.Hemachudha T, Ugolini G, Wacharapluesadee S, Sungkarat W, Shuangshoti S, Laothamatas J. Human rabies: neuropathogenesis, diagnosis, and management. Lancet Neurol. 2013 May;12(5):498–513. doi: 10.1016/S1474-4422(13)70038-3. doi: 10.1016/S1474-4422(13)70038-3. [DOI] [PubMed] [Google Scholar]
- 8.Leung AK, Davies HD, Hon KL. Rabies: epidemiology, pathogenesis, and prophylaxis. Adv Ther. 2007 Nov-Dec;24(6):1340–7. doi: 10.1007/BF02877781. 24;368(1623):20120143. doi: 10.1098/rstb.2012.0143. Print 2013 Aug 5. [DOI] [PubMed] [Google Scholar]
- 9.Rupprecht CE, Barrett J, Briggs D, Cliquet F, Fooks AR, Lumlertdacha B, Meslin FX, Müler T, Nel LH, Schneider C, Tordo N, Wandeler AI. Can rabies be eradicated? Dev Biol (Basel). 2008;131:95–121. [PubMed] [Google Scholar]
- 10.Jemberu WT, Molla W, Almaw G, Alemu S. Incidence of rabies in humans and domestic animals and people's awareness in North Gondar Zone, Ethiopia. PLoS Negl Trop Dis. 2013 May 9;7(5):e2216. doi: 10.1371/journal.pntd.0002216. doi: 10.1371/journal.pntd.0002216. Print 2013 May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan M, Palmer J. Dog bites.BMJ. 2007 Feb 24;334(7590):413–7. doi: 10.1136/bmj.39105.659919.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. WHO Administration of rabies immunoglobulin (2013) available at http://www.who.int/rabies/human/adminimmuno/en/ [Google Scholar]
- 13. WHO Expert Consultation on Rabies (2013). Available at http://apps.who.int/iris/bitstream/10665/85346/1/9789241209823_eng.pdf. [Google Scholar]
- 14.Fekadu M, Shaddock JH, Baer GM.Excretion of Rabies Virus in the Saliva of Dogs. J Infect Dis(1982)1455715–719.doi: 10.1093/infdis/145.2.715 [DOI] [PubMed] [Google Scholar]
- 15.Chomel B, Chappius G, Bullon F, Cardenas E, David de Beublain T, Maufrais MC, Giambuno E. Serological results of a dog vaccination campaign against rabies in Peru Rev. sei. tech. Off. int. Epiz. 1987;6(I):97–113. doi: 10.20506/rst.6.1.284. [DOI] [PubMed] [Google Scholar]
- 16. Pan American Health Organization, Pan American Foot-and-Mouth Disease Center, Veterinary Public Health Unit. 2012 Sistema de Informação Regional para a Vigilância Epidemiológica da Raiva (Regional information system for epidemiological surveillance of rabies) SIRVERA (2013). Available at http://siepi.panaftosa.org.br.SIRVERA. [Google Scholar]
- 17.Belotto A, Leanes LF, Schneider MC, Tamayo H, Correa E. Overview of rabies in the Americas. Virus Res. 2005 Jul;111(1):5–12. doi: 10.1016/j.virusres.2005.03.006. [DOI] [PubMed] [Google Scholar]



