Abstract
Background:
Traditionally, conservative treatment of thoracolumbar (TL) burst fractures without neurologic deficit has encompassed the application of an extension brace. However, their effectiveness on maintaining the alignment, preventing posttraumatic deformities, and improving back pain, disability and quality of life is doubtful.
Objective:
The objective was to identify and summarize the evidence from randomized controlled trials (RCTs) to determine whether bracing patients who suffer TL fractures adds benefices to the conservative manage without bracing.
Materials and Methods:
Seven databases were searched for relevant RCTs that compared the clinical and radiological outcomes of orthosis versus no-orthosis for TL burst fractures managed conservatively. Primary outcomes were: (1) Loss of kyphotic angle; (2) failure of conservative management requiring subsequent surgery; and (3) disability and pain outcomes. Secondary outcomes were defined by health-related quality of life and in-hospital stay.
Results:
Based on predefined inclusion criteria, only two eligible high-quality RCTs with a total of 119 patients were included. No significant difference was identified between the two groups regarding loss of kyphotic angle, pain outcome, or in-hospital stay. The pooled data showed higher scores in physical and mental domains of the Short-Form Health Survey 36 in the group treated without orthosis.
Conclusion and Recommendation:
The current evidence suggests that orthosis could not be necessary when TL burst fractures without neurologic deficit are treated conservatively. However, due to limitations related with number and size of the included studies, more RCTs with high quality are desirable for making recommendations with more certainty.
Keywords: Burst fracture, instability, orthosis, posterior ligamentous complex, thoracolumbar spine
INTRODUCTION
Burst fractures account for up to 17% of all major spinal fractures, and the thoracolumbar (TL) region (T11 to L2) is the most common site of such injuries. Burst fractures results from axial compression failure of the vertebral end plates and the anterior and middle columns.[1,2,3]
The majority of burst fractures are associated with some canal compromise, as a result of retropulsion of osseous fragments from the posterior wall of the vertebral body. Those osseous fragments may put in risk of neurologic injury, which has been reported to occur in up to 30% of the patients with TL fractures.[1,4] However, most patients with burst fractures do not have neurologic deficits and can be managed conservatively, especially when the posterior ligamentous complex is intact.[2,3,5,6,7,8,9] Nonoperative treatment has been encouraged for TL burst fractures because several studies have showed that conservative treatment could lead to good radiological and clinical long-term outcomes avoiding surgical related complications.[9,10,11,12,13]
Traditionally, conservative treatment of burst fractures has encompassed the initial rest in bed with or without postural reduction, but almost always is followed by application of an extension brace, early mobilization, and rehabilitation.[14] Currently, several orthotic TL devices are available for treatment of TL burst fractures, including anterior hyperextension brace (ASH), Jewett brace, Taylor–Knight brace and total body contact or “thoracolumbar sacral orthosis (TLSO)” brace. However, their effect on maintaining the alignment and preventing posttraumatic deformities is doubtful.[1,15,16,17,18] In addition, there is not convincing evidence about their value on improving back pain, disability, and health-related quality of life.[19,20] Lastly, the use of an orthosis results in additional cost to conservative treatment.
Over the last two decades, several studies have assessed the effectiveness of bracing in patients with TL burst fractures, but their results have not been subject of a comprehensive analysis.[15,17,19]
The objective of this review was to identify and summarize the evidence from randomized controlled trials (RCTs) to determine whether bracing patients who suffer TL fractures adds benefices to the conservative manage without bracing.
MATERIALS AND METHODS
The protocol was registered in International Prospective Register of Systematic Reviews (PROSPERO) system, from the Center for Revisions and Dissemination of the National Institute for Health Research of the United Kingdom; (Identifier: PROSPERO 2013: CRD42013006683). Results are presented following the PRISMA statement.[21]
Literature search
The literature search was performed by two independent reviewers (GAC and CDB) on articles included in the following databases: PubMed, the National Institutes of Health/National Library of Medicine, Clinical Trials Registry, CENTRAL (The Cochrane Library), EMBASE, LILACS, and Google Scholar. The search as through November 14, 2013 and did not have restrictions or filters with regard to language or year of publication. Literature search was carried out using the following key words: “orthosis,” “orthotic,” “burst fracture,” “spine fracture,” “vertebral fracture,” “injury” and “complications.”
Titles and abstracts of articles identified in the search were reviewed to recognize any relevant articles. Then, the full texts of selected article were obtained. The selection criteria were assessed by two independent reviewers to determine their suitability and discrepancies were settled by consensus.
Selection criteria
There were selected studies meeting the following characteristics:
Prospective RCTs;
studies with patients older than 18-year-old;
studies allocating at least 10 subjects in each group;
including participants who had acute traumatic TL burst fractures (AO Type A3) between T10 and L4;
presenting during the first 2 weeks of injury;
participants were allocated to one of the following orthosis: ASH brace, Jewett brace, Taylor–Knight brace or total body contact or “TLSO” brace;
continuous orthotic treatment for at least 3 months, and
minimum follow-up of 6 months. Outcomes measures must include at least one of the primary outcomes (kyphosis, failure of conservative management, disability, or pain outcomes) through a validated outcome measure.
Studies were rejected if meet any of the following:
Quasi-randomized or observational design;
studies including pediatric population; or
inability for data extraction from the study population.
Data extraction
Two authors (GAC and CDB) independently reviewed the full manuscripts of eligible studies. Data were entered in data extraction forms. Extracted data included publication data; sample size; treatment arms; timing of follow-up measurements; and primary and secondary outcomes. Disagreement between these reviewers was resolved by consensus.
For the present analysis, primary outcomes were:
Loss of kyphotic angle; as measured according to Cobb's method;
failure of conservative management requiring subsequent surgery; and
disability and pain outcomes. Secondary outcomes were defined by health-related quality of life and in-hospital stay.
Methodological quality assessment
Two authors (GAC and CDB) independently evaluated the methodological quality of the included studies using the Jadad's scale (also known as Oxford's scale), which scores studies’ description of randomization (2 points), blinding (2 points) and attrition information (1 point).[22] For purposes of classification, and in line of previous protocols, studies with a score of 3 or more on the Jadad's scale were considered of high methodological quality.[23]
Risk of biases also assessed using the criteria according to Cochrane risk of a bias tool. Seven domains were assessed in each included studies:
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective reporting.
Other bias.
Reviewers’ judgments were categorized as “low risk” of bias, “high risk” of bias or “unclear risk” of bias.[24]
The quality of evidence was graded applying the GRADE approach, using the software package GRADEprofiler (version 3.6; McMaster University, Hamilton, ON, Canada).[25]
Data analysis
A pooled analysis was performed on studies that provided data on outcomes of patients who underwent conservative management of TL burst fractures; with or without orthosis, using the software package RevMan 5.0 (Cochrane Collaboration, Oxford, United Kingdom).
Pooled analysis of dichotomous variables was presented pooled risk ratio estimates and the weighted mean differences (WMD) were used for continuous outcomes, along with 95% confidence intervals (95% CI).
Assessment of statistical heterogeneity was done by standard χ2 test and an I2 statistic. The I2 value describes the proportion of total variation in a study estimated to be due to heterogeneity among trials rather than sampling error.[26] For estimation of effect size, the random-effects model was employed to pool studies when statistical heterogeneity occurred (the P < 0.1) and/or when the I2 value was larger than 50%; otherwise, the fixed-effects model of Mantel-Haenszel method was used.
RESULTS
Search results
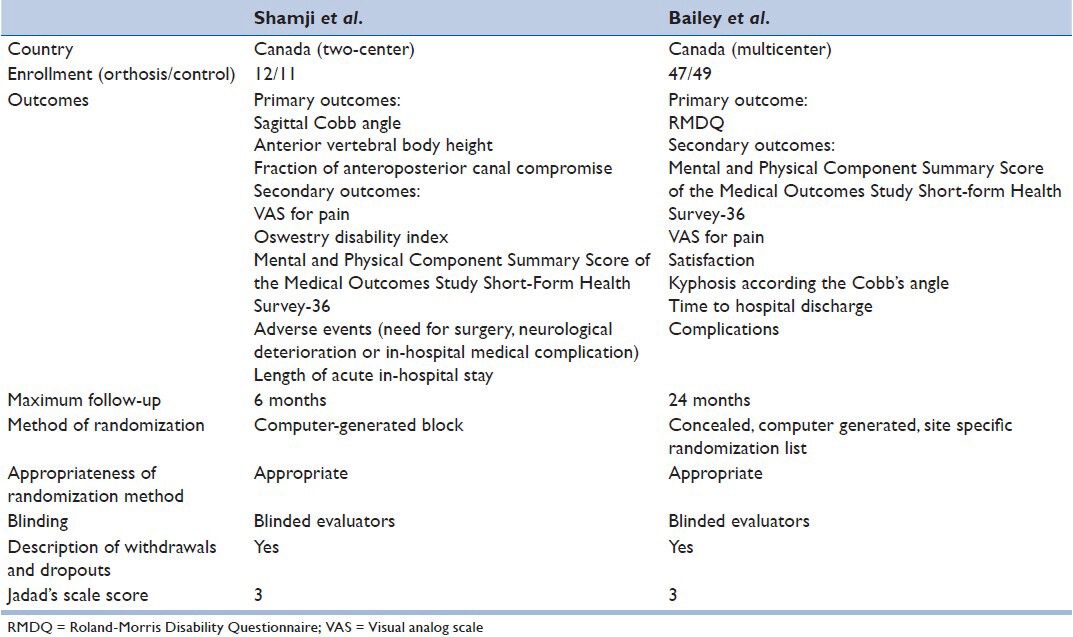
The search strategy [Figure 1] identified 316 potential studies from the databases. A total of 313 articles were excluded according to our selection criteria. The study by Bailey et al. published in 2009 was an interim analysis of a multicenter randomized clinical equivalence trial. Thus, it was excluded because it harbored preliminary data that were subsequently available as a final report.[19] Finally, two RCTs were selected and analyzed.[27,28] As conjunction, both studies recompiled data from a total of 129 patients and reported outcomes for 119 participants at follow-up of 6 months or more [Table 1].[27,28] Detailed sample size calculation was conducted to ensure appropriate power for the primary clinical endpoints for only one trial;[27] while the other was likely to be underpowered.[28]
Figure 1.
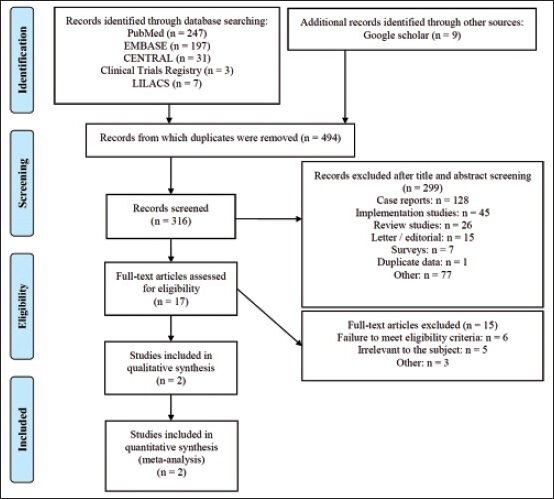
Flow-chart of the search strategy in the present systematic review
Table 1.
Characteristics and outcome parameters of the included randomized controlled clinical trials
Studies description
Bailey et al. conducted a multicenter, randomized, nonblinded equivalence trial involving three Canadian tertiary spine centers. They only enrolled patients with the following characteristics:
Harboring AO Type A3 burst fractures between T11 and L3,
Skeletally mature and <60 years of age,
Time to presentation up to 72 h from their injury,
Kyphotic deformity <35°, and without neurological deficits.[27]
The study compared patient's outcome after burst fracture treated with or without a TLSO orthesis (Aspen Medical Products, Irvine, CA, USA).
A total of 47 patients were enrolled into the TLSO group and 49 patients into the no orthosis group. The Roland-Morris Disability Questionnaire (RMDQ) score at 2 years postinjury was 8.7 ± 0.7 for the TLSO group and 9.8 ± 0.6 in the no orthosis group. The 95% CI (−0.8–2.9) was within the predetermined margin of equivalence. No statistically significant difference was found between treatment groups for all other secondary outcomes (visual analog scale [VAS] for pain, Short-Form 36 [SF-36] scores, kyphosis or satisfaction).
Shamji et al. performed a prospective, two-center, observer-blinded, RCT at Canadian tertiary care Level 1 trauma centers.[28] The aim of this study was to explore the relationship between bracing versus no-bracing in the treatment of TL burst fractures. They included neurologically intact patients with burst fractures (AO Type A3) from T10 to L4 for randomization, if their injury was judged to be appropriate for nonoperative care by a fellowship-trained spine surgeon. They used a custom-fitted TLSO in the treatment group.
A total of 23 patients were randomized for the study (TLSO: n = 12; no-brace: n = 11), and all them were available for assessing outcomes. After a 6-month follow-up, there were no statistically significant differences regarding radiological or self-reported clinical outcomes. There were no recorded failures of conservative treatment requiring subsequent surgery.
Results of methodological quality assessment of included studies
Two studies were assessed with Jadad's scale, and both were judged as high-quality according to the preestablished criteria.[27,28] Both studies were described as randomized and the methods for randomization were deemed appropriate. There was also an adequate description of withdrawals and dropouts in each study [Table 2]. However, performance bias relating to lack of blinding was inevitable in these two trials.
Table 2.
Quality assessment of the randomized controlled clinical trials included by using the Jadad's scale
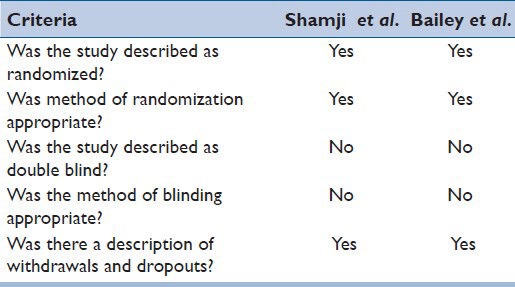
A further assessment of methodological quality using the Cochrane Risk of Bias tool revealed an overall low-risk of biases among both studies. However, these were judged at high-risk of performance biases, resulting from lack of blinding of patients [Table 3].
Table 3.
Risk of bias assessment of all included studies using the criteria according to Cochrane risk of biases tool
Primary outcomes
Two trials consisting of 119 participants report on loss of kyphotic angle as measured according Cobb's method.[27,28] Both studies were judged were rated as high quality according Jadad's scale. Pooled analysis shows that there is a not difference between groups regarding the amount of loss of kyphotic angle at the end of follow-up: WMD was 0.27 (95% CI, −2.38–2.93; P = 0.84) [Figure 2]. The heterogeneity index I2 was 0% and the quality of evidence for this outcome was moderate.
Figure 2.
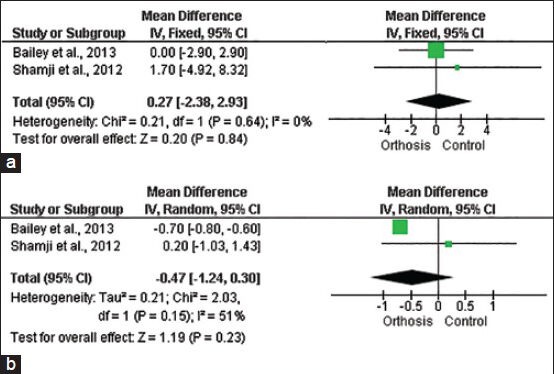
Forest plots evaluating primary outcomes. (a) Loss of kyphotic angle. (b) Visual analogue scale score
Failure of conservative management requiring subsequent surgery was reported by both two included trials. In the study by Bailey et al., there were recorded a total of six cases requiring surgery due to severe mechanical low back pain (three cases) or radicular pain (two cases), which were noted just after the initial bed rest phase before hospital discharge. Only one case in the TLSO group required late surgery.[27] On the other hand, in the study by Shamji et al., there were not recorded any case of failure of conservative treatment demanding surgery at the end of follow-up.[28] Since available data of this outcome were only from a single study, pooled risk ratio cannot be estimated.
Both included trials assessed disability according to a well-validated scale. In the study carried out by Shamji et al., there was found equivalent Oswestry Disability Index scores at 6 months postinjury between groups (TLSO group: 19 ± 6 vs. controls: 16 ± 7; P = 0.68).[28] In the other trial, there was also no difference in RMDQ scores at 2 years follow-up (TLSO group: 8.7 ± 0.7 vs. controls: 9.8 ± 0.6; P = 0.68).[27] However, due to the different scales of reporting disability, data on this parameter were not pooled.[27,28]
Pain outcomes were reported by two trials using the VAS pain score.[27,28] No further scale was employed in those trials for assessing pain outcomes. Pooled analysis shows that there is no difference between groups regarding the VAS score at the end of follow-up: WMD was-0.47 (95% CI, −1.24–0.30; P = 0.23) [Figure 2]. However, there was a marginal, but statistically significant inconsistence between results of individual studies (I2 = 51%). The quality of evidence for this outcome was very low.
Secondary outcomes
Health-related quality of life was reported in both included studies using the SF-36 survey.[27,28] Pooled analysis showed that Physical Component Summary Scores were higher in groups treated without orthosis. The WMD for this score was 2.5 (95% CI, 2.06–2.94; P < 0.001). Statistical heterogeneity was not significant between studies (I2 = 0%) and the quality of evidence for this outcome was low. Mental Component Summary Scores were also higher in this group (WMD 1.39 [95% CI, 0.91–1.87; P < 0.001]) [Figure 3]. Statistical heterogeneity was also nonsignificant (I2 was 2%). The quality of evidence for this outcome was moderate.
Figure 3.
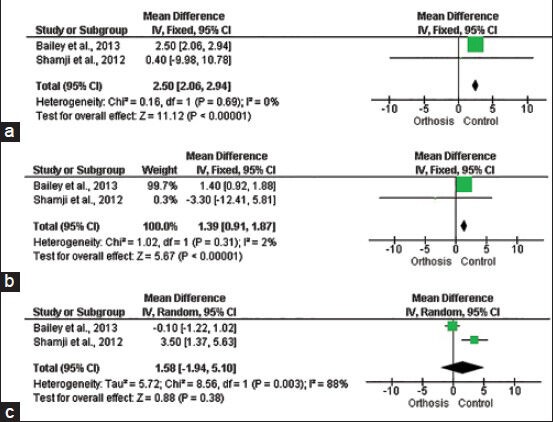
Forest plots evaluating secondary outcomes. (a) Physical Component Summary Score of the Medical Outcomes Study Short- Form Health Survey-36. (b) Mental Component Summary Score of the Medical Outcomes Study Short-Form Health Survey-36. (C) In-hospital stay
There was no significant difference in in-hospital stay among treatment groups (WMD 1.58 [95% CI, −1.94-5.10; [P = 0.38]) [Figure 3]. However, in-hospital stay demonstrated statistical significant heterogeneity between trials (I2 = 88%).
There were no possible to screen for potential biases because the small number of studies.
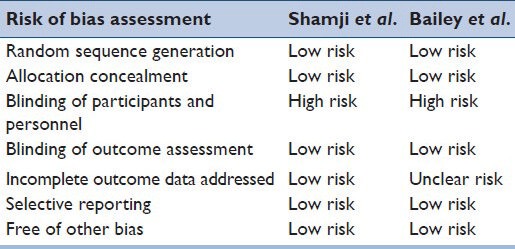
Quality of evidence
The complete GRADE evidence profile is presented in Figure 4.
Figure 4.
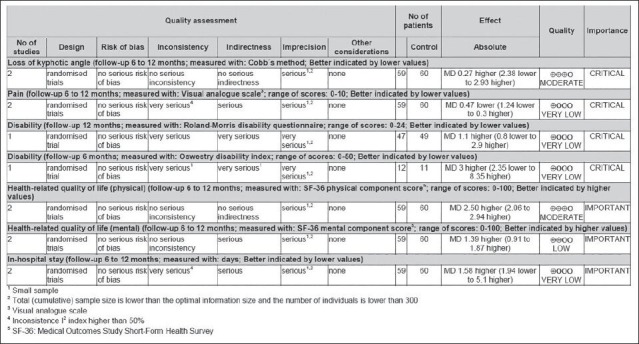
GRADE evidence profile for orthosis for thoracolumbar burst fractures without neurologic deficit (using GRADEprofiler version 3.6 [McMaster University, Hamilton, ON, Canada])
DISCUSSION
Several authors have deemed hyperextension orthosis as an integral part of nonoperative treatment of TL burst fractures;[29,30] however, there is also contradicting positions about their usefulness.[17,31] In 2009, Giele et al. had carried out a systematic review, including seven retrospective studies that had assessed the effect of bracing, but pooling data synthesis was not possible because of poor methodological quality, and therefore, the lack of high-quality studies prevents relevant conclusions from being drawn.[15] The aim of the present review was to clarify this uncertainty by assessing the highest quality available evidence provided by RCTs. In contrast with the review by Giele et al.,[15] both included RCTs were judged as high methodological quality according Jadad's scale and therefore, estimation of pooled results are deemed potentially translatable to the clinical setting.
Pooled WMD of primary outcomes showed no advantages of orthosis on the magnitude of loss of kyphotic angle according Cobb's method. This finding is in line of a previous study by Shen and Shen in which there were not found significant differences between the loss of reduction observed in patients who wear a hyperextension, Jewett braces and those treated without bracing.[17] Karjalainen et al. also found that the use of extension brace could not prevent the development of kyphotic deformity, despite seemed to decrease subjective symptoms during the early mobilization phase.[32]
The effects of wearing commonly prescribed extension orthosis on restriction of gross body motions has been investigated by several laboratories and clinical studies.[33,34] Lantz and Schultz examined four trunk movements (flexion, extension, lateral bending, and twisting) in five healthy adult men when standing and sitting, showing that TLSO failed to provide restrictions of at least 10% in at least one motion.[35] In another study, an extension brace and both an “off-the-shelf” and custom-molded TLSO were applied to cadaveric models of TL burst fracture, and the effect on fracture site motion were assessed. They found that no brace was able to restrict all range of motions and only TLSO orthosis can decrease angular motion, but had not effect translation at the fracture. In their study, they confirmed that extension orthosis had no effect on motion at the spinal fracture site.[36] Those biomechanical studies explain how orthosis failed to provide an adequate immobilization at fracture site, and therefore, are not capable to prevent the loss of kyphotic angle.
Pain outcomes were available as measured by VAS and the pooled analysis did not show statistically significant difference between treatment groups. However, there was significant heterogeneity in the analysis of this outcome, making conclusions quite doubtful.
As a measure of success of the conservative management, we planned to examine the risk of conservative treatment failure requiring subsequent surgery. However, there were recorded only few events, impeding to obtain conclusions with reasonable certainty. In the study by Shamji et al., there were no adverse events in regard to patients requiring surgery;[28] while in the study by Bailey only a total of six patients required surgical treatment; four who had been allocated in the TLSO group.[27] A detailed analysis of those treatment failures shows that five patients required surgery prior to their initial hospital discharge due to severe mechanical back pain impeding ambulation (three cases) or severe radicular pain with initial mobilization which was not present when supine. Only one patient treated in the TLSO group required an osteotomy 8 months following her fracture.[27] Therefore, on the basis those few cases, it is not possible to determine if there is any difference between treatment with or without an orthotic device in avoiding the need for late operative treatment.
Analysis of health-related quality of life was attained with SF-36 health survey, which is a valid tool for applying to spine trauma patients.[5] Pooled final scores showed that physical as well as mental domains were slightly better in those treated without orthosis. However, those differences were lower than the minimum clinically important difference.[37] This finding was unexpected, because a brace gave the patient spinal support, reduction of discomfort, and confidence to encourage exercise during the day.[38] However, a possible explanation for this finding is that orthosis may induce the psychological effect the appearance being sick or disabled for several activities, while its removal may facilitate sleep and a feeling of general well-being.[38]
Despite the hospital stay is commonly used as a measure of resource consumption of health interventions, it was examined as a secondary outcome, because it may be related with the celerity of the care center for customizing, designing and applying external orthosis previously to hospital discharge. Therefore, it may not be strictly reflects the severity of pain or hospital care required by patients. However, the pooled analysis showed very heterogeneous results, without statistically significant differences between treatment groups.
Regardless of the exclusive selection of high-quality RCTs, which allows minimizing the risk of bias, the present review had several limitations that must be recognized. Firstly, conclusions may not be as generalizable to the entire population because is based on efficacy studies; hence, follow-up is made under strictly controlled conditions. Therefore, observational studies detailing outcomes of patients are necessary to estimate the effects in large and heterogeneous populations.
In addition, current literature could be distorted by selection bias because there was no description regarding integrity of the posterior ligamentous complex, which integrity is of paramount importance for determining the suitability for conservative treatment.[2,39,40,41,42]
Another major drawback was the lack of available data for analyzing disability, which is one of the most important primary outcomes when assessing interventions for treating TL spine disorders. However, results of individual studies using different scales (RMDQ and Oswestry Disability Index) showed absence of statistically significant differences among treatment groups.[19,27,28] Finally, the relatively small number of patients in the present review could mask a possible small beneficial effect of TL braces.
CONCLUSION
Currently, available literature has described no difference regarding loss of kyphotic angle, pain outcome and hospital stays between patients treated with or without orthosis. Furthermore, those devices may be associated with impairment of the health-related quality of life. Therefore, the results of this review suggest that orthosis may be unnecessary when TL burst fractures without neurologic deficit are treated conservatively.
Avoiding the use of orthosis could yield similar clinical and radiological outcomes, while save costs and patient physical deconditioning associated with a brace. However, due to limitations related with number and size of the included studies, more RCTs with high quality are desirable for making recommendations with more certainty.
Footnotes
Source of Support: Health Sciences and Neurosciences (CISNEURO) Research Group, Cartagena de Indias, Colombia.
Conflict of Interest: None declared.
REFERENCES
- 1.Rajasekaran S. Thoracolumbar burst fractures without neurological deficit: The role for conservative treatment. Eur Spine J. 2010;19(Suppl 1):S40–7. doi: 10.1007/s00586-009-1122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joaquim AF, Patel AA. Thoracolumbar spine trauma: Evaluation and surgical decision-making. J Craniovertebr Junction Spine. 2013;4:3–9. doi: 10.4103/0974-8237.121616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heary RF, Kumar S. Decision-making in burst fractures of the thoracolumbar and lumbar spine. Indian J Orthop. 2007;41:268–76. doi: 10.4103/0019-5413.36986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hitchon PW, He W, Viljoen S, Dahdaleh NS, Kumar R, Noeller J, et al. Predictors of outcome in the non-operative management of thoracolumbar and lumbar burst fractures. Br J Neurosurg. 2013 doi: 10.3109/02688697.2013.872226. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A:773–81. doi: 10.2106/00004623-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Vaccaro AR, Zeiller SC, Hulbert RJ, Anderson PA, Harris M, Hedlund R, et al. The thoracolumbar injury severity score: A proposed treatment algorithm. J Spinal Disord Tech. 2005;18:209–15. [PubMed] [Google Scholar]
- 7.Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: A systematic review. J Neurosurg Spine. 2006;4:351–8. doi: 10.3171/spi.2006.4.5.351. [DOI] [PubMed] [Google Scholar]
- 8.Moller A, Hasserius R, Redlund-Johnell I, Ohlin A, Karlsson MK. Nonoperatively treated burst fractures of the thoracic and lumbar spine in adults: A 23- to 41-year follow-up. Spine J. 2007;7:701–7. doi: 10.1016/j.spinee.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Gnanenthiran SR, Adie S, Harris IA. Nonoperative versus operative treatment for thoracolumbar burst fractures without neurologic deficit: A meta-analysis. Clin Orthop Relat Res. 2012;470:567–77. doi: 10.1007/s11999-011-2157-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abudou M, Chen X, Kong X, Wu T. Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev. 2013;6:CD005079. doi: 10.1002/14651858.CD005079.pub3. [DOI] [PubMed] [Google Scholar]
- 11.Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine (Phila Pa 1976) 2003;28:2459–65. doi: 10.1097/01.BRS.0000090834.36061.DD. [DOI] [PubMed] [Google Scholar]
- 12.Tian NF, Wu YS, Zhang XL, Wu XL, Chi YL, Mao FM. Fusion versus nonfusion for surgically treated thoracolumbar burst fractures: A meta-analysis. PLoS One. 2013;8:e63995. doi: 10.1371/journal.pone.0063995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heary RF, Salas S, Bono CM, Kumar S. Complication avoidance: Thoracolumbar and lumbar burst fractures. Neurosurg Clin N Am. 2006;17:377–88. doi: 10.1016/j.nec.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Wood KB, Li W, Lebl DS, Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014;14:145–64. doi: 10.1016/j.spinee.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 15.Giele BM, Wiertsema SH, Beelen A, van der Schaaf M, Lucas C, Been HD, et al. No evidence for the effectiveness of bracing in patients with thoracolumbar fractures. Acta Orthop. 2009;80:226–32. doi: 10.3109/17453670902875245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ohana N, Sheinis D, Rath E, Sasson A, Atar D. Is there a need for lumbar orthosis in mild compression fractures of the thoracolumbar spine?: A retrospective study comparing the radiographic results between early ambulation with and without lumbar orthosis. J Spinal Disord. 2000;13:305–8. doi: 10.1097/00002517-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Shen WJ, Shen YS. Nonsurgical treatment of three-column thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976) 1999;24:412–5. doi: 10.1097/00007632-199902150-00024. [DOI] [PubMed] [Google Scholar]
- 18.van Middendorp JJ, Patel AA, Schuetz M, Joaquim AF. The precision, accuracy and validity of detecting posterior ligamentous complex injuries of the thoracic and lumbar spine: A critical appraisal of the literature. Eur Spine J. 2013;22:461–74. doi: 10.1007/s00586-012-2602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bailey CS, Dvorak MF, Thomas KC, Boyd MC, Paquett S, Kwon BK, et al. Comparison of thoracolumbosacral orthosis and no orthosis for the treatment of thoracolumbar burst fractures: Interim analysis of a multicenter randomized clinical equivalence trial. J Neurosurg Spine. 2009;11:295–303. doi: 10.3171/2009.3.SPINE08312. [DOI] [PubMed] [Google Scholar]
- 20.Agabegi SS, Asghar FA, Herkowitz HN. Spinal orthoses. J Am Acad Orthop Surg. 2010;18:657–67. doi: 10.5435/00124635-201011000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 23.Wang X, Li YM, Li WQ, Huang CG, Lu YC, Hou LJ. Effect of clazosentan in patients with aneurysmal subarachnoid hemorrhage: A meta-analysis of randomized controlled trials. PLoS One. 2012;7:e47778. doi: 10.1371/journal.pone.0047778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64:380–2. doi: 10.1016/j.jclinepi.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 26.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11:193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 27.Bailey CS, Urquhart JC, Dvorak MF, Nadeau M, Boyd MC, Thomas KC, et al. Orthosis versus no orthosis for the treatment of thoracolumbar burst fractures without neurologic injury: A multicenter prospective randomized equivalence trial. Spine J. 2013 doi: 10.1016/j.spinee.2013.10.017. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Shamji MF, Roffey DM, Young DK, Reindl R, Wai EK. A pilot evaluation of the role of bracing in stable thoracolumbar burst fractures without neurologic deficit. J Spinal Disord Tech. 2012 doi: 10.1097/BSD.0b013e31826eacae. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Öztürk I, Ertürer E, Sönmez MM, Sarı S, Şeker A, Seçkin MF. Early mobilization with customized TLSO brace in thoracolumbar burst fractures. Acta Orthop Traumatol Turc. 2012;46:373–8. [PubMed] [Google Scholar]
- 30.Aligizakis A, Katonis P, Stergiopoulos K, Galanakis I, Karabekios S, Hadjipavlou A. Functional outcome of burst fractures of the thoracolumbar spine managed non-operatively, with early ambulation, evaluated using the load sharing classification. Acta Orthop Belg. 2002;68:279–87. [PubMed] [Google Scholar]
- 31.Patwardhan AG, Li SP, Gavin T, Lorenz M, Meade KP, Zindrick M. Orthotic stabilization of thoracolumbar injuries. A biomechanical analysis of the Jewett hyperextension orthosis. Spine (Phila Pa 1976) 1990;15:654–61. doi: 10.1097/00007632-199007000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Karjalainen M, Aho AJ, Katevuo K. Painful spine after stable fractures of the thoracic and lumbar spine. What benefit from the use of extension brace? Ann Chir Gynaecol. 1991;80:45–8. [PubMed] [Google Scholar]
- 33.Kienle A, Saidi S, Oberst M. Effect of 2 different thoracolumbar orthoses on the stability of the spine during various body movements. Spine (Phila Pa 1976) 2013;38:E1082–9. doi: 10.1097/BRS.0b013e3182983518. [DOI] [PubMed] [Google Scholar]
- 34.Wang XY, Dai LY, Xu HZ, Chi YL. Kyphosis recurrence after posterior short-segment fixation in thoracolumbar burst fractures. J Neurosurg Spine. 2008;8:246–54. doi: 10.3171/SPI/2008/8/3/246. [DOI] [PubMed] [Google Scholar]
- 35.Lantz SA, Schultz AB. Lumbar spine orthosis wearing. I. Restriction of gross body motions. Spine (Phila Pa 1976) 1986;11:834–7. doi: 10.1097/00007632-198610000-00019. [DOI] [PubMed] [Google Scholar]
- 36.Rubery PT, Brown R, Prasarn M, Small J, Conrad B, Horodyski M, et al. Stabilization of 2-column thoracolumbar fractures with orthoses: A cadaver model. Spine (Phila Pa 1976) 2013;38:E270–5. doi: 10.1097/BRS.0b013e3182804c73. [DOI] [PubMed] [Google Scholar]
- 37.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: A choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J. 2008;8:968–74. doi: 10.1016/j.spinee.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 38.Stadhouder A, Buskens E, Vergroesen DA, Fidler MW, de Nies F, Oner FC. Nonoperative treatment of thoracic and lumbar spine fractures: A prospective randomized study of different treatment options. J Orthop Trauma. 2009;23:588–94. doi: 10.1097/BOT.0b013e3181a18728. [DOI] [PubMed] [Google Scholar]
- 39.Gabriel AC, Angel JP, Juan JG, Luis RM, Hernando RA, Rubén SB. Diagnostic accuracy of ultrasound for detecting posterior ligamentous complex injuries of the thoracic and lumbar spine: A systematic review and meta-analysis. J Craniovertebr Junction Spine. 2013;4:25–31. doi: 10.4103/0974-8237.121621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Joaquim AF, Fernandes YB, Cavalcante RA, Fragoso RM, Honorato DC, Patel AA. Evaluation of the thoracolumbar injury classification system in thoracic and lumbar spinal trauma. Spine (Phila Pa 1976) 2011;36:33–6. doi: 10.1097/BRS.0b013e3181c95047. [DOI] [PubMed] [Google Scholar]
- 41.Vaccaro AR, Rihn JA, Saravanja D, Anderson DG, Hilibrand AS, Albert TJ, et al. Injury of the posterior ligamentous complex of the thoracolumbar spine: A prospective evaluation of the diagnostic accuracy of magnetic resonance imaging. Spine (Phila Pa 1976) 2009;34:E841–7. doi: 10.1097/BRS.0b013e3181bd11be. [DOI] [PubMed] [Google Scholar]
- 42.Lee JY, Vaccaro AR, Schweitzer KM, Jr, Lim MR, Baron EM, Rampersaud R, et al. Assessment of injury to the thoracolumbar posterior ligamentous complex in the setting of normal-appearing plain radiography. Spine J. 2007;7:422–7. doi: 10.1016/j.spinee.2006.07.014. [DOI] [PubMed] [Google Scholar]


