Abstract
AIM: To compare endoscopic sclerotherapy (ES) with distal splenorenal shunt (DSRS) in the prevention of recurrent variceal bleeding in cirrhotic patients during a long-term follow-up period.
METHODS: In 1984 we started a prospective, controlled study of patients with liver cirrhosis. Long-term follow-up presents a natural history of liver cirrhosis complicated by advanced portal hypertension. In this study the effects of 2 types of treatment, DSRS or ES, were evaluated. The study population included 80 patients with cirrhosis and portal hypertension referred to our department from October 1984 to March 1991. These patients were drawn from a pool of 282 patients who underwent either elective surgery or ES during the same period of time. Patients were assigned to one of the 2 groups according to a random number table: 40 to DSRS and 40 to ES using polidocanol.
RESULTS: During the postoperative period, no DSRS patient died, while one ES patient died of uncontrolled hemorrhage. One DSRS patient had mild recurrent variceal hemorrhage despite an angiographically patent DSRS and another patient suffered duodenal ulcer rebleeding. Eight ES patients suffered at least one episode of gastrointestinal bleeding: 4 from varices and 4 from esophageal ulcerations. Eight ES patients developed transitory dysphagia. Long-term follow-up was completed in all patients except for 5 cases (2 DSRS and 3 ES patients). Five-year survival rates for shunt (73%) and ES (56%) groups were statistically different: in this follow-up period and in subsequent follow-ups this difference decreased and ceased to be of statistical relevance. The primary cause of death became hepatocellular carcinoma (HCC). Four DSRS patients rebled due to duodenal ulcer, while eleven ES patients had recurrent bleeding from esophago-gastric sources (seven from varices, three from hypertensive gastropathy, one from esophageal ulcerations) and two from unknown sources. Nine DSRS and 2 ES patients developed a chronic encephalopathy; 13 DSRS and 5 ES patients suffered at least one episode of acute encephalopathy. Five ES patients had esophageal stenoses, which were successfully dilated.
CONCLUSION: In a subgroup of patients with good liver function, DSRS with a correct portal-azygos disconnection more effectively prevents variceal rebleeding than ES. However, this positive effect did not influence the long-term survival because other factors (e.g. HCC) were more important in deciding the fate of the cirrhotic patients with portal hypertension.
Keywords: Esophageal varices, Portal hypertension, Liver cirrhosis, Shunt surgery, Endoscopic sclerotherapy
INTRODUCTION
The selective distal splenorenal shunt (DSRS) proposed by Warren[1] in 1967 has been considered to be the best procedure available for surgical decompression of patients with portal hypertension[2-4]. DSRS has been compared with sclerotherapy in four trials[5-8]. Meta-analysis of these studies[9] showed that DSRS significantly reduces the incidence of rebleeding and only slightly increases the occurrence of chronic encephalopathy, but does not improve survival. We began a prospective, randomized clinical trial to study the prevention of recurrent variceal bleeding in cirrhotic patients during long-term follow-up in 1984[8]. We continued recruitment until 1991 and continued to study the patients in the following years. In this interval of time, new procedures and new randomized trials were carried out, but as regards to survival, no treatment seems to be superior to another in patients with good or moderate liver function[10]. As regards to other surgical options, use of a small-diameter prosthetic H-graft portacaval shunt has been compared with the transjugular intra-hepatic porto-systemic shunt (TIPSS), showing a favorable trend in survival in the surgical group[11]. On the other hand, TIPSS has been compared with endoscopic sclerotherapy (ES) in 11 randomized trials and TIPSS seems, as confirmed by two meta-analyses[12,13], to reduce rebleeding, but significantly increases encephalopathy without differences in survival. Furthermore, a number of trials comparing endoscopic band ligation with ES have been performed in the past few years and a meta-analysis of these studies[14] showed that it is more effective than ES in preventing rebleeding, with no differences in survival.
Based on these analyses, it seems reasonable to choose as first-line therapy (i.e. beta-blockers, endoscopic band ligation, etc.) the least aggressive therapy[15]. TIPSS or shunt surgery can be performed as a salvage treatment in patients who continue to rebleed and maintain good liver function. The purpose of this report is to describe the follow-up of patients in this study, which now extends beyond 20 years for surviving patients. Long-term follow-up presents the natural history of a subgroup of patients with portal hypertension in whom an active treatment (DSRS or ES) reduced the risk of rebleeding without causing irreversible damage to liver function.
MATERIALS AND METHODS
Patients
The study population comprised 80 patients with cirrhosis and portal hypertension referred to our department from October 1984 to March 1991. These patients were drawn from a pool of 282 patients who underwent either elective surgery or endoscopic sclerotherapy because of portal hypertension during this period of time.
Criteria for inclusion in the study were as follows: (1) liver cirrhosis confirmed by biopsy in all patients; (2) endoscopic documentation of variceal hemorrhage (actively bleeding varix or non-bleeding varices without other lesions) requiring at least one unit of blood transfusion; (3) arrest of acute variceal hemorrhage either spontaneously or by use of intravenous vasopressin and/or somatostatin and/or balloon tamponade and/or haemostatic sessions of ES; (4) less than 70 years old;(5) good or moderate liver function (Child’s A and B class)[16]; (6) patency of the splanchnic venous system and hepatopetal portal flow (according to Nordlinger’s classification)[17]; (7) eligible for either shunt or ES; (8) absence of life-threatening diseases (e.g. tumors); (9) willing to return for regular follow-up. Patients bleeding from gastric varices were excluded. Figure 1 shows the reasons for the exclusion of 202 patients.
Figure 1.
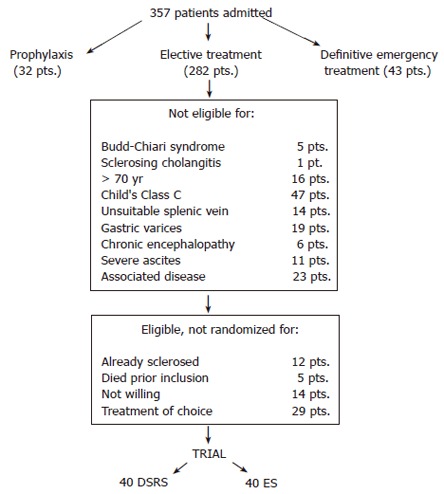
Reasons for exclusion. pts: patients.
Randomization for assignment into groups was carried out when the patient was stabilized, which occurred no more than 24 h before treatment. Patients were assigned to one of the 2 groups according to a random numbers table. Informed written consent was obtained from all patients prior to their inclusion in the study. No patient refused the assigned treatment.
Variceal rebleeding within 2 years of first treatment was considered as the primary measure of patient outcome. The sample size needed to show a decrease in variceal rebleeding from 43% to 7% is about 20 patients for each group, applying standard power (90%), type I error (P < 0.05) and a two-tailed t-test[18].
Preoperative evaluation
A complete medical history was obtained for each patient, and particular notice was taken of previous episodes of gastrointestinal bleeding and evidence of either primary or post hemorrhagic hepatic failure (jaundice, ascites or edema). Routine laboratory tests were performed to evaluate liver function (Table 1). Overall assessment of the severity of liver disease was graded according to the Child-Pugh classification system[16] and a personal hepatic score was obtained as previously described[4,19]. Serum alpha-fetoprotein assessment and ultrasonography were routinely performed in order to screen for the presence of hepatocellular carcinoma. The presence of esophageal varices was assessed through endoscopic examination. Criteria used for classifying the endoscopic findings were based on the General Rules for Recording Endoscopic Findings on Esophageal Varices compiled by the Japanese Research Society for Portal Hypertension[20].
Table 1.
Characteristics of patients enrolled in the RCT
| Characteristic | DSRS (n = 40) | ES (n = 40) | P |
| Age (yr) | 49.4 ± 9.9 | 53.8 ± 8.4 | 0.027 |
| Sex: M/F | 27/13 | 33/7 | 0.121 |
| Etiology: alcoholic/ non alcoholic | 14/26 | 26/14 | 0.0073 |
| Child’s class: A/B | 19/21 | 11/29 | 0.053 |
| Prothrombin time: > 80/80-50/< 50 | 5%/82%/13% | 13%/62%/25% | 0.058 |
| Bilirubin (μmol/L): < 20.5/20.5-51.3/> 51.3 | 62%/38%/0% | 41%/46%/13% | 0.0269 |
| Albumin (g/L): > 30/30-25/< 25 | 95%/5%/0% | 83%/17%/0% | 0.077 |
| Portal perfusion: degree I/II/III | 45%/45%/10% | 42%/27%/31% | 0.09 |
| Previous bleeding (n) | 2.3 ± 1.5 | 1.6 ± 0.09 | 0.022 |
| Blood unit (n) | 5.5 ± 5 | 4.3 ± 4.2 | 0.25 |
| Interval between bleeding and treatments (mo) | 3.5 ± 2.5 | 2.8 ± 3.2 | 0.32 |
| Previous encephalopathy episodes (n) | 10 | 7 | 0.41 |
| Easily controlled preoperative ascites | 5 | 11 | 0.09 |
Cerebral function was assessed through a complete neurological examination, taking into account mental state, asterixis, electroencephalographic findings (EEG), the trail making test[21] and the “Cancelling A’s” test[22]. Our grading of hepatic encephalopathy (HE) has been previously described[4,8,23]. We called HE “acute” if it was precipitated by gastrointestinal bleeding, heavy drinking, pharmacological or dietary imbalances, of brief duration and easily controlled with elimination of the precipitating cause. We called HE “chronic” if it was spontaneous, of long duration and more difficult to manage. Naturally, preoperative HE was excluded in all patients.
A visceral angiogram was obtained by selective catheterization of the celiac axis and superior mesenteric artery. The degree of hepatic perfusion was evaluated according to Nordlinger’s criteria[17]. The rate of contrast infusion (sodium and meglumine ioxaglate, Hexabrix 320- Byk Gulden, Milan, Italy) infusion was 6 mL/s × 10 s.
Operative management
All shunt procedures were performed by a single experienced surgical team[24]. DSRS was constructed according to the technique described by Warren[25] (20 cases). In 18 cases a spleno-pancreatic disconnection[26] was performed as a technical addition to DSRS, offering the optimum surgical therapy for each patient. In 2 patients a total shunt was performed for technical reasons; they were included in the statistical analysis on an intention-to-treat basis.
Endoscopic variceal sclerosis was conducted by 2 endoscopists with extensive experience in the field[27]. All patients were given 5-10 mg diazepam premedication. ES was performed using an Olympus GIF IT flexible endoscope or an electronic Welch Allyn videoendoscope. At each session 10 to 50 mL of polidocanol (5-10 g/L) (Athoxysclerol, Creusller) and 5 g/L methylene blue were injected using a flexible injection needle in the area 5-7 cm above the esophago-gastric junction. Methylene blue allowed visual confirmation of intravariceal and paravariceal injections.
Postoperative evaluation
In the evaluation of hospital mortality and early complications, we defined the first 30 d after the initial treatment as the postoperative period. In the ES group, the events that occurred during the interval between the first session and eradication were also recorded and evaluated.
In the postoperative period, esophageal endoscopy was performed on each patient. A visceral angiography was performed on the 10th average postoperative day only in patients having DSRS. Shunt patency was verified in the venous phase of angiograms in the DSRS group. In the ES group, the number of further sessions depended on the findings obtained at endoscopy performed one week after the first sclerosis session. As soon as the eradication was achieved, the patient was included in the follow-up program. The remaining ES patients underwent further sclerosis sessions if they were free of complications, such as mucosal ulcerations, symptomatic stricture, severe esophagitis, fever and pneumonia. In the presence of complications, an upper endoscopy was performed at intervals of seven to ten days and further ES sessions were considered only when complications were resolved.
During the follow-up period, DSRS patients were checked at 1, 3 and 6 mo after discharge and then at least twice yearly, on an outpatient basis. Follow-up endoscopy was scheduled 4-6 wk after the last session and then at 6-mo intervals, unless recurrent hemorrhage occurred.
At each visit, liver function was evaluated following a complete medical examination and laboratory tests. Assessment of the neurological status was performed using the above-mentioned criteria. An EEG was performed at least once a year. A return to drinking was ascertained based on patients’ statements, our own assessment and information from relatives. Continued drinking was defined as daily consumption in excess of 1 liter wine and/or spirits. All patients were on a 10-meq sodium and protein-balanced diet (1 g protein/kg body wt) and undergoing lactulose prophylactic treatment: the initial dose was 60 g/d in 3 separate doses and adjusted thereafter to induce at least 1 bowel movement per day.
Definitions
Eradication was defined as the absence of varices or the presence of F1 white varices.
Rebleeding was defined as hemorrhage due to esophago-gastric varices and/or congestive gastropathy, requiring at least 1 unit blood transfusion and was designated as being from varices if this was supported by endoscopic findings. The treatment of choice for variceal rebleeding was emergency sclerotherapy. Chronic rebleeding from congestive gastropathy was treated with beta-blocking therapy[28]. Rebleeding due to peptic ulcer was recorded separately. The risk of hospitalization for HE was defined by taking the number of late hospital admissions due to episodes of HE, and dividing it by the total number of patients evaluated in the follow-up period.
Data management and statistical analysis
Initial and subsequent data for the patients were collected on a dedicated spreadsheet (Excel, Microsoft Corp., Delaware, USA) for personal computer input (Macintosh G4, Apple Computer Inc.) and subsequent analysis (Statistica-Mac, Statsoft, Tulsa OK, USA). Survival and therapy failures were analyzed by the Kaplan-Meier method and were compared by Breslow and log-rank test[29]. Comparison between groups was made by Chi-square test for proportions and Student’s t-test for the means. In all patients, some preoperative variables were recorded and their influence upon survival in each treatment group was assessed by means of univariate analysis and Cox’s proportional hazards regression model[30]. The association of each parameter with survival was univariately estimated by comparing actuarial curves (Kaplan-Meier product-limit method and log-rank test) after categorization of the continuous variables in a multivariate setting[31]. Only those parameters showing a statistical value of P < 0.2 were included in the multivariate analysis. The results of the univariate analysis helped to substantially reduce the number of prognostic factors. For each parameter analyzed in the multivariate analysis, the regression coefficient (beta), the T-values (Hazard ratio) and the 95% confidence intervals (CI) are given.
RESULTS
In the ES group, varices were completely eradicated in 36 patients (90%): 1 patient died before eradication and 3 patients abandoned the sclerotherapy program. The number of injection sessions was 3.7 ± 1.4 occurring over 5.1 ± 3.4 mo and the mean amount of polydocanol required for eradication was 84.7 ± 38.7 mL.
During the postoperative period, no DSRS patient died, while 1 ES patient died of uncontrolled hemorrhage after the first sclerosis session. One DSRS patient had mild recurrent variceal hemorrhage controlled by conservative therapy, despite an angiographically patent shunt and another patient rebled due to duodenal ulcer. Eight ES patients suffered at least one episode of gastrointestinal bleeding. Four were from varices requiring emergency variceal sclerotherapy and 4 from esophageal ulcerations, which were managed conservatively. No patient had episodes of hepatic encephalopathy during the immediate postoperative period. Eight ES patients developed transitory dysphagia due to esophageal ulcerations. One ES patient suffered pleural effusion.
The mean follow-up in the DSRS group was 109 ±58 (median 99.5) mo; ranging from 3 to 240 mo and the mean follow-up in the ES group was 87 ± 61 (median 71) mo; ranging from 1 to 237 mo. Long-term follow-up was complete in all patients, except for 5 cases (2 DSRS and 3 ES patients). No DSRS patient had shunt thrombosis, while 3 ES patients changed treatment: in 1 case a liver transplantation was successfully performed for liver failure and in 2 other cases a porto-caval H-graft shunting was performed for recurrent digestive bleeding. In the ES group, varices reformed in 14 of 36 eradicated patients (39%) after 20.4 ± 16.4 mo. They were successfully reeradicated. No DSRS patient had variceal rebleeding (four DSRS patients had duodenal ulcer rebleeding), while 7 ES patients had recurrent hemorrhage from varices, 3 from hypertensive gastropathy, 1 from esophageal ulcerations and 2 from unknown sources. The global percentage of patients who rebled was 10% and 33%, respectively (P = 0.0194). Figure 2 shows the actuarial curves of patients at risk of rebleeding. This risk was significantly higher in the ES group than in the DSRS group (P = 0.00251), above all for the first four years of follow-up. In the subsequent intervals of time, the two curves showed similar behavior.
Figure 2.
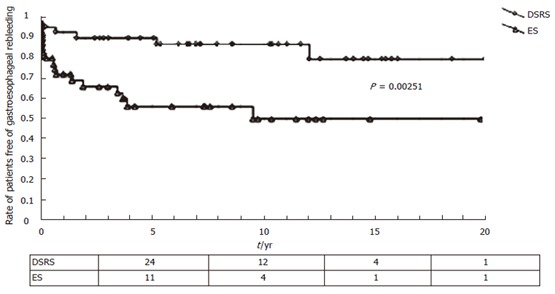
Actuarial curves of patients free from gastroesophageal rebleeding after distal spleno-renal shunt (DSRS) and endoscopic sclerotherapy (ES). P < 0.05 vs ES using the log-rank test.
There was no difference between patients with DSRS and ES in terms of preoperative results for the Trail making test, canceling A’s test and EEG (Table 2). Postoperatively, the Trail making test showed no modifications in either group, while the canceling A’s test showed an improved performance in both groups (probably due to a better comprehension of the test). EEG was unchanged after ES but worsened after DSRS. Thirteen DSRS (32.5%) and 5 ES patients (13%) suffered at least one episode of acute encephalopathy (P = 0.0189): three (2 DSRS and 1 ES) due to pharmacologic imbalance, three (2 DSRS and 1 ES) due to heavy drinking, three (1 DSRS and 2 ES) due to liver failure, seven (6 DSRS and 1 ES) due to constipation, one DSRS patient due to dietary abuse and one DSRS patient due to severe hyperglycemia. HE disappeared in all patients after medical therapy and dietary control in all patients. Nine DSRS (22.5%) and 2 ES patients (5%) developed a mild chronic encephalopathy: the difference in the incidence of chronic HE between DSRS and ES was statistically significant (P = 0.0263). However, the risk of hospitalization for HE was not different: 0.38 ± 0.4 and 0.28 ± 0.3 after DSRS and ES, respectively (P = NS). In summary, HE was more frequent in the DSRS group than in the ES group, but not more severe. Seven DSRS patients (17.5%) and 9 ES patients (23%) returned to drinking (P = NS). Five ES patients had esophageal stenosis that was successfully dilated. Ascites developed in 11 DSRS patients (27.5%) and in 19 ES patients (49%; P = 0.0521).
Table 2.
Comparison of the results of TMT, cancelling A's test and EEG. A’s test refers to the number of A's the patients has omitted to cancel in the test
| Preoperative | Long-term follow-up | P | |
| TMT (s) | |||
| DSRS | 55.3 ± 24.9 | 55.4 ± 27.9 | NS |
| ES | 60.1 ± 19.7 | 66.1 ± 40.1 | NS |
| A's test | |||
| DSRS | 4.9 ± 3.8 | 2.6 ± 2.5 | < 0.05 |
| ES | 5.5 ± 4.3 | 3.7 ± 3.4 | < 0.05 |
| EEG (% abnormal) | |||
| DSRS | 20% | 36% | < 0.05 |
| ES | 16% | 21% | NS |
NS: Not significant.
Long-term survival rates for shunt and ES groups were not statistically different according the log-rank test (Figure 3); however, a statistical difference was found by the Breslow test which better reflects the initial results. Causes of death are shown in Table 3: hepatocellular carcinoma became the primary cause of death with an increase in follow-up time (Figure 3). In the first five-year follow-up, the primary cause of death was liver failure (38%). No differences were found with respect to the etiology of liver cirrhosis: HCC developed in 35% of patients with non-alcoholic cirrhosis and in 32.5% of patients with alcoholic cirrhosis. Table 4 shows the results (actuarial survival curves and log-rank test) of the univariate analysis of some variables calculated at different follow-up intervals. By multivariate analysis according to Cox’s model, age over or below 53 years old was the only independent predictor of global survival rate.
Figure 3.
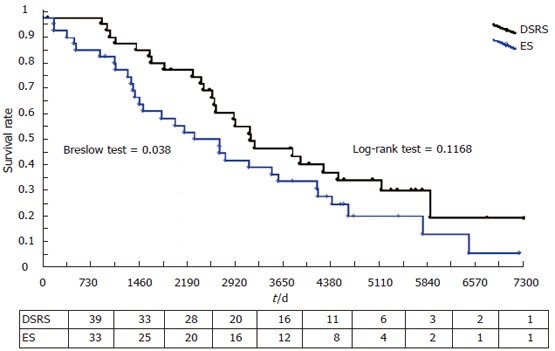
Actuarial survival curves for distal spleno-renal shunt (DSRS) and endoscopic sclerotherapy (ES). DSRS vs ES for the first 5 years (breslow test P = 0.038) while no differences were found in the final outcome (log rank test P = 0.1168)
Table 3.
Causes of death of patients submitted to DSRS (n = 26) or ES (n = 31)
| Causes of death | DSRS | ES |
| Digestive bleeding | 1 (4%) | 5 (16%) |
| Liver failure | 6 (23%) | 11 (36%) |
| Hepatocellular carcinoma | 13 (50%) | 10 (32%) |
| Other causes | 6 (23%) | 5 (16%) |
Table 4.
Results (actuarial survival curves and log-rank test) of the univariate analysis of some variables calculated during different interval of follow-up
| Variables | P (at 5 yr) | P (at 10 yr) | P (total follow-up) |
| Type of treatment (DSRS vs ES) | 0.0385 | 0.1415 | 0.1168 |
| Sex | 0.2186 | 0.3374 | 0.1943 |
| Child’s score (A vs B) | 0.0358 | 0.2533 | 0.1594 |
| Etiology of cirrhosis (non-alcohol vs alcohol) | 0.2891 | 0.0749 | 0.0438 |
| Portal perfusion | 0.2671 | 0.3579 | 0.3158 |
| Preop. Ascites | 0.3339 | 0.9022 | 0.9254 |
| Preop. encephalopathy | 0.6544 | 0.9857 | 0.8732 |
| Preop. Varices | 0.6513 | 0.4552 | 0.3858 |
| No. of previous bleeding | 0.1724 | 0.2739 | 0.1308 |
| Preop. Bilirubin | 0.2944 | 0.3358 | 0.0604 |
| Preop. GOT | 0.4504 | 0.2659 | 0.2553 |
| Preop. Prothrombin time | 0.2835 | 0.5629 | 0.4815 |
| Preop. Albumin | 0.7440 | 0.2133 | 0.1823 |
| Age (< 53 yr) | 0.1419 | 0.0431 | 0.0438 |
| Postop. Rebleeding | 0.1715 | 0.1168 | 0.0819 |
Preop: Preoperative; Postop: Postoperative.
DISCUSSION
The design of a randomized, controlled trial (RCT) comparing surgical treatment with a conservative therapy like ES, is often a complicated process requiring a choice of end-point, patient selection criteria, treatment schedules and methods of patient evaluation. In addition to our study[8], three other RCTs comparing DSRS to ES[5-7] have been published. They took different approaches to study these issues. It is true that survival is the primary end-point in prospective studies. In 2 studies[5,6] the definition of major end-point was not specified (survival, prevention of recurrent bleeding and maintenance of hepatic function) and no statistical method for determining trial size was used. The study of Terés[7] was designed to observe an increase in survival. However, the expected increase in survival appears to be too optimistic. On the basis of the available data[2,24,32-35], the sample requirements needed to show a realistic 10% increase in survival at 5 years is about 470 patients per group, applying standard power (80%), type I error (P < 0.05) and a two-tailed t-test[36].
Since gastro-esophageal rebleeding is considered the most life-threatening complication in ES, we wanted to verify whether DSRS was more effective in the prevention of rebleeding than ES and evaluate if this improvement affected survival. We limited the necessary recruitment to 20 patients per group, so the trial needed only one surgical team. This consideration is a general problem in surgical multicenter trials, as the surgeon’s skill is a major factor in the surgical outcome, especially in the case of a technically complex operation such as DSRS[37]. Our trial was undertaken after the team had acquired experience over 80 selective shunt procedures, to ensure a fairly good standardization of the surgical approach and intra- and post-operative treatment[24]. We then decided to increase the number of patients to be recruited to 40 patients per group in order to either eliminate the difference observed for the preoperative variables or carry out a subgroup analysis. The results of these trials[5-7] confirm previous results showing that DSRS is more effective in preventing variceal rebleeding than ES (Table 5). Either gastroduodenal lesions or esophageal varices can cause gastro-esophageal rebleeding after DSRS. The most common cause of variceal rebleeding is shunt thrombosis, but hemorrhage can also occur when the shunt is patent, because of renal vein hypertension[38].
Table 5.
2-yr survival and rebleeding rate in randomized controlled trials comparing DSRS with ES
| Warren[5] | Terés[7] | Rikkers[6] | Our data | |
| 2-yr survival rate | ||||
| after DSRS | 59%a | 71% | 65% | 95% |
| 2-yr survival rate | ||||
| after ES | 84%a | 68% | 61% | 85% |
| Child's C patients | 43% | 0 | 33% | 0 |
| Interval between bleeding | ||||
| and treatment (d) | > 3-5 | 10-15 | NR | 901 |
| Rebleeding rate after | ||||
| DSRS | 3%a | 14%a | 19%a | 2.5%a |
| Rebleeding rate after | ||||
| ES | 53%a | 37%a | 57%a | 35%a |
| Variceal eradication | ||||
| rate | NR | 46% | 63% | 90% |
| Failure to salvage | ||||
| rebleeders | 17% | 33% | 47% | 14% |
| Shunt for ES failure | 31% | 6% | 7% | 5% |
| Global mortality rate | ||||
| due to rebleeding | 3% | 14% | 27% | 16% |
| Global mortality rate | ||||
| due to other causes | 13% | 16% | 13% | 17% |
NR = Not reported; 1mean value;
P < 0.05 vs ES.
The problem of rebleeding in the ES group is complex and is connected with a number of factors, such as the number of patients with eradicated varices, the time interval required for eradication, the incidence of sclerosis-induced mucosal ulcerations of the esophageal wall, the variceal relapses after eradication and the incidence of hypertensive gastropathy[39]. Our incidence of rebleeding (35%) is similar to that reported by Terés[7] but lower compared to other studies[5,6]. The relevance of the difference in techniques in explaining these differences is not clear[40,41]. Different treatment intervals have been shown to affect the incidence of variceal rebleeding[42]. Finally, it is a common experience that early rebleeding occurs frequently in Child’s C patients[5] and the number of Child’s patients differed in all these RCTs.
The main complication in shunted patients was chronic HE that little affected ES patients. In the 4 RCTs the incidence of HE was higher in the DSRS group than in the ES group. This trend became significant in Terés’s study[7], probably due to the modified technique employed, which did not associate portal-azygos disconnection with the spleno-renal shunt. In fact, the entity of collaterals after DSRS seems to be an important factor influencing the incidence of HE[43,44]. In Rikkers’s[6] and Warren’s[5] studies chronic HE was probably attributed to the hepatic failure, and that was due to the fact that both Child’s C patients[5,6] and total shunts[6] were taken into consideration. In our preliminary study[8], the low rate of chronic HE in the DSRS group could be due to the recruitment of patients with good liver function and a shorter follow-up period than in other studies. In fact, the lengthening of the follow-up led to an increased risk of developing HE, above all in patients who underwent surgical shunt, but the quality of life was only slightly affected, as confirmed by the same incidence of hospitalization rate. In fact, the selective effect of DSRS prevented the onset of the severe form of chronic HE.
Two-year survival rate ranged from 59% to 95% in DSRS and from 61% to 90% in the ES group (Table 5). Where do these great differences stem from The different incidence in these studies for two prognostic factors (Child’s class C patients and the interval between hemorrhage and treatment) can explain these results[45]. However, a more important factor is present in the ES group: the fate of the patient after variceal rebleeding (Table 5). The fact that some studies[6,7] do not have available a good therapeutic option available in case of ES failure can influence these results. The better survival rate reported in Warren’s study[5] seems to be due to the large number of ES patients who underwent shunt surgery (10 out of 36 patients) with low operative mortality (10%). This advantage was not shown in the other studies[6,7].
The lack of statistical difference observed in our study was also confirmed by meta-analysis of the four RCTs: the overall risk of death following DSRS was only marginally lower in comparison to that following ES (0.78 odds ratio; 95% CI: 0.47-1.29). In this study, we found a statistically improved survival following DSRS with the Breslow test; it gives more emphasis to early deaths occurring in the ES group. When lengthening the follow-up period, the survival curves become more similar and the risk of rebleeding does not increase with increasing follow-up time, while the appearance of HCC heavily influenced long-term survival in both groups, becoming the primary cause of death. The Breslow test better reflects initial results while the log-rank test more accurately characterizes final outcome.
In contrast with a recent study[46], our analysis did not find any significant differences regarding the development of HCC (44% in DSRS group vs 42% in ES group even though there was a higher proportion of patients’ deaths due to HCC (50% of all the causes of death in the DSRS group vs 32% in the ES group). This finding should be interpreted cautiously since this trial was not specifically designed to evaluate the effect of DSRS or ES on the development of HCC. In any case, it is possible that the surgical access of the DSRS could promote an HCC diagnosis at a more advanced stage and prevent the use of specific therapies for HCC, such as radiofrequency (through a percutaneous or a laparoscopic approach) or surgical resections. Another study[47] concluded that DSRS was not a problem preventing safe performance of therapies for the HCC that developed during the follow-up period. On the other hand, it has been shown that patients with esophageal variceal bleeding who underwent ES had a high risk of developing HCC with an adverse impact on survival[48]. Further studies are necessary to evaluate the correlations between the therapies for portal hypertension and the appearance of HCC. Furthermore, in our analysis, no differences were found regarding the etiology of liver cirrhosis, although it is not possible to know how many patients had an HCV-related cirrhosis because the test has only been used in our Department since 1991. Hepatitis C disease has assumed increasing importance over the past years and undoubtedly contributed to cirrhosis and HCC in patients with cryptogenic or alcoholic liver disease before serologic markers became routinely available.
Multivariate analysis by Cox’s model found that the only factor contributing independently to the estimation of prognosis was the age of patients at the time of inclusion in the study (Hazard risk: 2.339; coefficient beta: 0.849; T-value: 2.729). That age was a prognostic variable is not surprising, since it reflects a longer duration of follow-up.
Meanwhile, in 2006, what is the lesson provided by the analysis of such a long-term follow-up study First of all, although it is clear that all patients who survive a variceal bleeding should be treated with beta-blockers or endoscopic band ligation, which appears to be better than ES in preventing rebleeding, it is also clear that all patients in whom bleeding cannot be controlled or who continue to rebleed can be treated with salvage TIPSS or shunt surgery, even though some studies seem to show the superiority of surgical over angiographic shunt in good-risk patients[11,49]. Secondly, although the number of patients who have uncontrolled rebleeding following beta-blockers or endoscopic band ligation are very few, it is important that there be centers with qualified surgeons who can offer DSRS to selected patients to guarantee long-term survival comparable to that obtained by liver transplantation. Finally, it is important to underline that, in the evaluation of chronic disease with multiple complications such as liver cirrhosis, the time factor should be considered and the effect of each therapy should also be analyzed over a long-term follow-up period. This work confirms that it is possible to perform a shunt procedure without impairing liver function or the prognosis of the cirrhotic patient.
Footnotes
S- Editor Wang J L- Editor Lutze M E- Editor Bai SH
References
- 1.Warren WD, Zeppa R, Fomon JJ. Selective trans-splenic decompression of gastroesophageal varices by distal splenorenal shunt. Ann Surg. 1967;166:437–455. doi: 10.1097/00000658-196709000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henderson JM, Millikan WJ, Warren WD. The distal splenorenal shunt: an update. World J Surg. 1984;8:722–732. doi: 10.1007/BF01655769. [DOI] [PubMed] [Google Scholar]
- 3.Spina GP, Galeotti F, Opocher E, Santambrogio R, Cucchiaro G, Lopez C, Pezzuoli G. Selective distal splenorenal shunt versus side-to-side portacaval shunt. Clinical results of a prospective, controlled study. Am J Surg. 1988;155:564–571. doi: 10.1016/s0002-9610(88)80411-2. [DOI] [PubMed] [Google Scholar]
- 4.Spina G, Santambrogio R, Opocher E, Galeotti F, Cucchiaro G, Strinna M, Pezzuoli G. Improved quality of life after distal splenorenal shunt. A prospective comparison with side-to-side portacaval shunt. Ann Surg. 1988;208:104–109. doi: 10.1097/00000658-198807000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henderson JM, Kutner MH, Millikan WJ Jr, Galambos JT, Riepe SP, Brooks WS, Bryan FC, Warren WD. Endoscopic variceal sclerosis compared with distal splenorenal shunt to prevent recurrent variceal bleeding in cirrhosis. A prospective, randomized trial. Ann Intern Med. 1990;112:262–269. doi: 10.7326/0003-4819-112-4-262. [DOI] [PubMed] [Google Scholar]
- 6.Rikkers LF, Jin G, Burnett DA, Buchi KN, Cormier RA. Shunt surgery versus endoscopic sclerotherapy for variceal hemorrhage: late results of a randomized trial. Am J Surg. 1993;165:27–32; discussion 32-33. doi: 10.1016/s0002-9610(05)80400-3. [DOI] [PubMed] [Google Scholar]
- 7.Terés J, Bordas JM, Bravo D, Visa J, Grande L, Garcia-Valdecasas JC, Pera C, Rodés J. Sclerotherapy vs. distal splenorenal shunt in the elective treatment of variceal hemorrhage: a randomized controlled trial. Hepatology. 1987;7:430–436. doi: 10.1002/hep.1840070303. [DOI] [PubMed] [Google Scholar]
- 8.Spina GP, Santambrogio R, Opocher E, Cosentino F, Zambelli A, Passoni GR, Cucchiaro G, Macrì M, Morandi E, Bruno S. Distal splenorenal shunt versus endoscopic sclerotherapy in the prevention of variceal rebleeding. First stage of a randomized, controlled trial. Ann Surg. 1990;211:178–186. doi: 10.1097/00000658-199002000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spina GP, Henderson JM, Rikkers LF, Teres J, Burroughs AK, Conn HO, Pagliaro L, Santambrogio R. Distal spleno-renal shunt versus endoscopic sclerotherapy in the prevention of variceal rebleeding. A meta-analysis of 4 randomized clinical trials. J Hepatol. 1992;16:338–345. doi: 10.1016/s0168-8278(05)80666-x. [DOI] [PubMed] [Google Scholar]
- 10.de Franchis R, Dell'Era A, Iannuzzi F. Diagnosis and treatment of portal hypertension. Dig Liver Dis. 2004;36:787–798. doi: 10.1016/j.dld.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Rosemurgy AS, Bloomston M, Clark WC, Thometz DP, Zervos EE. H-graft portacaval shunts versus TIPS: ten-year follow-up of a randomized trial with comparison to predicted survivals. Ann Surg. 2005;241:238–246. doi: 10.1097/01.sla.0000151884.67600.b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papatheodoridis GV, Goulis J, Leandro G, Patch D, Burroughs AK. Transjugular intrahepatic portosystemic shunt compared with endoscopic treatment for prevention of variceal rebleeding: A meta-analysis. Hepatology. 1999;30:612–622. doi: 10.1002/hep.510300316. [DOI] [PubMed] [Google Scholar]
- 13.Luca A, D'Amico G, La Galla R, Midiri M, Morabito A, Pagliaro L. TIPS for prevention of recurrent bleeding in patients with cirrhosis: meta-analysis of randomized clinical trials. Radiology. 1999;212:411–421. doi: 10.1148/radiology.212.2.r99au46411. [DOI] [PubMed] [Google Scholar]
- 14.de Franchis R, Primignani M. Endoscopic treatments for portal hypertension. Semin Liver Dis. 1999;19:439–455. doi: 10.1055/s-2007-1007131. [DOI] [PubMed] [Google Scholar]
- 15.Bosch J, Abraldes JG, Groszmann R. Current management of portal hypertension. J Hepatol. 2003;38 Suppl 1:S54–S68. doi: 10.1016/s0168-8278(02)00430-0. [DOI] [PubMed] [Google Scholar]
- 16.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 17.Nordlinger BM, Nordlinger DF, Fulenwider JT, Millikan WJ, Sones PJ, Kutner M, Steele R, Bain R, Warren WD. Angiography in portal hypertension: clinical significance in surgery. Am J Surg. 1980;139:132–141. doi: 10.1016/0002-9610(80)90242-1. [DOI] [PubMed] [Google Scholar]
- 18.Pocock SJ. Clinical trials. A practical approach. Chichester: John Wiley & Sons; 1983. [Google Scholar]
- 19.Capussotti L, Vergara V, Polastri R, Bouzari H, Galatola G. Liver function and encephalopathy after partial vs direct side-to-side portacaval shunt: a prospective randomized clinical trial. Surgery. 2000;127:614–621. doi: 10.1067/msy.2000.105861. [DOI] [PubMed] [Google Scholar]
- 20.The general rules for recording endoscopic findings on esophageal varices. Jpn J Surg. 1980;10:84–87. doi: 10.1007/BF02468653. [DOI] [PubMed] [Google Scholar]
- 21.Reitan RM. Validity of the trial making test as an indication of organic brain damage. Percept Mot Skills. 1958;8:271–274. [Google Scholar]
- 22.Neisser V. Cognitive psychology. New York: Appleton Century Crofts; 1967. pp. 99–115. [Google Scholar]
- 23.Conn HO, Leevy CM, Vlahcevic ZR, Rodgers JB, Maddrey WC, Seeff L, Levy LL. Comparison of lactulose and neomycin in the treatment of chronic portal-systemic encephalopathy. A double blind controlled trial. Gastroenterology. 1977;72:573–583. [PubMed] [Google Scholar]
- 24.Pezzuoli G, Spina G, Santambrogio R, Galeotti F, Opocher E, Cucchiaro G, Lopez C, Strinna M. The distal splenorenal shunt: an update on experience of 106 cases. Int Surg. 1987;72:144–148. [PubMed] [Google Scholar]
- 25.Warren WD, Millikan WJ. Selective transsplenic decompres-sion procedure changes in technique after 300 cases. Contemp Surg. 1981;18:11–30. [Google Scholar]
- 26.Warren WD, Millikan WJ Jr, Henderson JM, Abu-Elmagd KM, Galloway JR, Shires GT 3rd, Richards WO, Salam AA, Kutner MH. Splenopancreatic disconnection. Improved selectivity of distal splenorenal shunt. Ann Surg. 1986;204:346–355. doi: 10.1097/00000658-198610000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pezzuoli G, Cosentino F, Zannini P, Baisi A, Rubis Passoni G, Morandi E, Santambrogio R, Galeotti F, Opocher E. La sclerosi endoscopica delle varici esofagee. In: Gozzetti G, Pierangeli A, Esserre P, editors. progressi in chirurgia. Bologna; 1986. pp. 331–336. [Google Scholar]
- 28.Hosking SW, Kennedy HJ, Seddon I, Triger DR. The role of propranolol in congestive gastropathy of portal hypertension. Hepatology. 1987;7:437–441. doi: 10.1002/hep.1840070304. [DOI] [PubMed] [Google Scholar]
- 29.Peto R, Pike MC, Armitage P, Breslow NE, Cox DR, Howard SV, Mantel N, McPherson K, Peto J, Smith PG. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. analysis and examples. Br J Cancer. 1977;35:1–39. doi: 10.1038/bjc.1977.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cox DR. Regression models and life tables. J R Stat Soc Ser B. 1972;34:187–220. [Google Scholar]
- 31.Mazumdar M, Smith A, Bacik J. Methods for categorizing a prognostic variable in a multivariable setting. Stat Med. 2003;22:559–571. doi: 10.1002/sim.1333. [DOI] [PubMed] [Google Scholar]
- 32.Terblanche J, Bornman PC, Kahn D, Jonker MA, Campbell JA, Wright J, Kirsch R. Failure of repeated injection sclerotherapy to improve long-term survival after oesophageal variceal bleeding. A five-year prospective controlled clinical trial. Lancet. 1983;2:1328–1332. doi: 10.1016/s0140-6736(83)91090-5. [DOI] [PubMed] [Google Scholar]
- 33.Sclerotherapy after first variceal hemorrhage in cirrhosis. A randomized multicenter trial. The Copenhagen Esophageal Varices Sclerotherapy Project. N Engl J Med. 1984;311:1594–1600. doi: 10.1056/NEJM198412203112502. [DOI] [PubMed] [Google Scholar]
- 34.Korula J, Balart LA, Radvan G, Zweiban BE, Larson AW, Kao HW, Yamada S. A prospective, randomized controlled trial of chronic esophageal variceal sclerotherapy. Hepatology. 1985;5:584–589. doi: 10.1002/hep.1840050410. [DOI] [PubMed] [Google Scholar]
- 35.Westaby D, Macdougall BR, Williams R. Improved survival following injection sclerotherapy for esophageal varices: final analysis of a controlled trial. Hepatology. 1985;5:827–830. doi: 10.1002/hep.1840050520. [DOI] [PubMed] [Google Scholar]
- 36.Pocock SJ. Clinical trials. A practical approach. Chichester: John Wiley & Sons; 1983. [Google Scholar]
- 37.Warren WD, Millikan WJ Jr, Henderson JM, Wright L, Kutner M, Smith RB 3rd, Fulenwider JT, Salam AA, Galambos JT. Ten years portal hypertensive surgery at Emory. Results and new perspectives. Ann Surg. 1982;195:530–542. doi: 10.1097/00000658-198205000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Richards WO, Pearson TC, Henderson JM, Millikan WJ Jr, Warren WD. Evaluation and treatment of early hemorrhage of the alimentary tract after selective shunt procedures. Surg Gynecol Obstet. 1987;164:530–536. [PubMed] [Google Scholar]
- 39.Fleig WE, Stange EF, Hunecke R, Schönborn W, Hurler U, Rainer K, Gaus W, Ditschuneit H. Prevention of recurrent bleeding in cirrhotics with recent variceal hemorrhage: prospective, randomized comparison of propranolol and sclerotherapy. Hepatology. 1987;7:355–361. doi: 10.1002/hep.1840070224. [DOI] [PubMed] [Google Scholar]
- 40.Westaby D, Macdougall BR, Melia W, Theodossi A, Williams R. A prospective randomized study of two sclerotherapy techniques for esophageal varices. Hepatology. 1983;3:681–684. doi: 10.1002/hep.1840030509. [DOI] [PubMed] [Google Scholar]
- 41.Sarin SK, Sachdev G, Nanda R, Batra SK, Anand BS. Comparison of the two time schedules for endoscopic sclerotherapy: a prospective randomised controlled study. Gut. 1986;27:710–713. doi: 10.1136/gut.27.6.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Villeneuve JP. Prognostic factors for rebleeding in patients with variceal hemorrhage. In: Burroughs AK, editor. Methodology and reviews of clinical trials in portal hypertension. Amsterdam: Excerpta medica; 1986. pp. 161–167. [Google Scholar]
- 43.Vang J, Simert G, Hansson JA, Thylen U, Bengmark TS. Results of a modified distal spleno-renal shunt for portal hypertension. Ann Surg. 1977;185:224–228. doi: 10.1097/00000658-197702000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rigau J, Terés J, Visa J, Bosch J, Conesa A, Grande L, Vilar JA, García-Valdecasas JC, Pera C. Long term follow-up of 100 patients with portal hypertension treated by a modified splenorenal shunt. Br J Surg. 1986;73:708–711. doi: 10.1002/bjs.1800730911. [DOI] [PubMed] [Google Scholar]
- 45.Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology. 1981;80:800–809. [PubMed] [Google Scholar]
- 46.Bañares R, Núñez O, Escudero M, Fernández C, Vaquero J, Beceiro I, Echenagusía A, Clemente G, Santos L. Patients with cirrhosis and bare-stent TIPS may have increased risk of hepatocellular carcinoma. Hepatology. 2005;41:566–571. doi: 10.1002/hep.20576. [DOI] [PubMed] [Google Scholar]
- 47.Hirano S, Kondo S, Omi M, Anbo Y, Katoh H. Treatment of hepatocellular carcinoma occurring after distal splenorenal shunt for esophagogastric varices. Hepatogastroenterology. 2001;48:1110–1113. [PubMed] [Google Scholar]
- 48.Chen WC, Lo GH, Lai KH, Cheng JS, Hsu PI, Lin CK. Development of hepatocellular carcinoma after successful management of esophageal variceal bleeding. J Chin Med Assoc. 2004;67:557–564. [PubMed] [Google Scholar]
- 49.Helton WS, Maves R, Wicks K, Johansen K. Transjugular intrahepatic portasystemic shunt vs surgical shunt in good-risk cirrhotic patients: a case-control comparison. Arch Surg. 2001;136:17–20. doi: 10.1001/archsurg.136.1.17. [DOI] [PubMed] [Google Scholar]


