Abstract
Background:
To analyse the mode of delivery in trial of labour (TOL), incidence of successful vaginal deliveries and indications of repeat caesarean section (CS).
Materials and Methods:
Prospective selective study. Study population consisted of 367 pregnant women with previous one lower segment caesarean section (LSCS) in reproductive age group. These were grouped in to three groups, Group 1 (n = 239): Women, who were elected for repeat CS without a TOL. Group 2 (n = 76): Women, who were given TOL and delivered vaginally. Group 3 (n = 52): Women, who were given a TOL but due to failed trial, had to be taken for emergency repeat section. The maternal and foetal outcome was studied in all the groups.
Statistical Method Used:
The data was entered in the Microsoft excel worksheet, values expressed as mean ± SD. Chi-square test was done to compare the categorical variables among the groups. ANOVA (one-way analysis of variance) was done to compare the baseline characteristics of patients and time to delivery among the groups.
Results:
Out of 128 women who were given TOL, 76 (59.37%) vaginal birth after caesarean (VBAC) occurred, out of which 40 (52.63%) had spontaneous vaginal deliveries without augmentation of labour and 36 (47.36%) subjects had augmentation of labour with artificial rupture of membranes (ARMs) and oxytocin. A total of 52 women (40.62%) underwent emergency LSCS.
Conclusion:
Proper selection and counselling about clinically significant risks, women can be given TOL with careful monitoring and taken for emergency LSCS on minimal indication is the best answer to management of previous one CS in labour.
Keywords: Caesarian section, safe, trial of labour, vaginal birth after caesarean section
INTRODUCTION
In the past decade, the rate of caesarean sections (CSs) has risen. Previous caesareans delivery seems to be the main cause of an increase in the number of CS nowadays. In obstetrics practice, one of the major topics of debate is decision making in caesarean birth. A history of previous caesarean birth creates more difficulty in such situation. Before 1970, deliveries by CS were considered as indication for CS in subsequent pregnancies, reflecting a concern that uterine scar tissue might rupture during labour. In the 1980s, the dictum ‘once a caesarean always caesarean’, espoused by Craigin in 1916, was revised in many countries and a trial of labour (TOL) in women with history of CS was proposed in an attempt to reduce repeat CS.1,2 However, an apparent increase in incidence of uterine rupture and concern about maternal and foetal safety has challenged the choice of vaginal delivery in women having a scarred uterus. Consequently, clinicians are increasingly being faced in deciding the mode of delivery in pregnant women whose first delivery was by CS. Our medical college caters rural population also in large numbers, who soon return to work in puerperium, for them repeat CS would increase the time of convalescence and delay in return to work. Therefore, through this study effort has been made to score in vaginal birth following CS in selected cases.
MATERIALS AND METHODS
This prospective study was conducted in department of Obstetrics and Gynaecology, from November 2007 to October 2009. Out of the total 587 women with term pregnancy with one previous CS, admitted for delivery, 367 subjects were taken in study, based on inclusion and exclusion criteria. The criteria taken in consideration are: Inclusion Criteria — Women, with one previous lower segment caesarean section (LSCS), live pregnancy with haemoglobin ≥8 g/dl. Exclusion Criteria — Women with gestational age <34 weeks, intrauterine foetal death (IUD), live pregnancy with haemoglobin <8 g/dl and other medical disorder. Women (n = 376) who were admitted for safe confinement who met the study criteria were consecutively recruited. All subjects were analysed prospectively and data was collected in a proforma, meeting the objectives of study. Thus, 367 women included in study were grouped in to Group 1 (n = 239): Women, who were elected for repeat CS without a TOL. Group 2 (n = 76): Women, who were given a TOL and delivered vaginally. Group 3 (n = 52): Women, who were given a TOL but due to failed trial, had to be taken for emergency repeat section. The word elective repeat caesarean section (ERCS) here refers either to the women being taken for repeat section directly without TOL electively or on emergency basis when the woman was already in labour. TOL refers to trial for vaginal delivery, which may end as successful vaginal birth after caesarean (VBAC) or failed TOL resulting in repeat section. Thorough history was elicited from all subjects as per the proforma. All study subjects were analysed in full details regarding age, parity, previous obstetric performance including number of vaginal deliveries prior to this pregnancy, the indication for LSCS and institution where the woman underwent LSCS. History of intra-operative and post-operative complication was also noted, which could have bearing in future obstetric care. Regarding the present pregnancy, details about the number of antenatal visits, any ante partum complications were noted. Menstrual history to know the period of gestation was noted. A detailed general, physical, systemic and obstetric examination was done. Per abdominal examination was done to estimate the period of gestation, amount of liquor, to rule out any malpresentation, to estimate the expected foetal weight and condition of scar and foetal cardiac activity. Per vaginal examination was done to note the dilatation, effacement of cervix, station of presenting part and adequacy of pelvis for vaginal delivery. All women underwent routine haematological investigations. Ultrasonogram was used to correlate with menstrual age and foetal well-being. After ruling out contraindication, for vaginal delivery and ensuring that there was no obvious fetopelvic disproportion women with gestational age up to 40 weeks were allowed for TOL. Patient allowed for VBAC-TOL were carefully monitored in intra-partum period for any sign of impending rupture like tachycardia, hypotension, scar tenderness, vaginal bleeding, foetal heart rate (FHR) variability by continuous cardiotropographic monitor (CTG), haematuria, etc. Progress of labour was noted with cervical dilatation, effacement, descent of head and uterine contraction. Labour was accelerated with artificial rupture of membrane (ARM) in active labour whenever required. Oxytocin was also used in few subjects for acceleration of labour, with carefully monitoring of foetal cardiac activity by CTG and assessing integrity of previous caesarean scar clinically, and careful vital monitoring. Following ARM, colour and quality of liquor was noted. In third stage, routine scar exploration was deferred until indicated, for example excessive bleeding, uterus not contracting. Few subjects that had undergone a TOL required repeat CS due to various indications. In subjects where rupture was suspected, TOL was immediately abandoned and taken for emergency laparotomy and necessary steps were taken promptly. Women (n = 239) were taken for direct caesarean for various indications without TOL. The subjects admitted to antenatal ward for ERCS were taken for CS after required preparation. However, some of them had gone into labour before they could be taken electively and they were taken for LSCS in emergency directly without TOL. Women, who had come in labour with known indication of repeat LSCS, were also taken electively for LSCS in emergency without TOL. Institutional ethical clearance was obtained prior to the study.
Statistical method used
The data was entered in the Microsoft Excel worksheet, values expressed as mean ± SD. Chi-square test was done to compare the categorical variables among the groups. One-way analysis of variance (ANOVA) was done to compare the baseline characteristics of patients and time to delivery among the groups. Median Bishop score difference among the groups was analysed using Kruskal-Wallis non-parametric. P value <0.05 was considered significant.
RESULTS
Total number of deliveries including CSs was 15,013, out of this 13,190 delivered vaginally, 1823 delivered by CS; total number of antenatal women with previous LSCS was 587. A total of 356 women had repeat CS. A total of 187 women underwent VBAC. Hence incidence of CS in study period of 2 years was 12.14%, previous CS was 3.33% and repeat CS was 19.5%.
Total number of antenatal women with previous one LSCS was 587. Out of the 587 women of previous LSCS, 128 women met the study inclusion criteria. Maximum (85.65%) women were aged between 20 and 30 years. Most of the women were from villages i.e 85.83%. 65.12% women had no prior antenatal booking i.e they were unbooked and were unsupervised prior to this admission. A total of 52.3% women were from lower socioeconomic status. A total of 73.84% women were >37 weeks of gestational age and 7.6% were >40 weeks of gestation.
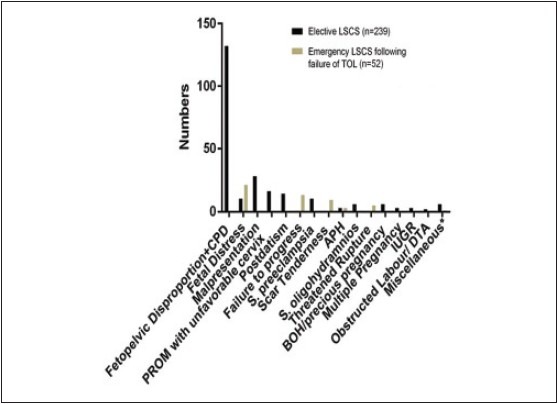
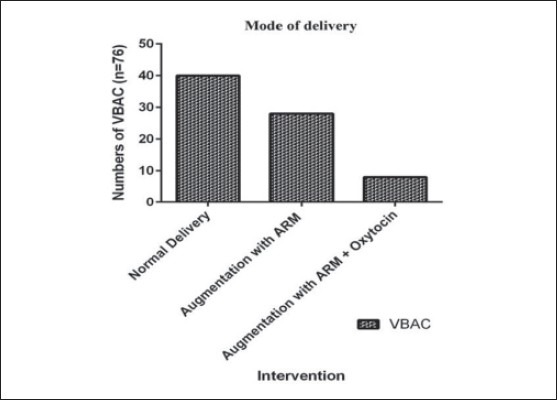
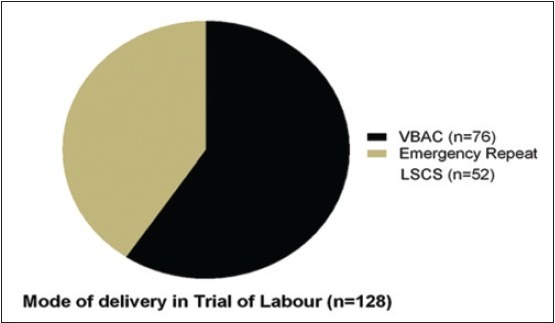
Out of 128 cases, who were given TOL, vaginal birth occurred in 76 (59.37%) and 52 cases (40.62%) underwent emergency LSCS. Out of 59.37% of successful VBAC, 52.63% delivered without augmentation of labour. A total of 47.36% women required augmentation of labour with ARMs and oxytocin [Figures 1 and 2].
Figure 1.
Mode of Delivery
Figure 2.
Mode of delivery in trial of labour
Various indications for ERCS in women following TOL is shown in [Table 1] and in [Figures 3 and 4]. Commonest being fetopelvic disproportion (FPD) 45.36%. In the present study, incidence of scar dehiscence was higher following TOL than elective repeat LSCS (9.62% Vs. 1.62%), which was statistically significant (P = <0.005). The incidence of scar dehiscence is only 9.62% in the present study and it was clinically detected, the women were immediately taken for emergency.
Table 1.
Indication of Repeat Caesarean Section
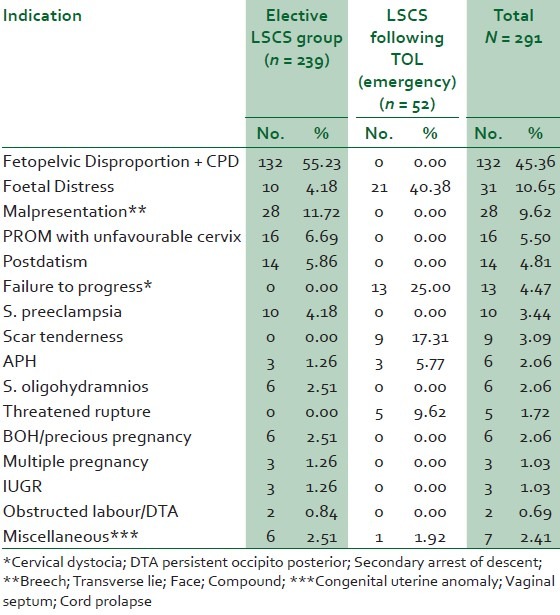
Figure 3.
Indications of repeat elective and emergency caesarean section
Figure 4.
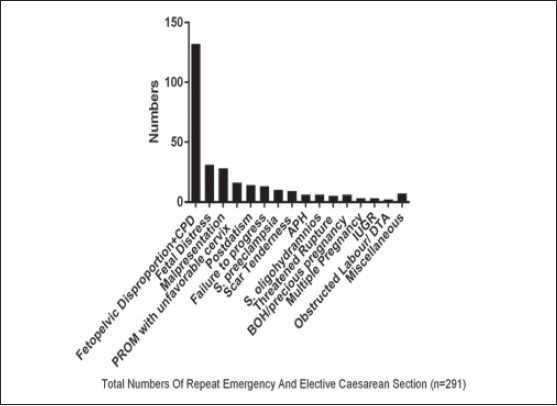
Total numbers of repeat emergency and elective Caesarean section
Rupture uterus was seen in only two women undergoing TOL, none of the women in the other group had rupture uterus.
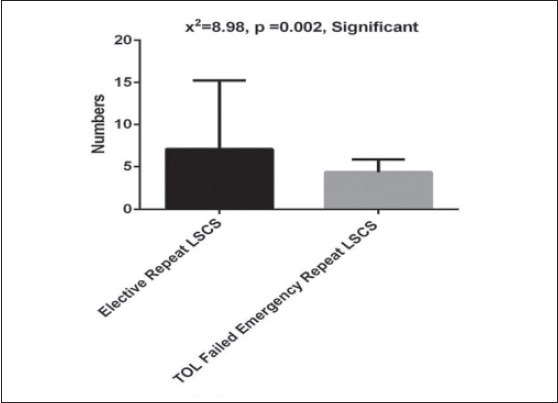
On opening the abdomen, 11.68% had adhesions. In emergency LSCS following TOL other findings like thinned out Lower uterine segment (LUS) (7.56%) and bladder advancement/oedema (4.12%) were more common. Complications such as difficulty in delivery of baby (11.54%), change of uterine incision (9.62%), extension of uterine incision (5.77%), use of haemostatic suture (7.69%) and incomplete rupture (3.85%) were also seen in emergency LSCS [Table 2]. Maternal morbidity in the form of fever (7.89%), wound sepsis (10.53%), need of blood transfusion (7.89%) and paralytic ileus (2.63%) were more in emergency LSCS following TOL [Table 2, Figure 5].
Table 2.
Intra-operative findings, complications and modification
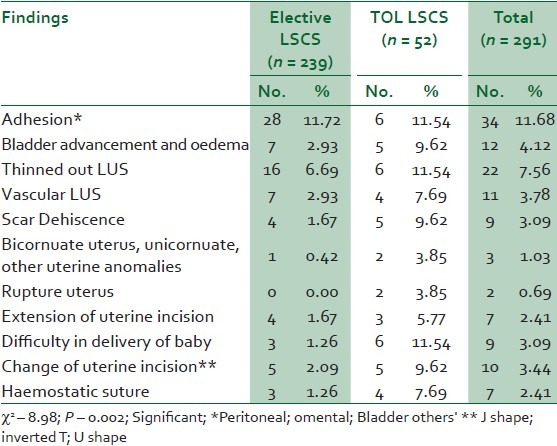
Figure 5.
Intra-operative findings, complications and modifications
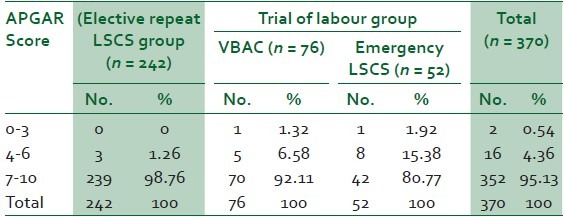
Table 3 shows that maximum (98.76%) babies in the ERCS group were healthy with Apgar score between 7 and 10, and only (1.26%) had Apgar <7. While in TOL group, (87.5%) had Apgar 7-10, (10.1%) with Apgar 4-6 and (0.54%) Apgar at 5 min, ≤3.
Table 3.
Analysis of APGAR Score Of newborn at 5 min
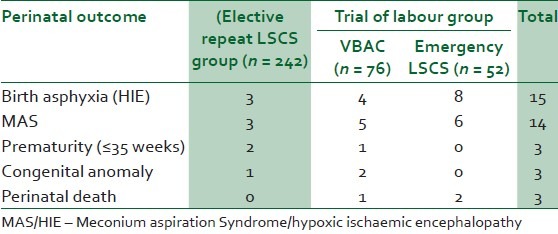
It is evident from [Table 4] that perinatal morbidity occurred in 35/370 (9.45%). Out of them, 15/35 babies had birth asphyxia14/35 Meconium Aspiration Syndrome (MAS), 3 babies were premature, 3 had congenital anomalies with 3 peri-natal deaths.
Table 4.
Perinatal Outcome
In the present study, 73.84% women were of gestational age >37-40 weeks. Out of 16 subjects with history of vaginal birth prior to CS, 10 (62.5%) underwent VBAC and 6 (37.5%) underwent emergency LSCS, whereas out of 14 subjects with history of post-CS birth 9 (64.28%) delivered vaginally and 5 (35.71%) taken in for emergency CS.
DISCUSSION
CS rates have steadily risen from 10% of all deliveries in the 1980s to21.3% of births in the United Kingdom (RCOG 2001),3 the primary caesarean delivery rate has increased from 14.5% in 1996 to 23.4% in 2007.4 Planned ERCS and planned induction of labour for women with a prior caesarean birth are both associated with benefits and harms. In the present study, incidence of CS was 12.14% for primary CS, as recommended by American College of Obstetricians and Gynaecologists Task Force.5 Repeat caesarean delivery and those performed for dystocia have been the leading indications in Western industrialised countries, similar in our study.6,7
In the present study, TOL was given in 128 women [Figures 1 and 2], out of which 76 delivered vaginally, contribution to VBAC success rate of 59.37%. A total of 40.62% women underwent emergency LSCS. The repeat caesarean rate was high in our study group. This is because unlike in Western literature,2 our women belonged to younger age group in maximum number (20-30 years), which reflects early age of marriage and conception and majority of women (86.64%) belonged to rural areas with less literacy rate. Referred subjects coming from rural area usually come in late labour without prior antenatal check-ups. Maximum number of subjects had no documentation of their previous CS, which made decision for TOL difficult and usually trial culminated in CS after a short trial because most of the patients had taken trial at home, so there occurred apprehension in doctor on duty for further trial and fear of putting woman in further calamity, contributed for much higher rate of repeat CS.
In our study, only 11.71% subjects were properly booked. In the present study, majority of women (65.12%) were unbooked, (22.88%) were partly booked, that is, less than three visits in antenatal clinics. In unbooked women, proper antenatal counselling was lacking, women not being admitted in appropriate time, unavailability of documents related to previous surgery, reduced confidence in giving consent for TOL.
Women who were booked in private clinics usually denied for TOL during counselling related to morbidity. In the present study, 192 (52.31%) women belonged to lower socio-economic status and 159 (43.32%) belonged to middle socio-economic status. This could be because of belief of general public that post-caesarean pregnancy could result in repeat section, which would be performed in low cost in government institution while some women come forward for vaginal delivery, which is usually favoured by faculty associated to medical college. Only 4.36% women were of higher socio-economic group who were mentally prefixed for repeat section.
In the present study, women with history of previous vaginal deliveries and one CS have more chances of success for TOL, as out of 14 subjects with history of post-CS birth 9 (64.28%) delivered vaginally and 5 (35.71%) taken in for emergency CS.
In 52 (40.62%) subjects, a trial was abandoned and was taken for emergency LSCS, for various obstetrical indications. Comparable to the present study VBAC success rate was 63.83% in study conducted by Agrawal et al., from India.7
Uterine rupture in TOL group was 0.7%, uterine dehiscence in 0.7% in TOL, 0.5% in ERCS group in a study.8 In the present study, incidence of scar dehiscence was higher following TOL than elective repeat LSCS (9.62% Vs. 1.62%), which was statistically significant (P = <0.005) and comparable to other studies. The incidence of scar dehiscence was 9.62% in the present study and it was clinically detected, maximum were incomplete (70%), the women were immediately taken for emergency CS and no maternal or foetal morbidity occurred due to scar dehiscence. Rupture uterus was seen in only 2/128 women undergoing TOL, none of the women in the other group had rupture uterus. The rupture site required only repair with no foetal mortality as it was detected timely and laparotomy performed within 15 min.
In emergency LSCS following TOL, other findings like thinned out LUS (7.56%) and bladder advancement/oedema (4.12%) were more common. Complications such as difficulty in delivery of baby (11.54%), change of uterine incision (9.62%), extension of uterine incision (5.77%), use of haemostatic suture (7.69%) were also seen in emergency LSCS [Table 2].
Maternal morbidity in the form of fever (7.89%), wound sepsis (10.53%), need of blood transfusion (7.89%) and paralytic ileus (2.63%) were more in emergency LSCS following TOL.
In a study in 2002, risk of delivery-related perinatal death was 1.3 per 1000 among the 15,515 women who attempted VBAC. Although the absolute risk was again small, this rate was 11 times greater than the risk of perinatal death in 9014 women who planned repeat caesarean delivery.9 In contrast, in the present study perinatal morbidity occurred in 35/370 (9.45%). Out of them 15/35 babies had birth asphyxia14/35 MAS, 3 babies were premature, 3 had congenital anomalies with 3 perinatal deaths, comparable to babies born to emergency CS group. This may be due to proper monitoring and less number enrolled for study group.
Collectively from all data absolute risk of uterine rupture attributable to a TOL resulting in death or injury to the foetus is approximately 1 per 1000.2 In contrast, there was no foetal death due to rupture or dehiscence.
Among women with a previous low transverse CS, induction of labour is not associated with significantly higher rates of uterine rupture compared with spontaneous labour, provided a consistent protocol with strict criteria for intervention is adopted.10 M Maternal morbidity in the form of fever (7.89%), wound sepsis (10.53%), need of blood transfusion (7.89%) and paralytic ileus (2.63%) were more in emergency LSCS following TOL in the present study. Most studies suggest that the maternal mortality rate does not differ significantly between women undergoing a TOL compared with those undergoing an ERCS.8,11 Conversely, Landon et al.,8 observed that the risks of transfusion and infection were significantly greater for women attempting a TOL. Rossi and D’Addario reported similar findings in their meta-analysis. McMahon et al., in a population-based study of 6138 women, found that major complications - hysterectomy, uterine rupture or operative injury - were almost twice as common in women undergoing a TOL compared with those undergoing an elective second caesarean delivery.12,13
CONCLUSION
TOL in previous CS is like a double-edged sword, if the woman achieves VBAC, she has the benefits of short hospital stay, decreased morbidity and less expenditure. Considering the fact that foetal morbidity and mortality due to TOL is comparable with the women labouring without a scar, TOL may be encouraged. Women decided for TOL must be thoroughly assessed before allowing for TOL. It is concluded from this study that after proper selection and counselling about clinically significant risks, benefits and alternatives in an understandable and unbiased form and consent, women can be given TOL with careful monitoring and taken for emergency LSCS on minimal indication and is the best answer to management of previous one CS in labour.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Cragin E. Conservation in Obstetrics. N Y Med J. 1961;140:1. [Google Scholar]
- 2.Cunningham GF, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY. Prior caesarian delivery. In: F Cunningham GF, editor. Williams Obstetrics. 23rd ed. New York: McGraw Hill; 2010. pp. 565–76. [Google Scholar]
- 3.Dodd JM, Crowther CA. Elective repeat caesarean section versus induction of labour for women with a previous caesarean birth. Cochrane Database Syst Rev. 2012;16:5. doi: 10.1002/14651858.CD004906.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Boyle A, Reddy UM. Epidemiology of cesarean delivery: The scope of the problem. Semin Perinatol. 2012;36:308–14. doi: 10.1053/j.semperi.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 5.American College of Obstetricians and Gynecologists, Task Force on Cesarean Delivery Rates: Evaluation of cesarean delivery. Washington, DC: ACOG; 2000. [Google Scholar]
- 6.Notzon FC, Cnattingius S, Bergsjø P, Cole S, Taffel S, Irgens L, et al. Cesarean section delivery in the 1980s: International comparison by indication. Am J Obstet Gynecol. 1994;170:495–504. doi: 10.1016/s0002-9378(94)70217-9. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal A, Gupta HP, Anand S, Das K. Vaginal birth after cesarean - A partographic analysis. J Obst Gyn India. 2002;52:85–9. [Google Scholar]
- 8.Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW, et al. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351:2581–9. doi: 10.1056/NEJMoa040405. [DOI] [PubMed] [Google Scholar]
- 9.Smith GC, Pell JP, Cameron AD, Dobbie R. Risk of perinatal death associated with labor after previous cesarean delivery in uncomplicated term pregnancies. JAMA. 2002;287:2684–90. doi: 10.1001/jama.287.20.2684. [DOI] [PubMed] [Google Scholar]
- 10.Locatelli A, Regalia AL, Ghidini A, Ciriello E, Biffi A, Pezzullo JC. Risks of induction of labour in women with a uterine scar from previous low transverse caesarean section. BJOG. 2004;111:1394–9. doi: 10.1111/j.1471-0528.2004.00287.x. [DOI] [PubMed] [Google Scholar]
- 11.Mozurkewich EL, Hutton EK. Elective repeat cesarean delivery versus trial of labor: A meta-analysis of the literature from 1989 to 1999. Am J Obstet Gynecol. 2000;183:1187–97. doi: 10.1067/mob.2000.108890. [DOI] [PubMed] [Google Scholar]
- 12.McMahon MJ, Luther ER, Bowes WA, Jr, Olshan AF. Comparison of a trial of labor with an elective second cesarean section. N Engl J Med. 1996;335:689–95. doi: 10.1056/NEJM199609053351001. [DOI] [PubMed] [Google Scholar]
- 13.Rossi AC, D’Addario V. Maternal morbidity following a trial of labor after cesarean section vs elective repeat cesarean delivery: A systematic review with metaanalysis. Am J Obstet Gynecol. 2008;199:224–31. doi: 10.1016/j.ajog.2008.04.025. [DOI] [PubMed] [Google Scholar]


