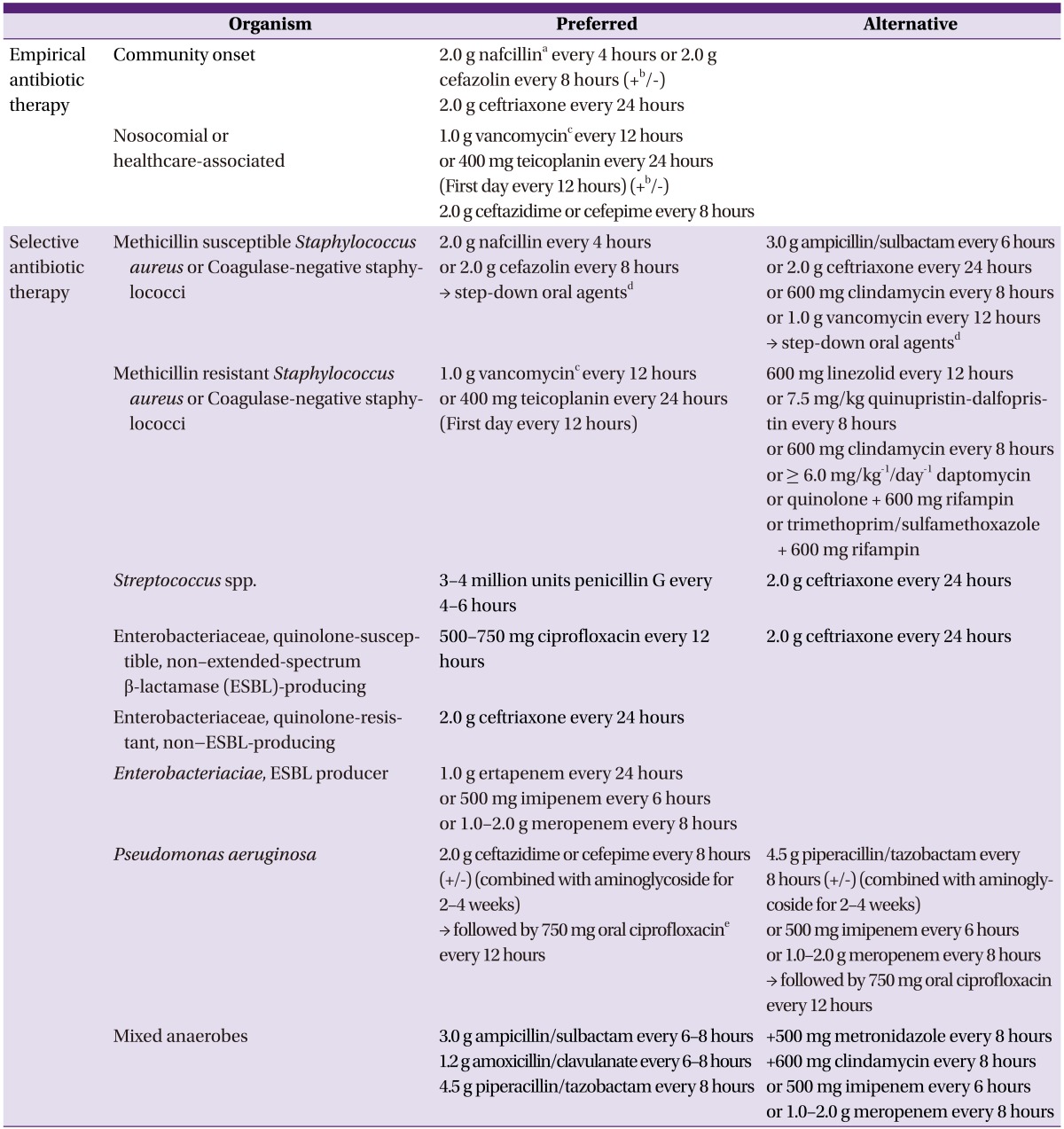
Table 6.
Suggested regimens for antimicrobial therapy of osteomyelitis
aIn patients with delayed hypersensitivity to nafcillin, cefazolin can be used. In patients with immediate hypersensitivity, penicillins should be replaced by vancomycin or clindamycin. S. aureus isolates that are clindamycin-susceptible but erythromycin-resistant should be tested for inducible clindamycin resistance using the D-test.
bCombination therapy can be considered before the causative organism is identified in some conditions, i.e., preceding bacteremia when associated with urinary tract infection or intra-abdominal infection, or in the immunocompromised or elderly.
cThe trough concentration of vancomycin should be 15-20 µg/mL.
dCombination therapy with drugs to which the organism is susceptible should be used for the treatment of osteomyelitis caused by S. aureus. 500-750 mg ciprofloxacin every 12 houres + 600 mg rifampin every 24 houres/750 mg levofloxacin + 600 mg rifampin every 24 houres/trimethoprim/sulfamethoxazole 80/400 mg single strength, 2 tablets every 12 houres + 600 mg rifampin every 24 houres.
eQuinolone monotherapy is no longer considered adequate because of the high risk for the emergence of resistance during the high bacterial burden that exists in the initial stages of the disease; however, it can be used as an oral step down therapy after initial combination therapy with β-lactam agent and aminoglycoside.