Abstract
Study Objective
We sought to determine if patients living in areas affected by emergency department (ED) closure, with subsequent increased distance to the nearest ED, had a higher risk of inpatient death from time-sensitive conditions.
Methods
Using the California Office of Statewide Health and Planning Development (OSHPD) database, we performed a non-concurrent cohort study of hospital admissions in California between 1999-2009 for patients admitted for acute myocardial infarction (AMI), stroke, sepsis and asthma/chronic obstructive pulmonary disease (COPD). We used generalized linear mixed effects models comparing adjusted inpatient mortality for patients experiencing increased distance to the nearest ED versus no change in distance.
Results
Of 785,385 patient admissions, 67,577 (8.6%) experienced an increase in distance to ED care due to an ED closure. The median change for patients experiencing an increase in distance to the nearest ED was only 0.8 miles with a range of 0.1 to 33.4 miles. Patients with an increase did not have a significantly higher mortality (adjusted odds ratio 1.04, 95% CI 0.99, 1.09). In subgroups, we also noted no statistically significant differences in adjusted mortality among patients with AMI, stroke, asthma/COPD, and sepsis. We did not observe any significant variations in mortality for time-sensitive conditions in sensitivity analyses that incorporated a lag effect of time after change in distance, allowance for a larger affected population, or removal of ST-elevation myocardial infarction (STEMI) from the AMI subgroup.
Conclusions
In this large population-based sample, less than 10% of the patients experienced an increase in distance to the nearest ED, and of that group, the majority had less than a one-mile increase. These small increased distances to the nearest ED were not associated with higher inpatient mortality among time-sensitive conditions.
Introduction
Background
In 2006, the Institute of Medicine reported that “the emergency care system of the future should be highly regionalized, coordinated, and accountable.”1 While purposeful and nationwide regionalization has yet to materialize into health policy,2 current changes in ED distribution provide an opportunity to study the natural experiment of ED closures and the subsequent effects on patients to inform regionalization initiatives or other health policies aiming to restructure healthcare delivery systems.3
Over the last two decades, the annual number of ED visits nationwide increased from 94.9 million to 116.8 million (23%) amidst a concurrent decrease in the number of EDs from 4,114 to 3,925 (4.6%).4 The trend in California is even more striking, where there has been a 12% reduction in available EDs and a 27% increase in total patient visits per ED.5-9 Increased ED demand in a setting of progressive ED closures – which disproportionately occur in underserved areas10 – has stirred significant public and media concern.11
Importance
ED closure is important because it may increase the distance and time it takes for patients to access critical medical care. Increased geographic distance affects people’s willingness to seek care.12,13 One study of hospital closure in Los Angeles demonstrated that even a one-mile increase in hospital proximity is associated with a 6.5% increase in the death rate from AMI and an 11-20% increase from unintentional injuries.14 However, this study was done with aggregated outcomes rather than patient-level outcomes. Another study in Los Angeles found that hospital closure caused a transient increase in crowding and ambulance diversions for surrounding EDs,15 which have both been related to adverse patient outcomes.16,17
Goals of This Investigation
There is limited literature evaluating the impact of ED closure on clinically relevant patient health outcomes, and little known about the extent to which people are affected by closures. Defining such effects may provide policy makers with a clearer picture of the impact of closure as they propose changes in acute care systems, especially given the federal emphasis on regionalization.1 In this study, we sought to first quantify the proportion of patients who, over an eleven-year period, experienced an increase in distance to their nearest ED and the extent to which they were affected. Our main goal was to determine if patients who experienced increases in distance to their nearest ED suffered increased inpatient mortality. Specifically, we hypothesized that these increases in distance would be associated with poorer outcomes for four time-sensitive medical conditions: acute myocardial infarction (AMI), stroke, sepsis, and asthma/chronic obstructive pulmonary disease (COPD). We sought to evaluate whether patients with these pre-specified time-sensitive conditions had a higher risk of in-patient mortality when evaluated as an overall cohort together as well as separately in analyses stratified by condition.
Methods
Study design and setting
Using data from non-federal hospitals in California, we performed a non-concurrent cohort study of all admissions for conditions that have been previously identified as time-sensitive:18-22 AMI, stroke, sepsis and asthma/COPD, based on the Clinical Classifications Software from the Agency for Healthcare Quality and Research.23
Data Sources
We used non-public patient-level data for admitted adult patients from January 1, 1999 to December 31, 2009 from the California Office of Statewide Health and Planning Development (OSHPD) Patient Discharge Data (PDD), including age, gender, race/ethnicity, insurance, visit date, source of admission, ICD-9 codes of primary and secondary diagnoses, and hospital disposition (including in-hospital death). We did not analyze patients who were discharged from the ED and were not admitted.
We also obtained utilization data from the state to document which hospitals had ED closures by year from 1999-2009 and merged corresponding annual hospital-level characteristics from the hospital financial and utilization reports.24 Discrepancies or missing data were confirmed directly, as described previously.25 We also obtained case-mix of each hospital to adjust for case severity.
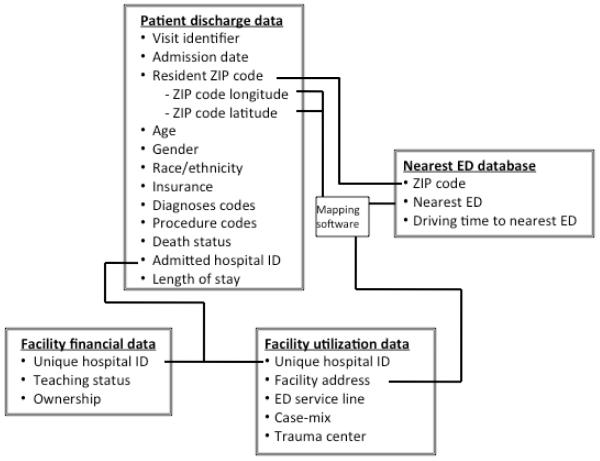
We identified the longitude and latitude coordinates of each patient zip code using Mailer’s software.26 Figure 1 and Appendix Figure A1 demonstrate our dataset linkage and patient selection flowchart, respectively. This study was approved by the University of California San Francisco Committee on Human Research.
Figure 1.
Schematic of data linkage
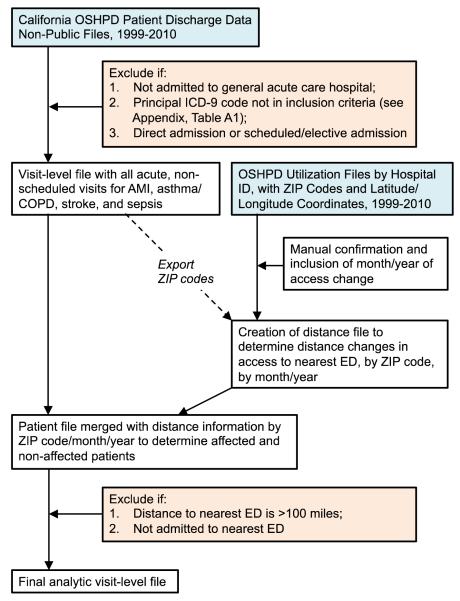
Appendix Figure A1.
Patient selection flowchart
Selection of participants
To determine the patients affected by ED closures, we geocoded the location of each patient’s home zip code to the nearest ED and calculated the straight-line distance between the population centroid of the two zip codes for each year.27 We then calculated the change in distance between adjacent years for each zip code. This allowed us to stratify patients into those who experienced an increase in distance to the nearest ED and those who did not.
To capture the patient population more precisely, we limited the study to include only patients who were admitted from the ED by excluding direct or elective admissions from the community since they bypass the ED (and therefore would not be affected by ED closure). Additionally, we included only those patients who actually were admitted to their nearest hospital rather than analyzing a more theoretical cohort of patients who potentially could have experienced change based on geocoding of zip code calculations alone. This allowed us to exclude patient preferences for certain EDs. For example, patients with a specific health plan (e.g., Kaiser, Veterans Administration) may prefer going to their designated hospital even if it is not the closest ED. We did not completely exclude all patients from these health plans, however, since our model still captured such patients if the preferred destination was the closest or overridden (e.g., deemed unsafe due to critical condition) by pre-hospital providers. We also excluded patients whose mailing zip codes were more than 100 miles away from their admitted hospital as done in other literature,28 since they were likely admitted to hospitals while away from home (e.g., vacation) or not residing at the location they provided to the hospital.
The treatment group included all patients living in zip codes that experienced an increase in driving distance to their nearest ED in the year they visited the ED, compared to the base year 1999. The control group consisted of all patients living in zip codes that did not experience an increase in driving distance in the year they visited the ED, compared to the base year 1999.
Outcome Variables
The primary outcome variable in our model is composite inpatient mortality for all of the time-sensitive conditions studied. The secondary outcomes are the inpatient mortality for each individual condition studied. The mortality outcomes were obtained from the patient-level files.
Predictor Variables
We adjusted for age, race/ethnicity, sex, and insurance status (Medicare, Medicaid, Private, Indigent, and Other). We also controlled for standard Elixhauser comorbidities29 to adjust for differences in baseline mortality risks as well as case-mix of each hospital to control for hospital-level differences in patient acuity.
Statistical analysis
We applied a generalized linear mixed effects model framework to estimate a patient’s likelihood for inpatient mortality as a function of the distance to their nearest ED. We performed hierarchical modelling to account for patient-level effects and hospital-level clustering. We analyzed the general cohort of patients with all four time-sensitive conditions, and also performed stratified analyses to determine if there were isolated effects in any of the specific conditions. We specified two models a priori of the relationship between difference in distance and mortality: Model 1, which compared mortality if a patient had no change or a decrease in distance compared to an increase in distance, and Model 2, which compared inpatient mortality among those experiencing a decrease, no change, and increase in distance.
Since mortality could potentially change over time due to, for example, the development of new treatments, we also added year as a linear variable to control for secular trends. Additionally, because closures are usually implemented gradually, allowing for community awareness and change in ED-seeking behavior, we incorporated a lag effect for the year the ED closed. Patients were categorized as unaffected if admitted in the first half of the year of closure, and affected if hospitalized in the latter half. All analyses were performed with SAS 9.2 (Cary, NC).
Results
Characteristics of patients who experienced change in ED distance due to closure
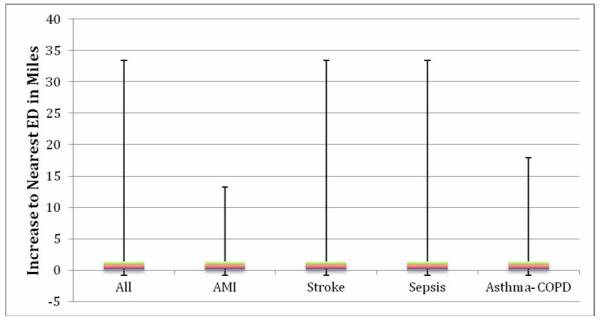
We studied a total of 785,385 patients during this period (Table 1), of which 67,577 (8.6%) individuals experienced an increase in distance to their nearest ED. The increase in distance experienced by patients ranged from as little as 0.1 to as great as 33.4 miles, with a median of 0.8 miles. As shown in Table 2, the medians were identical when analyzed by disease condition. Patients experiencing a decrease had a greater distance change than those experiencing an increase; overall, patients who had a decrease in distance to the nearest ED were, on average, 13.8 miles closer than before, with a median of 6.6 miles and a range of 0.1 to 77.7 miles.
Table 1.
Characteristics of study patients based on whether or not they experienced an increase in distance to the nearest ED (n=785,385)
| Change in Driving Distance | Decrease and no change (%) |
Increase (%) |
|---|---|---|
| Number of patients* | 717,808 (91.4) | 67,577 (8.6) |
|
| ||
| Subgroup conditions* | ||
| AMI | 149273 (92.0) | 12979 (8.0) |
| Stroke | 174989 (91.6) | 16116 (8.4) |
| Sepsis | 178209 (90.3) | 19148 (9.7) |
| Asthma-COPD | 215337 (91.8) | 19334 (8.2) |
|
| ||
| Gender | ||
| Male | 329912 (46.0) | 31011 (45.9) |
| Female | 387881 (54.0) | 36565 (54.1) |
| Unknown | 15 (0.0) | 1 (0.0) |
|
| ||
| Age category | ||
| 18-44 years | 52489 (7.3) | 5410 (8.0) |
| 45-64 years | 182758 (25.5) | 19231 (28.5) |
| 65-74 years | 149845 (20.9) | 13848 (20.5) |
| 75-84 years | 201438 (28.1) | 17533 (26.0) |
| ≥ 85 years | 131278 (18.3) | 11555 (17.1) |
|
| ||
| Race/Ethnicity | ||
| Non-hispanic White | 477645 (66.5) | 40033 (59.2) |
| Non-hispanic Black | 54105 (7.5) | 9553 (14.1) |
| Hispanic | 109163 (15.2) | 11949 (17.7) |
| Other (Asian, Pacific Islander, Native American) |
64530 (9.0) | 5330 (7.9) |
| Unknown | 12365 (1.7) | 712 (1.1) |
|
| ||
| Insurance | ||
| Medicare | 468755 (65.3) | 42907 (63.5) |
| Medi-Cal (Medicaid) | 90400 (12.6) | 10009 (14.8) |
| Private | 115881 (16.1) | 10179 (15.1) |
| Uninsured/self-pay | 33653 (4.7) | 3777 (5.6) |
| Other | 8914 (1.2%) | 697 (1.0) |
| Unknown | 205 (0.0) | 8 (0.0) |
|
| ||
| Elixhauser comorbidities† | ||
| Hypertension | 418781 (58.3) | 42508 (62.9) |
| Diabetes | 169252 (23.6) | 17382 (25.7) |
| Fluid & electrolyte disorder | 203746 (28.4) | 21393 (31.7) |
|
| ||
| Mortality | 75075 (10.5) | 7459 (11.0) |
|
| ||
| Case mix index mean (SD) | 1.12 (0.19) | 1.19 (0.18) |
These are row percentages; remainder of table shows column percentages.
Only most common three Elixhauser comorbidities listed
Table 2.
Distance changes experienced by patients, 1999-2009, overall and stratified by disease condition
| Median (IQR) [range] distance change (miles) |
|
|---|---|
| All | |
| Decrease | −6.6 (−20.2, −0.5) [−77.7, −0.1] |
| Increase | 0.8 (0.2, 1.4) [0.1, 33.4] |
|
| |
| AMI | |
| Decrease | −0.8 (−11.6, −0.3) [−77.7, −0.1] |
| Increase | 0.8 (0.2, 1.4) [0.1, 13.2] |
|
| |
| Stroke | |
| Decrease | −6.7 (−20.2, −0.7) [−77.7, −0.1] |
| Increase | 0.8 (0.2, 1.4) [0.1, 33.4] |
|
| |
| Sepsis | |
| Decrease | −1.8 (−20.2, −0.5) [−77.7, −0.1] |
| Increase | 0.8 (0.2, 1.4) [0.1, 33.4] |
|
| |
| Asthma-COPD | |
| Decrease | −7.6 (−20.2, −0.7) [−77.7, −0.1] |
| Increase | 0.8 (0.2, 1.4) [0.1, 17.9] |
All patients experiencing “no change” were zero
Patients who faced increased distances to the nearest ED were more likely to be black or Hispanic, more likely to be uninsured or be insured by Medicaid, and less likely to be privately insured. They were more likely to suffer from hypertension, diabetes, fluid and electrolyte disorders, renal failure, and mental health disease.
Main analyses of entire cohort: Adjusted outcomes of all patients in sample
The adjusted mortality of the entire cohort of patients experiencing an increased distance to the nearest ED was not significantly higher than those who did not (adjusted OR 1.04, 95% CI 0.99, 1.09). (Table 3)
Table 3.
Multivariate model comparing in-hospital mortality of patients experiencing an increased distance to their nearest ED compared with those having no increase in distance
| Patients experiencing increased distance to nearest ED (n=785,385) |
||
|---|---|---|
|
| ||
| Sample size | Odds Ratio (95% CI) |
|
|
| ||
| All time sensitive conditions | ||
| Decrease/no change in distance to nearest ED | 717,808 (92.0%) | ref |
| Increase in distance to nearest ED | 67,577 (8.6%) | 1.04 (0.99, 1.09) |
|
| ||
| AMI (n=162,252) | ||
| Decrease/no change in distance to nearest ED | 149,273 (92.0%) | ref |
| Increase in distance to nearest ED | 12,979 (8.0%) | 1.09 (0.94, 1.25) |
| Stroke (n=191,105) | ||
| Decrease/no change in distance to nearest ED | 174,989 (91.6%) | ref |
| Increase in distance to nearest ED | 16,116 (8.4%) | 1.02 (0.95, 1.10) |
| Sepsis (n=197,357) | ||
| Decrease/no change in distance to nearest ED | 178,209 (90.3%) | ref |
| Increase in distance to nearest ED | 19,148 (9.7%) | 1.04 (0.97, 1.11) |
| Asthma/COPD (n=234,671) | ||
| Decrease/no change in distance to nearest ED | 215,337 (91.8%) | ref |
| Increase in distance to nearest ED | 19,334 (8.2%) | 1.08 (0.94, 1.24) |
models adjusted for age, race/ethnicity, gender, insurance, case-mix index, and Elixhauser comorbidities (congestive heart failure, paralysis, neurological disorders, chronic lung disease, diabetes, renal failure, liver disease, metastatic cancer, solid tumor, coagulopathy, obesity, weight loss, fluid & electrolyte disorders, chronic blood loss anemia, deficiency anemia, peripheral vascular disease, alcohol abuse, and depression), year, and zip code level clustering
Given that patients experiencing a decrease in distance had a much greater change in distance than those experiencing an increase, we wanted to test if the potential benefit of experiencing a decrease in distance was diluting the effect of patient experiencing an increase in distance. As shown in the lower panel of Table 4, we performed the adjusted analysis in the three subgroups of patients (those experiencing a decrease in distance, no change in distance, and an increase in distance) also showed no significant difference in those with an increased distance (OR 1.04, 95% CI 0.99, 1.09). Those with a decrease in distance similarly did not experience a benefit as defined by a decrease in the adjusted risk of inpatient mortality (OR 1.01, 95% CI 0.92, 1.12).
Table 4.
Multivariate model comparing in-hospital mortality of patients experiencing a decrease, no change, and increase in distance to their nearest ED
| Patients experiencing increased and decreased change to nearest ED (n=785,385) |
||
|---|---|---|
|
| ||
| Sample size | Odds Ratio (95% CI) |
|
|
| ||
| All time sensitive conditions: | ||
| Decrease in distance to nearest ED | 23,981 (3.1%) | 1.01 (0.92, 1.12) |
| No change in distance to nearest ED | 693,827 (88.3%) | ref |
| Increase in distance to nearest ED | 67,577 (8.6%) | 1.04 (0.99, 1.09) |
|
| ||
| AMI | ||
| Decrease in distance to nearest ED | 4,580 (2.8%) | 1.09 (0.94, 1.25) |
| No change in distance to nearest ED | 144,693 (89.2%) | ref |
| Increase in distance to nearest ED | 12,979 (8.0%) | 1.04 (0.96, 1.13) |
| Stroke | ||
| Decrease in distance to nearest ED | 5,710 (3.0%) | 1.15 (1.00, 1.31) |
| No change in distance to nearest ED | 169,279 (88.6%) | ref |
| Increase in distance to nearest ED | 16,116 (8.4%) | 1.03 (0.96, 1.10) |
| Sepsis | ||
| Decrease in distance to nearest ED | 5,442 (2.8%) | 1.07 (0.94, 1.21) |
| No change in distance to nearest ED | 172,767 (87.5%) | ref |
| Increase in distance to nearest ED | 19,148 (9.7%) | 1.04 (0.97, 1.11) |
| Asthma/COPD | ||
| Decrease in distance to nearest ED | 8,249 (3.5%) | 1.02 (0.80, 1.29) |
| No change in distance to nearest ED | 207,088 (88.3%) | ref |
| Increase in distance to nearest ED | 19,334 (8.2%) | 1.08 (0.94, 1.24) |
models adjusted for age, race/ethnicity, gender, insurance, case-mix index, and Elixhauser comorbidities (congestive heart failure, paralysis, neurological disorders, chronic lung disease, diabetes, renal failure, liver disease, metastatic cancer, solid tumor, coagulopathy, obesity, weight loss, fluid & electrolyte disorders, chronic blood loss anemia, deficiency anemia, peripheral vascular disease, alcohol abuse, and depression), year, and zip code level clustering
Stratified analyses: Adjusted outcomes of patients with AMI, stroke, sepsis, and asthma/COPD
We present our stratified results from Model 1 comparing mortality of patients in all subgroups who experienced an increase in distance compared with those who did not experience a change or had a decrease (Table 3). Of 162,252 patients with AMI, 8.0% (n=12,979) experienced a closure and subsequent increase in distance to the nearest ED, compared with 92.0% (n=149,273) who did not. There was no statistically significant difference in inpatient mortality when comparing these two groups (OR 1.09, 95% CI 0.94, 1.25). Of 191,105 stroke patients, 8.4% (n=16,116) faced an increase in distance, compared with 91.6% (n=174,989) who did not. Again, there was no difference in inpatient mortality (OR 1.02, 95% CI 0.95, 1.10) between these groups. When analyzing the 197,357 sepsis patients, 9.7% (n=19,148) experienced an increase in distance, and again there was no statistically increased odds (OR 1.04, 95% CI 0.97, 1.11) of inpatient mortality compared with the 90.3% (n=178,209) who did not. For the 234,671 asthma/COPD patients, those experiencing an increase in distance to the nearest ED (8.2%, n=19,334) similarly had no significant odds of inpatient mortality (OR 1.08, 95% CI 0.94, 1.24) of inpatient death compared with the referent group (91.8% n=215,337).
The lower panel of model 2 shows the results of a three-category analysis, when patients experiencing an increase in distance and decrease in distance were separately compared with the referent group of those with no change (Table 4). For AMI patients, a very small group of patients experienced a decrease in driving distance to the nearest ED (2.8%, n=4,580), compared with the no change group (89.2%, n=144,693), and the increase group (8.0%, n=12,979). No significant differences in in-hospital mortality were found when comparing these groups. These results were similar again for all patients experiencing an increase in distance to the nearest ED with the other three conditions.
Patients with stroke experiencing a decrease in distance to the nearest ED just met the criteria for 95% statistical significance. For these patients, 3.0% (n=5,710) of patients had a decrease in distance to the nearest ED, with a barely perceptible increase in inpatient mortality (OR 1.15, 95% CI 1.00, 1.31) compared with the referent group of no change (88.6%, n=169,279).
Sensitivity analyses
We performed numerous sensitivity analyses to investigate if certain assumptions would result in different findings, specifically regarding: 1) lag time related to potential differential effects depending on when changes in distance occurred; 2) the inclusion criteria for patients who were assumed to be affected by changes in distance; and 3) the assumption that all AMI patients experienced similar effects from distance changes, especially those with STEMI.
First, to test for the idea that EDs and hospitals likely recover from nearby closures, adjusting staffing and resources to meet increased demand, we carried out subset analyses including only patients who experienced change within two years of closure. These analyses were not different from our main results.
Second, our main model excludes patients who were not admitted at their nearest ED, which allows for the most conservative estimate of the effect on mortality. We performed an additional sensitivity analysis that includes all of these potential patients living in a zip code that experienced an increase to the nearest ED. These results showed no change from our main model. The results for the stratified analyses for the remaining conditions remained insignificant.
Finally, there is a real possibility that patients with STEMI could have been re-routed (and therefore travelled longer distances) intentionally due to regionalization networks that, in California, began first in 2003 (Marin County) and subsequently in several counties in Southern California, including Los Angeles, San Diego, Ventura, and Orange counties. While inception of a formalized network did not always mean that the infrastructure was fully established to implement direct transport to the nearest hospital with cardiac catheterization capability (e.g., not all ambulances had trained paramedics, or even electrocardiogram machines on board), it is possible that these patients could have benefited from being transported farther distances if they received a higher level of care. Therefore, we removed patients with STEMI from our AMI group and re-analyzed our results in the overall cohort modelled with all conditions, as well as stratified by disease condition. We found no difference in our results.
Limitations
Our study has several notable limitations. First, our primary outcome was in-hospital mortality which, while having strong face validity, remains a crude indicator of adverse outcomes related to delays in emergency care, relative to endpoints such as survival to longer time periods or clinical outcome measures such as angina, ejection fraction, or functional status. It is possible that small changes in distance and time might be more likely to affect morbidity than mortality, but this effect remains unmeasured by our study. In addition, compared to other more frequent clinical outcomes, mortality may have lower statistical power. Having said this, and even though death remained a rare event, the number of deaths in our cohort was quite large.
Second, our data does not contain information regarding the proportion of our cohort that arrived by ambulance, or whether they could have received intervention prior to arrival. It is possible that there are systematic differences in method of transport between groups who experienced an increase in distance compared with the control group, or even at baseline, since people living further from an ED could be more likely to activate EMS than others. However, the literature suggests that greater distance from EDs in some areas (notably rural areas) have a lower likelihood of EMS utilization.30,31 Even if patients with increased distance to an ED were more likely to use EMS, it would only affect the results if such patients were more ill or had more co-morbidities. Given the lack of information in this area, it is unclear if this would positively or negatively bias our results, yet remains a potential limitation. Similarly, it is possible that patients most affected by ED closure die before they reach the ED. Such patients would not be included in our study, and this immortal time bias could therefore attenuate our results.
Third, our data for increases in driving time is very skewed, with the majority of patients experiencing less than a 10-minute increase. Detecting mortality differences if patients do not experience a significant increase could be limited. Additionally, any significant measurement error in the geocoding of distances could attenuate the effect. We do not believe there are systematic biases in our measurement of driving time for communities experiencing increases in driving time; however, theoretically, if shorter increases in distance are underestimated when calculating driving times, compared with longer increases in distance, our findings would be conservative and therefore not show an effect.
Fourth, while we measured increased distance to the nearest ED, factors such as ED overcrowding, waiting times, diversion or even traffic patterns and road construction could alter driving distances or time to ED care. Moreover, changes over time in the care of each of the conditions studied (e.g., the sepsis campaign, etc.) are likely not addressed equally at each hospital in the same time frame, but adoption of such changes are nearly impossible to measure across all hospitals for all our conditions and is a limitation of the study. While our model did cluster on the hospital to account for some intra-hospital differences, systematic differences – such as overall early adoption of aggressive treatments to decrease mortality for the time-sensitive conditions we studied – in hospitals where patients experienced no change in their distance to the nearest ED compared with hospitals where patients did experience an increased distance could contribute to our negative findings.
Fifth, while our retrospective cohort approach has advantages for this type of analysis and our use of ICD-9 codes is a common approach in healthcare research, we had limited control over the accuracy of the data and variation in coding of conditions. We cannot completely exclude the possibility of unknown but important population differences between the treatment and control groups. However, as noted in our prior work, the OSHPD database is very detailed with high response rates, and we do not expect bias in the results as long as the errors do not systematically differ by the characteristics examined.25
Finally, our findings are limited to the context of California, which is somewhat more urban than the nation, producing more closures of EDs in areas with concentrated populations. As a result, our findings may not apply to different settings, such as rural areas with lesser concentration of healthcare resources.
Discussion
In this study of California ED’s, closures that produced longer distances to emergency care were not associated with higher odds for inpatient mortality across a range of time-sensitive conditions. Our results are contrary to our initial hypothesis that mortality would worsen when the distance to emergency care increases. Despite strong evidence for early treatment of many acute conditions, these findings raise several interesting possible explanations.
First, only a small percentage – less than 2% – of patients experienced an increase in distance. Of those that did, the increases in distance were minimal, with a mean of 1.4 miles or median of 0.8 miles. While rural closures have occurred in California, the majority of ED closures have been in urban areas with other existing services that could mitigate potential negative consequences of closures. Studying closures in other settings, particularly more rural settings, could provide an important contribution to the literature regarding whether closures in different contexts have differential effects.
Second, because we studied time-dependent conditions, time waiting to be seen by a clinician would potentially be less affected than less urgent conditions. In most EDs, ambulance transports are triaged before walk-in patients. Therefore the minimal increase in travel time incurred by an increase in distance could have been negligible for patients with these time-sensitive conditions who would be triaged first. It is very possible that a similar analysis in patients with non-time-sensitive conditions could have different findings.
On the other hand, it is also possible that time waiting to be seen, which are generally longer than transport times, could overwhelm any increases in distance to the nearest ED. Transport times would especially be shorter for patients who activate EMS. As mentioned in the limitations, our data do not contain information regarding method of transport to the ED. The literature states that approximately 50% of AMI patients arrive to the ED by self-transport,32 despite the benefits of emergency medical services (EMS) activation.33 Similarly, patients with stroke often delay seeking care or activating EMS because they doubt the seriousness of symptoms.34 In urban areas, even without EMS activation, however, transport times are generally shorter than the waiting time to see a physician, which could partially explain a negative effect of increased distance on outcome.
Third, it is possible that ED closure may take place because the ED is underperforming in terms of volume or quality of care provided. For example, hospitals that close are more likely to be small (< 100 beds), less efficient, financially distressed, operate at excess capacity, and offer fewer specialty services – all of which may negatively affect patient care.14,35-39 Similarly, EDs that close have fewer monthly ambulance transports, ED treatment stations, and annual ED visits.9,15 Since greater volume often results in better outcomes 40,41, closures may disproportionately occur in underperforming EDs. As a result, mortality may not be increased because while patients must travel farther to their nearest hospital, they may be benefiting from improved quality of care. This, too, would be a vital area of inquiry and may be condition-specific. For example, after a well-publicized closure of the Martin Luther King-Drew trauma center that had been faulted for providing poor quality care to patients, trauma patients who were diverted to a nearby hospital did not experience an increase in mortality.42
An important point regarding our findings relates to our ability to interpret a non-statistically significant result as essentially no effect. Given that the confidence intervals of the adjusted odds ratios in our combined and stratified cohorts were all very narrow – e.g., for our main model, the 95% CI was 0.99 to 1.10 (Table 3) – this limits the size of possible difference to be quite small. On the other end, the 95% CI for the >5 mile increase for the asthma/COPD patients is 0.62 to 1.61 (Table 5), so this allows for effect sizes in the more important range.
Table 5.
Multivariate model comparing in-hospital mortality of patients experiencing stepwise increasing distances to their nearest ED compared with those having no change or decrease
| Patients experiencing increased and decreased change to nearest ED (n=785,385) |
||
|---|---|---|
|
| ||
| Sample size | Odds Ratio (95% CI) |
|
|
| ||
| All time sensitive conditions | ||
| Decrease/no change | 717808 (91.4%) | Ref |
| Increase of <2 miles | 55846 (7.1%) | 1.04 (0.99, 1.10) |
| Increase of 2-5 miles | 7469 (1.0%) | 1.03 (0.91, 1.16) |
| Increase of >5 miles | 4262 (0.5%) | 1.09 (0.95, 1.26) |
|
| ||
| AMI | ||
| Decrease/no change | 149273 (92.0%) | Ref |
| Increase of <2 miles | 10538 (6.5%) | 1.06 (0.97, 1.15) |
| Increase of 2-5 miles | 1503 (0.9%) | 0.94 (0.71, 1.25) |
| Increase of>5 miles | 938 (0.6%) | 1.01 (0.82, 1.24) |
| Stroke | ||
| Decrease/no change | 174989 (91.6%) | Ref |
| Increase of <2 miles | 13370 (7.0%) | 1.00 (0.93, 1.09) |
| Increase of 2-5 miles | 1752 (0.9%) | 1.03 (0.86, 1.25) |
| Increase of>5 miles | 994 (0.5%) | 1.22 (1.02, 1.47) |
| Sepsis | ||
| Decrease/no change | 178209 (90.3%) | Ref |
| Increase of <2 miles | 16320 (8.3%) | 1.05 (0.97, 1.13) |
| Increase of 2-5 miles | 1802 (0.9%) | 0.98 (0.82, 1.17) |
| Increase of>5 miles | 1026 (0.5%) | 0.93 (0.78, 1.11) |
| Asthma/COPD | ||
| Decrease/no change | 215337 (91.8%) | Ref |
| Increase of <2 miles | 15618 (6.7%) | 1.09 (0.94, 1.26) |
| Increase of 2-5 miles | 2412 (1.0%) | 1.04 (0.62, 1.72) |
| Increase of>5 miles | 1304 (0.6%) | 1.00 (0.62, 1.61) |
models adjusted for age, race/ethnicity, gender, insurance, case-mix index, and Elixhauser comorbidities (congestive heart failure, paralysis, neurological disorders, chronic lung disease, diabetes, renal failure, liver disease, metastatic cancer, solid tumor, coagulopathy, obesity, weight loss, fluid & electrolyte disorders, chronic blood loss anemia, deficiency anemia, peripheral vascular disease, alcohol abuse, and depression), year, and zip code level clustering
These findings are crucial in the current discussion of regionalization of healthcare services, particularly emergency care. They suggest that in certain context where other services may exist, it is possible that closures do not have a detrimental effect on patient outcomes, at least when measured by in-hospital mortality.
Our study contributes to the understanding of ED closures within a particular context, that should be interpreted in light of what is known regarding hospital consolidations or closures.43 In certain scenarios, hospital closures have the potential to provide cost savings and improve efficiency of remaining hospitals.35,44,45 Patients may utilize outpatient resources more effectively after hospital downsizing or closure.46 Alternatively, consolidations or mergers of hospitals that reduce one ED might provide other services that decrease overall mortality in the hospital.47 For instance, investment in resources such as a 24-hour catheterization lab or a fully staffed ICU may lead to no change in mortality, negating the effects of ED closure. Finally, regionalization of services resulting from hospital closure may increase the specialty or disease-specific volume of care at another facility, which may improve outcomes of certain conditions, such as AMI.45 While the exclusion of STEMI patients in our study did not result in positive results, our study did not directly evaluate the result of regionalization efforts.
Although distances only increased for a small percentage of the community, that percentage was characteristically more vulnerable, including minority groups, the uninsured or those insured by Medicaid, and those with co-morbidities. Increased distance may serve as a surrogate marker of actual difficulty in getting to an ED, and while these groups did not experience a notable difference in mortality, there is a disparity that may appear in other process-driven measures.
In summary, California residents who faced an increase in distance to the nearest ED due to ED closure did not have higher inpatient mortality from AMI, stroke, sepsis, or asthma/COPD. Our findings add important nuance to the complex decisions involved when hospital and health system administrators consider whether to close an ED. While public concern about closures’ effects on access to emergency care will likely remain a valid issue, our data suggest that closures during this time period in California resulted in only minimal increases in distance for a minority of patients and that, at least when measured by inpatient mortality, closures did not result in poorer outcomes for these patients with time-sensitive conditions.
Appendix Figure A2.
Increase of distance to nearest ED across study conditions
Acknowledgement, Funding and Disclosures
We would like to acknowledge Nicole Gordon, BA for her technical support. This publication was supported by NIH/NCRR/OD UCSF-CTSI Grant Number KL2 RR024130 (RYH), the Robert Wood Johnson Foundation Physician Faculty Scholars (RYH), and the NIH/NHLBI Grant Number K24HL098372 (ADA). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of any of the funding agencies.
Appendix.
Table A1.
ICD-9 codes used for patient conditions from the Clinical Classifications Software (AHRQ)
| AMI | 410.0, 410.00, 410.01, 410.02, 410.1, 410.10, 410.11, 410.12, 410.2, 410.20, 410.21, 410.22, 410.3, 410.30, 410.31, 410.32, 410.4, 410.40, 410.41, 410.42, 410.5, 410.50, 410.51, 410.52, 410.6, 410.60, 410.61, 410.62, 410.7, 410.70, 410.71, 410.72, 410.8, 410.80, 410.81, 410.82, 410.9, 410.90, 410.91, 410.92 |
| Stroke | 430., 431., 432.0, 432.1, 432.9, 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.0, 434.00, 434.01, 434.1, 434.10, 434.11, 434.9, 434.90, 434.91, 436. |
| Asthma/ COPD |
493.00, 493.01, 493.02, 493.10, 493.11, 493.12, 493.20, 493.21, 493.22, 493.81, 493.82, 493.90, 493.91, 493.92, 490., 491.0, 491.1, 491.2, 491.20, 491.21, 491.22, 491.8, 491.9, 492.0, 492.8, 494., 494.0, 494.1, 496. |
| Sepsis | 003.1, 020.2, 022.3, 036.2, 038.0, 038.1, 038.10, 038.11, 038.19, 038.2, 038.3, 038.40, 038.41, 038.42, 038.43, 038.44, 038.49, 038.8, 038.9, 054.5, 449., 790.7 |
Appendix Table A2.
Multivariate model comparing in-hospital mortality of patients experiencing an increased driving time to their nearest ED compared with those having a decrease or no change
| Patients experiencing increased driving distance to nearest ED (n=785,385) |
||
|---|---|---|
| Sample size | Odds Ratio (95% CI) |
|
| All time sensitive conditions | ||
| Decrease/no change | 717,808 (92.0%) | Ref |
| Increase | 67,577 (8.6%) | 1.04 (0.99, 1.09) |
| AMI (n=162,252) | ||
| Decrease/no change in driving time to nearest ED | 149,273 (92.0%) | ref |
| Increase in driving time to nearest ED | 12,979 (8.0%) | 1.09 (0.94, 1.25) |
| Stroke (n=191,105) | ||
| Decrease/no change in driving time to nearest ED | 174,989 (91.6%) | ref |
| Increase in driving time to nearest ED | 16,116 (8.4%) | 1.02 (0.95, 1.10) |
| Sepsis (n=197,357) | ||
| Decrease/no change in driving time to nearest ED | 178,209 (90.3%) | ref |
| Increase in driving time to nearest ED | 19,148 (9.7%) | 1.04 (0.97, 1.11) |
| Asthma/COPD (n=234,671) | ||
| Decrease/no change in driving time to nearest ED | 215,337 (91.8%) | ref |
| Increase in driving time to nearest ED | 19,334 (8.2%) | 1.08 (0.94, 1.24) |
models adjusted for age, race/ethnicity, gender, insurance, case-mix index, and Elixhauser comorbidities (congestive heart failure, paralysis, neurological disorders, chronic lung disease, diabetes, renal failure, liver disease, metastatic cancer, solid tumor, coagulopathy, obesity, weight loss, fluid & electrolyte disorders, chronic blood loss anemia, deficiency anemia, peripheral vascular disease, alcohol abuse, and depression), year, and zip code level clustering
Appendix Table A3.
Multivariate model comparing in-hospital mortality of patients experiencing a decrease, no change, and increase in driving time to their nearest ED
| Patients experiencing increased and decreased change to nearest ED (n=785,385) |
||
|---|---|---|
| Sample size | Odds Ratio (95% CI) |
|
| All time sensitive conditions: | ||
| Decrease | 23,981 (3.1%) | 1.01 (0.92, 1.12) |
| No change | 693,827 (88.3%) | ref |
| Increase | 67,577 (8.6%) | 1.04 (0.99, 1.09) |
| AMI | ||
| Decrease in driving time to nearest ED | 4,580 (2.8%) | 1.09 (0.94, 1.25) |
| No change in driving time to nearest ED | 144,693 (89.2%) | ref |
| Increase in driving time to nearest ED | 12,979 (8.0%) | 1.04 (0.96, 1.13) |
| Stroke | ||
| Decrease in driving time to nearest ED | 5,710 (3.0%) | 1.15 (1.00, 1.31) |
| No change in driving time to nearest ED | 169,279 (88.6%) | ref |
| Increase in driving time to nearest ED | 16,116 (8.4%) | 1.03 (0.96, 1.10) |
| Sepsis | ||
| Decrease in driving time to nearest ED | 5,442 (2.8%) | 1.07 (0.94, 1.21) |
| No change in driving time to nearest ED | 172,767 (87.5%) | ref |
| Increase in driving time to nearest ED | 19,148 (9.7%) | 1.04 (0.97, 1.11) |
| Asthma/COPD | ||
| Decrease in driving time to nearest ED | 8,249 (3.5%) | 1.02 (0.80, 1.29) |
| No change in driving time to nearest ED | 207,088 (88.3%) | ref |
| Increase in driving time to nearest ED | 19,334 (8.2%) | 1.08 (0.94, 1.24) |
models adjusted for age, race/ethnicity, gender, insurance, case-mix index, and Elixhauser comorbidities (congestive heart failure, paralysis, neurological disorders, chronic lung disease, diabetes, renal failure, liver disease, metastatic cancer, solid tumor, coagulopathy, obesity, weight loss, fluid & electrolyte disorders, chronic blood loss anemia, deficiency anemia, peripheral vascular disease, alcohol abuse, and depression), year, and zip code level clustering
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
There are no other conflicts of interest.
- Study concept and design: Hsia, McCulloch, and Auerbach
- Acquisition of data: Hsia and Maselli
- Analysis and interpretation of data: Hsia, Kanzaria, Srebotnjak, Maselli, McCulloch and Auerbach
- Drafting of the manuscript: Hsia and Kanzaria
- Critical revision of the manuscript for important intellectual content: Hsia, Kanzaria, Srebotnjak, Maselli, McCulloch and Auerbach
- Statistical analysis: Srebotnjak and Maselli
- Obtained funding: Hsia and Auerbach
- Administrative, technical, and material support: Hsia, Kanzaria, Srebotnjak, Maselli, McCulloch and Auerbach
- Study supervision: Hsia, McCulloch and Auerbach
Contributor Information
Renee Y. Hsia, Department of Emergency Medicine, University of California, San Francisco San Francisco General Hospital San Francisco, CA USA.
Hemal K. Kanzaria, Robert Wood Johnson Foundation Clinical Scholars® University of California Los Angeles Department of Medicine and Emergency Medicine Division of General Internal Medicine and Health Service Research Los Angeles, CA USA.
Tanja Srebotnjak, University of California, San Francisco San Francisco, CA USA.
Judy Maselli, Department of Medicine, Division of Hospital Medicine University of California, San Francisco San Francisco, CA USA.
Charles McCulloch, Department of Epidemiology and Biostatistics University of California, San Francisco San Francisco, CA USA.
Andrew D. Auerbach, Department of Medicine, Division of Hospital Medicine University of California, San Francisco San Francisco, CA USA.
References
- 1.Institute of Medicine The future of emergency care in the United States health system. Acad Emerg Med. 2006;13:1081–5. doi: 10.1197/j.aem.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 2.Glickman SW, Kit Delgado M, Hirshon JM, et al. Defining and measuring successful emergency care networks: a research agenda. Acad Emerg Med. 2010;17:1297–305. doi: 10.1111/j.1553-2712.2010.00930.x. [DOI] [PubMed] [Google Scholar]
- 3.Trivedi AN, Zaslavsky AM, Schneider EC, et al. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353:692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 4.Tang N, Stein J, Hsia RY, et al. Trends and characteristics of US emergency department visits, 1997-2007. JAMA. 2010;304:664–70. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lambe S, Washington DL, Fink A, et al. Trends in the use and capacity of California’s emergency departments, 1990-1999. Ann Emerg Med. 2002;39:389–96. doi: 10.1067/mem.2002.122433. [DOI] [PubMed] [Google Scholar]
- 6.Emergency Department Care in California: Who Uses It and Why? California Counts: Population Trends and Profiles. Public Policy Institute of California; [Accessed April 23, 2010]. 2008. at http://www.ppic.org/main/publication.asp?i=775. [Google Scholar]
- 7.Melnick GA, Nawathe AC, Bamezai A, et al. Emergency department capacity and access in California, 1990-2001: an economic analysis. Health Aff (Millwood) 2004:W4-136–42. doi: 10.1377/hlthaff.w4.136. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 8.California’s Emergency Departments: System Capacity and Demand. California Healthcare Foundation; USC Center for Health Financing, Policy, and Management; [Accessed 8/3/2010]. 2002. at http://www.chcf.org/publications/2002/04/californias-emergency-departments-system-capacity-and-demand. [Google Scholar]
- 9.Is California’s Hospital-Based ED System Eroding? California Healthcare Foundation; USC Center for Health Financing, Policy, and Management; [Accessed 8/3/2010]. 2009. at http://www.chcf.org/publications/2009/07/is-californias-hospitalbased-ed-system-eroding. [Google Scholar]
- 10.Shen YC, Hsia RY. Changes in emergency department access between 2001 and 2005 among general and vulnerable populations. Am J Public Health. 2010;100:1462–9. doi: 10.2105/AJPH.2009.175828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scheck A. Emergency Medicine News. 2003. Is There Really a Crisis in California? EDs Close, Beds Increase, and the Problems Remain; p. 10. [Google Scholar]
- 12.Ludwick A, Fu R, Warden C, et al. Distances to emergency department and to primary care provider’s office affect emergency department use in children. Acad Emerg Med. 2009;16:411–7. doi: 10.1111/j.1553-2712.2009.00395.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee JE, Sung JH, Ward WB, et al. Utilization of the emergency room: impact of geographic distance. Geospat Health. 2007;1:243–53. doi: 10.4081/gh.2007.272. [DOI] [PubMed] [Google Scholar]
- 14.Buchmueller TC, Jacobson M, Wold C. How far to the hospital? The effect of hospital closures on access to care. J Health Econ. 2006;25:740–61. doi: 10.1016/j.jhealeco.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Sun BC, Mohanty SA, Weiss R, et al. Effects of hospital closures and hospital characteristics on emergency department ambulance diversion, Los Angeles County, 1998 to 2004. Ann Emerg Med. 2006;47:309–16. doi: 10.1016/j.annemergmed.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Schull MJ, Vermeulen M, Slaughter G, et al. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44:577–85. doi: 10.1016/j.annemergmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Shen YC, Hsia RY. Association between ambulance diversion and survival among patients with acute myocardial infarction. JAMA. 2011;305:2440–7. doi: 10.1001/jama.2011.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carr BG, Branas CC, Metlay JP, et al. Access to emergency care in the United States. Ann Emerg Med. 2009;54:261–9. doi: 10.1016/j.annemergmed.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–6. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 20.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 21.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 22.Nava S, Navalesi P, Conti G. Time of non-invasive ventilation. Intensive Care Med. 2006;32:361–70. doi: 10.1007/s00134-005-0050-0. [DOI] [PubMed] [Google Scholar]
- 23.Institute of Medicine . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academy of Sciences; 2003. [Google Scholar]
- 24.Office of Statewide Health Planning and Development. California Health and Human Services [Accessed January 9, 2011]; at http://www.oshpd.ca.gov/
- 25.Hsia RY, Srebotnjak T, Kanzaria HK, et al. System-level health disparities in california emergency departments: minorities and medicaid patients are at higher risk of losing their emergency departments. Ann Emerg Med. 2012;59:358–65. doi: 10.1016/j.annemergmed.2011.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mailer’s Software. Melissa Data. Rancho Santa Margarita, CA: [Accessed May 22, 2009]. at http://www.melissadata.com/ [Google Scholar]
- 27.Phibbs CS, Luft HS. Correlation of travel time on roads versus straight line distance. Med Care Res Rev. 1995;52:532–42. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]
- 28.Shen YC, Hsia RY. Does decreased access to emergency departments affect patient outcomes? Analysis of acute myocardial infarction population 1996-2005. Health services research. 2012;47:188–210. doi: 10.1111/j.1475-6773.2011.01319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Brismar B, Dahlgren BE, Larsson J. Ambulance utilization in Sweden: analysis of emergency ambulance missions in urban and rural areas. Ann Emerg Med. 1984;13:1037–9. doi: 10.1016/s0196-0644(84)80065-7. [DOI] [PubMed] [Google Scholar]
- 31.Huang CH, Chen WJ, Ma MH, et al. Ambulance utilization in metropolitan and rural areas in Taiwan. Journal of the Formosan Medical Association = Taiwan yi zhi. 2001;100:581–6. [PubMed] [Google Scholar]
- 32.Canto JG, Zalenski RJ, Ornato JP, et al. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation. 2002;106:3018–23. doi: 10.1161/01.cir.0000041246.20352.03. [DOI] [PubMed] [Google Scholar]
- 33.Faxon D, Lenfant C. Timing is everything: motivating patients to call 9-1-1 at onset of acute myocardial infarction. Circulation. 2001;104:1210–1. [PubMed] [Google Scholar]
- 34.Evenson KR, Foraker RE, Morris DL, et al. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. International journal of stroke : official journal of the International Stroke Society. 2009;4:187–99. doi: 10.1111/j.1747-4949.2009.00276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lindrooth RC, Lo Sasso AT, Bazzoli GJ. The effect of urban hospital closure on markets. J Health Econ. 2003;22:691–712. doi: 10.1016/S0167-6296(03)00060-2. [DOI] [PubMed] [Google Scholar]
- 36.California’s closed hospitals, 1995-2000. The Nicholas C. Petris Center of Health Care Markets and Welfare; [Accessed August 12, 2010]. 2001. at http://www.petris.org/Publications/_Archived_Publications/californias_closed_hospitals.htm. [Google Scholar]
- 37.Fleming ST, Williamson HA, Jr., Hicks LL, et al. Rural hospital closures and access to services. Hospital & health services administration. 1995;40:247–62. [PubMed] [Google Scholar]
- 38.Harrison TD. Consolidations and closures: an empirical analysis of exits from the hospital industry. Health economics. 2007;16:457–74. doi: 10.1002/hec.1174. [DOI] [PubMed] [Google Scholar]
- 39.Hart LG, Pirani MJ, Rosenblatt RA. Causes and consequences of rural small hospital closures from the perspectives of mayors. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 1991;7:222–45. doi: 10.1111/j.1748-0361.1991.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 40.Jollis JG, Peterson ED, DeLong ER, et al. The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med. 1994;331:1625–9. doi: 10.1056/NEJM199412153312406. [DOI] [PubMed] [Google Scholar]
- 41.Gandjour A, Bannenberg A, Lauterbach KW. Threshold Volumes Associated With Higher Survival in Health Care: A Systematic Review. Med Care. 2003;41:1129–41. doi: 10.1097/01.MLR.0000088301.06323.CA. [DOI] [PubMed] [Google Scholar]
- 42.Yaghoubian A, Lewis RJ, Putnam BA, et al. Impact on patient outcomes after closure of an adjacent trauma center. The American surgeon. 2008;74:930–4. [PubMed] [Google Scholar]
- 43.Vogt WB, Town R, Williams CH. How has hospital consolidation affected the price and quality of hospital care? The Synthesis project Research synthesis report. 2006 [PubMed] [Google Scholar]
- 44.Capps C, Dranove D, Lindrooth RC. Hospital closure and economic efficiency. J Health Econ. 2010;29:87–109. doi: 10.1016/j.jhealeco.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 45.Hemmelgarn BR, Ghali WA, Quan H. A case study of hospital closure and centralization of coronary revascularization procedures. CMAJ. 2001;164:1431–5. [PMC free article] [PubMed] [Google Scholar]
- 46.Brownell MD, Roos NP, Burchill C. Monitoring the impact of hospital downsizing on access to care and quality of care. Med Care. 1999;37:JS135–50. doi: 10.1097/00005650-199906001-00013. [DOI] [PubMed] [Google Scholar]
- 47.Mukamel DB, Zwanziger J, Tomaszewski KJ. HMO penetration, competition, and risk-adjusted hospital mortality. Health services research. 2001;36:1019–35. [PMC free article] [PubMed] [Google Scholar]