Abstract
Background
Previous research has shown positive relationships between dysfunctional cognitive styles and different aspects of pain (eg, pain frequency). One goal of our longitudinal study was to investigate potential risk factors for the incidence of headache (HA) and back pain (BP).
Methods
In the first wave (2003), questionnaires were sent to 6,400 children between the ages of 9 and 14 years. Those who answered in wave 1 were contacted again every year (four survey waves in total: 2003–2006). The data presented are based on the children’s self-reports in the second wave (2004) and third wave (2005). Potential risk factors (dysfunctional stress coping, pain catastrophizing, anxiety sensitivity, and somatosensory amplification) were collected in wave 2. Binary logistic regression analyses – for boys and girls – were performed to assess the predictive value of the risk factors for HA and BP in wave 3.
Results
In the comprehensive model, none of the examined variables predicted the incidence of HA. Anxiety sensitivity increased the risk that boys would report BP after 1 year by 50% and dysfunctional stress coping increased the risk by 40%. For girls, somatosensory amplification increased the risk of the incidence of BP 1 year later by 80%, whereas pain catastrophizing reduced the risk by 50%.
Conclusion
In this incidence sample, the amount of variance explained by the psychological variables investigated was very small. Integrating this result with existing findings from cross-sectional studies suggests that dysfunctional cognitive processing styles may develop more as a consequence or a concomitant feature of BP or HA, but play a less important role in its initial development.
Keywords: longitudinal study, risk factors, coping, incidence
Introduction
In recent years, pain in children and adolescents has attracted growing attention. Epidemiological studies show that headache (HA) and back pain (BP) frequently occur in this age group and are often accompanied by psychological problems.1,2 “Dysfunctional stress coping strategies” refer to maladaptive cognitive or behavioral reactions to stress and strain.3 Postal surveys showed that children with recurrent HA (HA twice per week or more) used more dysfunctional stress coping strategies in stressful situations, such as passive avoidance, rumination, resignation, and irritable behavior, than did children without HA.4 However, the causal relationships between stress, dysfunctional stress coping, and HA are still far from understood. Are stress and dysfunctional stress coping risk factors for the development of HA, or does HA increase the risk of stressful experiences and dysfunctional coping?5,6 With regard to BP, the situation is comparable. Stress as a causative factor has rarely been investigated in children.7
Many researchers have investigated to what extent certain appraisals, expectations, and beliefs regarding pain and body sensations, such as pain catastrophizing, anxiety sensitivity, and somatosensory amplification, are correlated with pain. “Catastrophizing” denotes an exaggerated negative cognitive and behavioral preoccupation with pain,8 characterized by an increased attentional focus on pain cognitions, an overestimation of the negative consequences of pain (eg, damage), and the experience of helplessness with regard to pain.9 Several cross-sectional studies8,10,11 and one prospective study12 have found correlations between pain and catastrophizing in children. The construct of “anxiety sensitivity” originated in the context of models of panic disorder and was only subsequently examined with respect to its role in pain experiences.13 Anxiety sensitivity is the disposition of a person to be fearful regarding their own bodily reactions, which are experienced as threatening and dangerous. High anxiety sensitivity increases the fear of pain and may result in avoidance behavior, which may maintain the pain.14,15 “Somatosensory amplification”16 denotes the disposition to focus one’s attentions and perceptions on one’s bodily sensations. This focus is accompanied by a catastrophizing interpretation of these sensations. The concept overlaps to a certain extent with the construct of anxiety sensitivity, but the former places greater emphasis on the perceptional and attentional focus than the latter. Those with high somatosensory amplification may be more prone to chronic pain.17 In their review, Duddu et al18 conclude that the evidence points to a complex, but still unclear, relationship between somatic symptoms and underlying cognitions and illness behaviors.
The objective of the present study was the unidirectional analysis of potential causal factors for the development of pain by means of a longitudinal design. Although temporal priority is not sufficient to establish a causal role for any factor, temporal priority is a necessary condition for such a causal role. We hypothesized that a dysfunctional cognitive processing style, operationalized as dysfunctional stress coping, catastrophizing, anxiety sensitivity, and somatosensory amplification, would increase the risk for the incidence of recurrent pain. In addition, the question of whether these factors exert a differential influence depending on the pain site (HA or BP) is addressed. Since there is evidence of sex-specific effects,8,19 whether the potential risk factors had a different effect in boys and in girls was also investigated.
Methods
Participants
The “KiJuKo” study consisted of a postal survey that was conducted in four waves (W1–W4) in four consecutive years (2003–2006). In the first wave (W1: 2003), 6,400 randomly selected households with a child aged 9–14 years received questionnaires. All participants in W1 were invited to participate again in the following years. The data presented here are based on the children’s and adolescents’ questionnaires from the second (W2: 2004) and third (W3: 2005) waves.
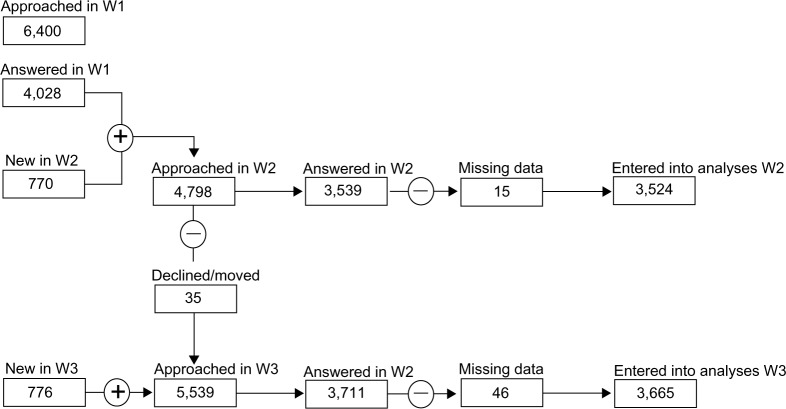
The number of participants in W2 was n=3,524 (73.5% of those contacted). Responder characteristics and selection features are given in Figure 1. The average age of the children in W2 was 11.25 years (± standard deviation 2.28 years; range 8–15 years) and the proportion of boys was 49.5%.20
Figure 1.
Flowchart showing numbers of participating children from W1 to W3.
Notes: Children characterized as “new” participants for W2 and W3 were children who reached the age of 9 years in the interim and thus became eligible for filling in the questionnaire for the first time in that wave.
Abbreviations: W1, wave 1 (2003); W2, wave 2 (2004); W3, wave 3 (2005).
Questionnaire
The KiJuKo questionnaire was developed on the basis of an extensive literature survey and clinical experience. Whenever possible, the operationalization of the potential risk factors was based on established instruments (see Table S1). Detailed information regarding the development of the questionnaire and the procedures, as well as the results of the first wave, has already been published elsewhere.21
Study design
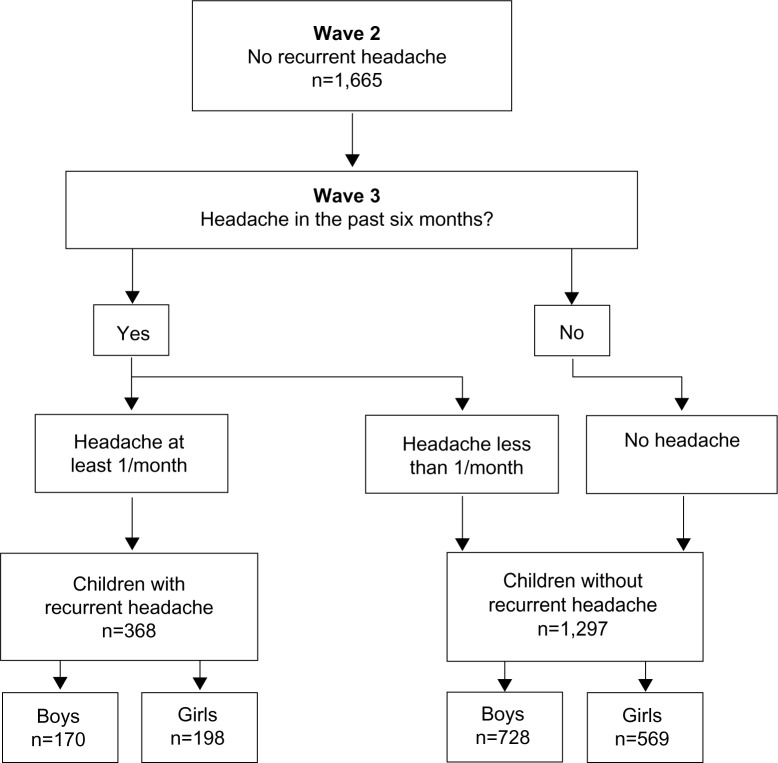
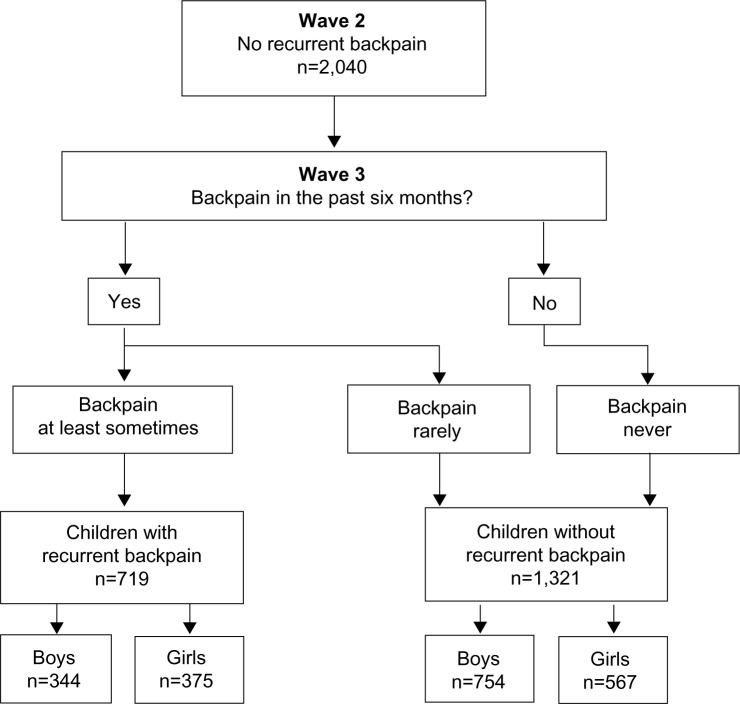
In order to predict the incidence of HA and BP, the questionnaires of all children who did not have HA or BP in W2, but who developed HA or BP 1 year later in W3, were selected for the logistic regression (incidence samples: HA, n=1,665; BP, n=2,040; see Figures 2 and 3).
Figure 2.
Flowchart for the headache incidence sample.
Figure 3.
Flowchart for the back pain incidence sample.
In each wave, the reported HA frequencies within the last 6 months (based on the children’s own reports) were allocated to one of four categories: no HA, HA less than once per month, HA at least once per month, and HA at least once per week. For the regression, the criterion variable was dichotomized in two groups: recurrent HA in W3 “present”, ie, HA once or more per month (n=368, 22.1%), and “not present”, ie, HA less than once per month (n=1,297, 77.9%).
Information on the frequency of BP was collected by means of a 5-point rating scale ranging from “never” to “always”. For BP, a dichotomous variable was generated in analogy to the dependent variable HA, with BP classed as recurrent BP if the child reported having experienced BP at least “sometimes” in the last 6 months. In W3, the number of children with recurrent BP was 719 (35.2%) and without recurrent BP was 1,321 (64.8%). Thus, for both HA and BP, the variables were dichotomized. The cut-off was chosen between “never”/“not at all” (not present =0) and “rarely”/“a little” (present =1), because we assumed that younger children could distinguish more reliably between “no, I never had HA/BP” and “yes, I have had HA/BP” (independently of the frequency of the pain). As an added advantage, dichotomizing facilitates the interpretation of the results.
Apart from age and sex, potential predictors collected in W2 with the children’s and adolescents’ questionnaires (Tables 1–6) were the following variables: dysfunctional stress coping, pain catastrophizing, anxiety sensitivity, and somatosensory amplification. It should be noted that the pain catastrophizing items were only filled in by children 11 years and older, because pilot studies (data on file, 2003) had shown them to be too difficult for younger children.
Table 1.
Dependent variable (criterion 1): headache frequency in the last 6 months (wave 3)
| Headache | Absolute frequency (%) |
|---|---|
| ≥1×/week | 115 (6.7) |
| ≥1×/month | 253 (14.7) |
| <1×/montha | 439 (25.4) |
| No headachea | 858 (49.7) |
| Missing | 60 (3.5) |
| Total | 1,725 (100) |
Note:
Reference categories of items in regression analyses.
Table 6.
Predictor variables for back pain (wave 2)
| Variable | Absolute frequency, n (%)
|
|||||
|---|---|---|---|---|---|---|
| Nevera | Seldom/very little | Sometimes | Often | Always/very much | Missing | |
| Dysfunctional stress coping strategies | 506 (24.8) | 1,015 (49.8) | 419 (20.5) | 63 (3.1) | 2 (0.1) | 35 (1.7) |
| Pain catastrophizingb | 181 (8.9) | 458 (22.5) | 90 (4.4) | 12 (0.6) | – | 1,299 (63.6) |
| Anxiety sensitivity | 1,421 (69.6) | 559 (27.4) | 48 (2.4) | 4 (0.2) | 2 (0.1) | 6 (0.3) |
| Somatosensory amplification | 675 (33.1) | 1138 (55.8) | 209 (10.2) | 10 (0.5) | 2 (0.1) | 6 (0.3) |
Notes:
Reference categories of items in regression analyses;
the pain catastrophizing items were only answered by children aged 11 years or older.
The satisfactory internal consistency (Cronbach’s alpha: α≥0.722 in this study from 0.71 to 0.88; see Table S1) allowed an aggregation of the items belonging to one predictor into a mean scale score per predictor. For the analyses, the predictor variables were dichotomized in the same way as the criterion variables, ie, the reference category is “no/never”.
Statistical analyses
The data were analyzed by means of a binary logistic regression following the recommendations of Field.23 Multicollinearity was excluded on the basis of variance inflation factors and tolerances.24 All variance inflation factor values lay within the range 1–2, indicating that no multicollinearity was present.
In a first step, the predictive values of age and sex with regard to recurrent HA and BP were examined through univariable analyses. Since, in these preliminary analyses, sex emerged as an important factor for the incidence of HA (P<0.05; odds ratio [OR] =1.67; 95% confidence interval [CI] =1.19–2.33) and BP (P<0.05; OR =1.81; 95% CI =1.05–3.09), further analyses were conducted separately for boys and girls. Age was analyzed as a continuous variable and was only relevant in the analyses regarding HA (P=<0.05; OR =1.14; 95% CI =1.01–1.28).
On the basis of these univariable models, all variables with a P-value <0.25 were entered into the multivariable regression model.25 All statistical analyses were conducted using SPSS software (v 14; SPSS Inc., Chicago, IL, USA).
Results
The frequencies for the criterion, control, and predictor variables for HA are reported in Tables 1–3 and for BP in Tables 4–6.
Table 3.
Predictor variables for headache (wave 2)
| Variable | Absolute frequency, n (%)
|
|||||
|---|---|---|---|---|---|---|
| Nevera | Seldom/very little | Sometimes | Often | Always/very much | Missing | |
| Dysfunctional stress coping strategies | 416 (25.0) | 836 (50.2) | 327 (19.6) | 55 (3.3) | 1 (0.1) | 30 (1.8) |
| Pain catastrophizingb | 126 (7.6) | 259 (15.6) | 51 (3.1) | 2 (0.1) | – | 1,227 (73.6) |
| Anxiety sensitivity | 1,197 (71.8) | 426 (25.6) | 30 (1.8) | 3 (0.2) | 1 (0.1) | 8 (0.5) |
| Somatosensory amplification | 602 (36.2) | 894 (53.6) | 152 (9.1) | 6 (0.4) | 3 (0.2) | 8 (0.5) |
Notes:
Reference categories of items in regression analyses;
the pain catastrophizing items were only answered by children aged 11 years or older.
Table 4.
Dependent variable (criterion 2): back pain in the last 6 months (wave 3)
| Back pain | Absolute frequency (%) |
|---|---|
| Always | 4 (0.2) |
| Often | 74 (3.6) |
| Sometimes | 274 (13.4) |
| Seldom | 424 (20.8) |
| Nevera | 1,264 (62) |
| Missing | – |
| Total | 2,040 (100) |
Note:
Reference categories of items in regression analyses.
Prediction of HA incidence
For boys, none of the variables contributed to the development of HA, as no significant ORs were found in the univariable or multivariable analyses (Table 7). Age was included as a control variable in each univariable analysis, and it was found that regardless of the variable investigated the risk of developing HA decreased with increasing age (all ORs for age in these analyses lay between 0.76 and 0.87, P<0.05).
Table 7.
Summary of univariable and multivariable logistic regression analyses predicting the incidence of headache in boys and girls
| Variable | Univariable analyses
|
Multivariable analyses
|
|||||
|---|---|---|---|---|---|---|---|
| P | Odds ratio | 95% confidence interval | Nagelkerke’s pseudo-R2 | P | Odds ratio | 95% confidence interval | |
| Boys | |||||||
| Dysfunctional coping | 0.473 | 1.15 | 0.79–1.68 | 0.019 | – | – | – |
| Pain catastrophizing | 0.486 | 0.79 | 0.40–1.54 | 0.037 | – | – | – |
| Anxiety sensitivity | 0.505 | 1.14 | 0.77–1.68 | 0.020 | – | – | – |
| Somatosensory amplification | 0.980 | 1.01 | 0.71–1.42 | 0.019 | – | – | – |
| Girls | |||||||
| Dysfunctional coping | 0.002 | 2.11 | 1.32–3.36 | 0.021 | 0.386 | 1.54 | 0.58–4.09 |
| Pain catastrophizing | 0.172 | 0.66 | 0.36–1.20 | 0.019 | 0.089 | 0.57 | 0.29–1.09 |
| Anxiety sensitivity | 0.674 | 0.93 | 0.65–1.32 | 0.001 | – | – | – |
| Somatosensory amplification | 0.026 | 1.52 | 1.05–2.19 | 0.010 | 0.297 | 1.43 | 0.73–2.81 |
Note: Nagelkerke’s pseudo-R2 for the multivariable analyses in girls: R2=0.034.
In the univariable analyses for girls, dysfunctional stress coping and somatosensory amplification emerged as influential factors for the incidence of HA 1 year later. For girls who used dysfunctional stress coping, the risk of developing HA was 2.1 times as great compared to girls who never used dysfunctional stress coping. Girls who interpreted bodily sensations in the sense of somatosensory amplification had a 1.5-fold increased risk of developing HA 1 year later. However, both variables lost their significance when they were considered in a multivariable model. Age was irrelevant in all analyses (P>0.10).
Prediction of BP incidence
In the univariable analyses for boys, dysfunctional stress coping, anxiety sensitivity, and somatosensory amplification exerted an influence on the development of BP after 1 year (Table 8). As in the case of HA in boys, age was relevant across all analyses (P<0.05; OR =1.07–1.21).
Table 8.
Summary of univariable and multivariable logistic regression analyses predicting the incidence of back pain in boys and girls
| Variable | Univariable analyses
|
Multivariable analyses
|
|||||
|---|---|---|---|---|---|---|---|
| P | Odds ratio | 95% confidence interval | Nagelkerke’s pseudo-R2 | P | Odds ratio | 95% confidence interval | |
| Boys | |||||||
| Dysfunctional coping | 0.002 | 1.61 | 1.19–2.18 | 0.036 | 0.022 | 1.44 | 1.06–1.97 |
| Pain catastrophizing | 0.785 | 1.07 | 0.66–1.72 | 0.024 | – | – | – |
| Anxiety sensitivity | 0.001 | 1.61 | 1.21–2.15 | 0.036 | 0.012 | 1.47 | 1.09–1.99 |
| Somatosensory amplification | 0.030 | 1.35 | 1.03–1.77 | 0.029 | 0.187 | 1.22 | 0.91–1.62 |
| Girls | |||||||
| Dysfunctional coping | 0.131 | 1.30 | 0.92–1.83 | 0.026 | 0.392 | 1.36 | 0.68–2.72 |
| Pain catastrophizing | 0.068 | 0.63 | 0.39–1.03 | 0.015 | 0.015 | 0.51 | 0.30–0.88 |
| Anxiety sensitivity | 0.291 | 0.86 | 0.65–1.14 | 0.022 | – | – | – |
| Somatosensory amplification | 0.044 | 1.36 | 1.01–1.83 | 0.026 | 0.035 | 1.78 | 1.04–3.05 |
Notes: Nagelkerke’s pseudo-R2 for the multivariable analyses in boys: R2=0.049; for girls R2: =0.036.
The results of the multivariable model pointed to the importance of dysfunctional stress coping and anxiety sensitivity. The risk of developing BP increased by 1.4 if boys reported dysfunctional stress coping (reference: boys who reported that they “never” used these strategies). Anxiety sensitivity increased the risk by 1.5.
Age was shown to be relevant in the multivariable model (P<0.001; OR =1.17; 95% CI =1.08–1.25), ie, with every year of a boy’s life, the risk of developing BP increased by approximately 1.2. The model only explained a very small amount of variance (Nagelkerke’s R2: 0.049).
For girls, only somatosensory amplification was influential in univariable analyses. In the multivariable model, pain catastrophizing emerged as a further relevant factor separate from somatosensory amplification. Girls who focused more sensitively on bodily sensations had a 1.8-fold increased risk of reporting BP 1 year later. Increased pain catastrophizing reduced the risk of developing BP. Girls who reported a catastrophizing style of pain appraisal when they experienced pain had a reduced risk (0.5) of developing BP 1 year later. Age was not relevant in the multivariable model (P>0.10). This model also explained a very small amount of variance (Nagelkerke’s R2: 0.036).
Discussion
The purpose of the study was to examine the role of cognitive processing styles for the new occurrence of HA and BP in youths in a 1-year follow-up. To the best of the authors’ knowledge, this is the first study to contrast potential risk factors for the incidence of BP and HA.
In agreement with our expectations and the findings of existing research, several variables of those we examined proved to be predictors for the development of pediatric pain with differing risk profiles for the development of HA and BP. Our results confirmed existing findings concerning sex-specific effects: more girls than boys experience (6 months’ prevalence)26 and develop (incidence) HA and BP.27 Moreover, our results agree with reported findings19,28 that different factors seem to be relevant for girls and for boys. For boys, none of the variables examined was a risk factor for the incidence of HA. For girls, dysfunctional stress coping and somatosensory amplification showed an influence on the development of HA when analyzed individually, but not when entered into the multivariable model.
For BP, univariable and multivariable analyses showed that dysfunctional stress coping and anxiety sensitivity predicted the development of BP 1 year later for boys. With respect to BP in girls, somatosensory amplification emerged as a factor increasing risk, while pain catastrophizing reduced the risk of developing recurrent BP 1 year later.
In the following discussion, we only refer to the results of the multivariable models, since it is only in this way that the relative impact of the individual variables can be assessed.
The present findings only agree partially with existing studies. Several authors found that children with recurrent HA exhibit more dysfunctional stress coping strategies than children without HA.4,29,30 It was the aim of this study to investigate whether the incidence of HA and BP can be predicted on the basis of dysfunctional stress coping, ie, whether children who showed more dysfunctional stress coping at the time of the first survey would go on to develop recurrent HA 1 year later; clearly, this was not the case, as none of the variables investigated was a predictor for the development of HA. Other studies investigated only correlations between these variables in a cross-sectional study design.30,31 Studies that employed a longitudinal design investigated potential predictors that were not the focus of the present study.32,33
We used a strictly unidirectional design to assess whether cognitive processing styles influence the development of HA. Taken together, our findings and the reports of studies4,29,30 that found an association between HA and dysfunctional coping suggest that HA possibly precedes dysfunctional cognitive processing styles. The causal direction may be from HA to dysfunctional cognitive processes, rather than vice versa. It is possible that repeated experiences of HA lead to children developing dysfunctional pain coping.
For boys, dysfunctional stress coping predicted the new onset of BP. Thus, one can conclude, with some caution, that a dysfunctional stress coping style in the sample described is only predictive for BP in boys. The first longitudinal study in children for the new onset of pain symptoms (lower BP) found that children who reported high levels of psychosocial difficulties, especially conduct problems and hyperactivity, were 1.6 times more likely to develop lower BP.7 Mustard et al found that the risk of the incidence of BP was associated with both low (OR =1.86; 95% CI =1.14–3.03) and moderate/high (OR =1.85; 95% CI =1.07–3.02) levels of psychological distress.34 On the other hand, Brattberg reported that stress perceived in childhood/adolescence did not predict future pain or stress.35
In pediatric pain research, connections between catastrophizing and pain characteristics have been reported,10,12 with stronger catastrophizing in girls than in boys.8 In the present study, however, pain catastrophizing appeared to be relevant for the development of BP in girls, but, surprisingly, in the opposite direction: catastrophizing reduced the risk of reporting BP 1 year later. This unexpected result has to be considered in the context of the fact that only children of 11 years and older filled in the questionnaire, because pilot studies showed the questions to be too difficult for younger children. However, the response rate for the Pain Catastrophizing Scale for Children items was still lower than for other items, something which was observed throughout all waves. This could be due to the fact that the questions may still have been challenging for the children. Therefore, this result will have to be confirmed in further longitudinal analyses before potential explanations can be sought.
For boys, anxiety sensitivity played a role in the development of BP, whereas, for girls, no influence on the development of HA or BP was found.36 In line with existing research,28 we found that girls achieved higher scores for Anxiety Sensitivity Index than boys. However, these scores do not appear to have a predictive role for BP; such a role we found only for boys.
For girls, somatosensory amplification maintains its risk-aggravating influence if it is considered in the comprehensive model. This result supports indications that those individuals who introspect and who have a tendency to select and focus on relatively weak or infrequent sensations (the main elements of somatosensory amplification) might be more prone to experiencing BP.37
What was unexpected was the fact that the variables examined did not have an effect regarding the incidence of HA, but only regarding the development of BP. Future research will have to examine and replicate this result before definite conclusions can be reached.
When considering the results in comparison to those reported in the literature, it has to be taken into account that the present data were collected from a population sample. The findings of Nagel38 support the trend previously reported by Crombez et al8 and Vervoort et al,10 that catastrophizing is more pronounced in clinical samples than in population samples. This argument might also extend to the other psychological constructs and, in our view, may explain the diverging results.
Overall, only a small proportion of the observed variance (for BP: boys, 4.9%, girls, 3.6%) could be explained through the psychological variables we examined. For the prediction of the incidence of recurrent pain, other predictors, which were not considered in the present models, seem to be relevant (see, for example, Kröner-Herwig et al39). Furthermore, it is conceivable that the factors investigated play a more prominent role in the maintenance or exacerbation of recurring pain than in its development.
Strengths and limitations
A particular strength of the present study is the collection of longitudinal data from a large population sample and its use of a strictly defined incidence sample. Moreover, in its investigation of pediatric pain, it was not limited to a single pain site or to the isolated consideration of single psychological variables.
The large population-based study design, however, necessitated the use of self-report measures and precluded any etiological, clinical diagnosis; as a consequence, it is not possible to distinguish between the various subtypes of HA and BP, and, in particular, whether it was a primary or secondary type. This limitation should be taken into account when interpreting the results.
In this study, the interval considered was 1 year. When interpreting the results, the possibility should be taken into account that the influence of certain risk factors may only be observable after a longer period of latency and may thus not be detectable on the basis of the 1-year follow-up data presented here.
A further limitation is the reduction of the sample size that resulted from the fact that we restricted ourselves to the analysis of incidence. This constituted a very strict criterion and thus led to a considerable reduction in the sample size. However, our methodology followed the methodological demands with regard to the development of prognostic models40 that only those participants who do not exhibit a certain feature (eg, pain) at time t1, but develop this at a later time, t2, are included.
In this study, we considered pain frequency. Some researchers advocate the incorporation of pain intensity or impairment resulting from pain; these aspects were not discussed in the present study.
Conclusion
In a longitudinal design using strictly defined incidence samples, we investigated whether cognitive processing styles played a role in the development of HA and BP in boys and girls. Although the influence of the individual variables differed between HA and BP and between boys and girls, the overall role for cognitive styles on the initial development of these conditions was very small.
Supplementary material
Table S1.
Instruments with which the predictor variables (wave 2) were measured
| Predictor variable | Example item | Number of items | Item source | Internal consistency (Cronbach’s α) |
|---|---|---|---|---|
| Dysfunctional stress coping strategies | If other children put me under pressure or I am under pressure in school … Examples: … I would like to pretend to be ill. … I complain about everything. |
5 | SVF-KJ1 | 0.73 |
| Pain catastrophizing | When I am in pain, I worry all the time about whether the pain will end. | 13 | PCS-C5,6 | 0.88 |
| Anxiety sensitivity | It scares me when my heart beats rapidly. | 4 | ASI3,4 | 0.72 |
| Somatosensory amplification | I can sometimes hear my pulse or my heartbeat throbbing in my ear. | 4 | SSAS2 | 0.71 |
Abbreviations: SVF-KJ, German Coping Questionnaire for Children and Adolescents; SSAS, Somatosensory Amplification Scale; ASI, Anxiety Sensitivity Index; PCS-C, Pain Catastrophizing Scale for Children.
References
- 1.Hampel P, Petermann F, Dickow B. Stressverarbeitungsfragebogen von Janke und Erdmann angepasst für Kinder und Jugendliche (SVF-KJ) [Stress Management Questionnaire by Janke and Erdmann Adapted for Children and Adolescents (SVF-KJ)] Göttingen: Hogrefe; 2001. [Google Scholar]
- 2.Barsky AJ, Wyshak G, Klerman GL. The somatosensory amplification scale and its relationship to hypochondriasis. J Psychiatr Res. 1990;24:323–334. doi: 10.1016/0022-3956(90)90004-a. [DOI] [PubMed] [Google Scholar]
- 3.Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 4.Blais MA, Otto MW, Zucker BG, et al. The anxiety sensitivity index: item analysis and suggestions for refinement. J Pers Assess. 2001;77:272–294. doi: 10.1207/S15327752JPA7702_10. [DOI] [PubMed] [Google Scholar]
- 5.Crombez G, Bijttebier P, Eccleston C, et al. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain. 2003;104:639–646. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- 6.Nagel A. Schmerzkatastrophisierung bei Kindern und Jugendlichen mit Kopfschmerzen: Validierung einer Deutschen Version der Pain Catastrophizing Scale for Children [Pain Catastrophizing in Children and Adolescents with Headache: Validity of a Germany Version of the Pain Catastrophizing Scale for Children] [diploma thesis] Göttingen: Georg-August-Universität Göttingen; 2006. German. [Google Scholar]
Table 2.
Control variables for headache: age and sex (wave 2)
| Variable | Absolute frequency (%) |
|---|---|
| Age (years) | |
| 10 | 229 (13.8) |
| 11 | 281 (16.8) |
| 12 | 256 (15.4) |
| 13 | 209 (12.6) |
| 14 | 236 (14.2) |
| 15 | 231 (13.8) |
| 16 | 179 (10.8) |
| 17 | 44 (2.6) |
| Sex | |
| Boysa | 898 (53.9) |
| Girls | 767 (46.1) |
Note:
Reference categories of items in regression analyses.
Table 5.
Control variables for back pain: age and sex (wave 2)
| Variable | Absolute frequency (%) |
|---|---|
| Age (years) | |
| 10 | 302 (14.7) |
| 11 | 359 (17.6) |
| 12 | 336 (16.5) |
| 13 | 299 (14.7) |
| 14 | 265 (13) |
| 15 | 231 (11.3) |
| 16 | 198 (9.7) |
| 17 | 50 (2.5) |
| Sex | |
| Boysa | 1,098 (53.8) |
| Girls | 942 (46.2) |
Note:
Reference categories of items in regression analyses.
Acknowledgments
This research project has been supported by a grant from the German Ministry of Education, Research and Science (BMBF) (Grant 01 EM 0521) as part of the German Headache Consortium. We acknowledge the support by the German Research Foundation and the Open Access Publication Fund of the Göttingen University.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Roth-Isigkeit A, Thyen U, Raspe HH, Stöven H, Schmucker P. Reports of pain among German children and adolescents: an epidemiological study. Acta Paediatr. 2004;93:258–263. [PubMed] [Google Scholar]
- 2.Heinrich M, Morris L, Kröner-Herwig B. Self-report of headache in children and adolescents in Germany: possibilities and confines of questionnaire data for headache classification. Cephalalgia. 2009;29:864–872. doi: 10.1111/j.1468-2982.2008.01812.x. [DOI] [PubMed] [Google Scholar]
- 3.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer Publishing Company; 1984. [Google Scholar]
- 4.Saile H, Scalla P. Chronische Kopfschmerzen und Stress bei Kindern [Chronic headaches and stress in children] Z Klin Psychol Psychiatr Psychother. 2006;35:188–195. German. [Google Scholar]
- 5.Waldie KE. Childhood headache, stress in adolescence, and primary headache in young adulthood: a longitudinal cohort study. Headache. 2001;41:1–10. doi: 10.1046/j.1526-4610.2001.111006001.x. [DOI] [PubMed] [Google Scholar]
- 6.Bandell-Hoekstra I, Abu-Saad HH, Passchier J, Knipschild P. Recurrent headache, coping, and quality of life in children: a review. Headache. 2000;40:357–370. doi: 10.1046/j.1526-4610.2000.00054.x. [DOI] [PubMed] [Google Scholar]
- 7.Jones GT, Watson KD, Silman AJ, Symmons DP, Macfarlane GJ. Predictors of low back pain in British schoolchildren: a population-based prospective cohort study. Pediatrics. 2003;111:822–828. doi: 10.1542/peds.111.4.822. [DOI] [PubMed] [Google Scholar]
- 8.Crombez G, Bijttebier P, Eccleston C, et al. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain. 2003;104:639–646. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- 10.Vervoort T, Goubert L, Eccleston C, Bijttebier P, Crombez G. Catastrophic thinking about pain is independently associated with pain severity, disability, and somatic complaints in school children and children with chronic pain. J Pediatr Psychol. 2006;31:674–683. doi: 10.1093/jpepsy/jsj059. [DOI] [PubMed] [Google Scholar]
- 11.Lynch AM, Kashikar-Zuck S, Goldschneider KR, Jones BA. Psychosocial risks for disability in children with chronic back pain. J Pain. 2006;7:244–251. doi: 10.1016/j.jpain.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Vervoort T, Eccleston C, Goubert L, Buysse A, Crombez G. Children’s catastrophic thinking about their pain predicts pain and disability 6 months later. Eur J Pain. 2010;14:90–96. doi: 10.1016/j.ejpain.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 14.Asmundson GJ, Norton PJ, Veloso F. Anxiety sensitivity and fear of pain in patients with recurring headaches. Behav Res Ther. 1999;37:703–713. doi: 10.1016/s0005-7967(98)00172-7. [DOI] [PubMed] [Google Scholar]
- 15.Norton PJ, Asmundson GJ. Anxiety sensitivity, fear, and avoidance behavior in headache pain. Pain. 2004;111:218–223. doi: 10.1016/j.pain.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 16.Barsky AJ, Wyshak G, Klerman GL. The somatosensory amplification scale and its relationship to hypochondriasis. J Psychiatr Res. 1990;24:323–334. doi: 10.1016/0022-3956(90)90004-a. [DOI] [PubMed] [Google Scholar]
- 17.Ak I, Sayar K, Yontem T. Alexithymia, somatosensory amplification and counter-dependency in patients with chronic pain. The Pain Clinic. 2004;16:43–51. [Google Scholar]
- 18.Duddu V, Isaac MK, Chaturvedi SK. Somatization, somatosensory amplification, attribution styles and illness behaviour: a review. Int Rev Psychiatry. 2006;18:25–33. doi: 10.1080/09540260500466790. [DOI] [PubMed] [Google Scholar]
- 19.Hampel P, Petermann F. Age and gender effects on coping in children and adolescents. J Youth Adolesc. 2005;34:73–83. [Google Scholar]
- 20.Gassmann J, Morris L, Heinrich M, Kröner-Herwig B. One-year course of paediatric headache in children and adolescents aged 8–15 years. Cephalalgia. 2008;28:1154–1162. doi: 10.1111/j.1468-2982.2008.01657.x. [DOI] [PubMed] [Google Scholar]
- 21.Kröner-Herwig B, Heinrich M, Morris L. Headache in German children and adolescents: a population-based epidemiological study. Cephalalgia. 2007;27:519–527. doi: 10.1111/j.1468-2982.2007.01319.x. [DOI] [PubMed] [Google Scholar]
- 22.Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. New York: McGraw-Hill; 1994. [Google Scholar]
- 23.Field A. Discovering Statistics Using SPSS. 3rd ed. London: Sage Publications Ltd; 2009. [Google Scholar]
- 24.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th ed. Boston: Allyn and Bacon; 2001. [Google Scholar]
- 25.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York: John Wiley & Sons, Inc; 2000. [Google Scholar]
- 26.Brattberg G, Wickman V. Prevalence of back pain and headache in Swedish school children: a questionnaire survey. The Pain Clinic. 1992;5:211–220. [Google Scholar]
- 27.Brattberg G. The incidence of back pain and headache among Swedish school children. Qual Life Res. 1994;3(Suppl 1):S27–S31. doi: 10.1007/BF00433372. [DOI] [PubMed] [Google Scholar]
- 28.Walsh TM, Stewart SH, McLaughlin E, Comeau N. Gender differences in Childhood Anxiety Sensitivity Index (CASI) dimensions. J Anxiety Disord. 2004;18:695–706. doi: 10.1016/S0887-6185(03)00043-4. [DOI] [PubMed] [Google Scholar]
- 29.Luka-Krausgrill U, Reinhold B. Kopfschmerzen bei Kindern: Auftretensrate und Zusammenhang mit Streß, Streßbewältigung, Depressivität und sozialer Unterstützung [Headaches in children: incidence rate and association with stress, stress management, depression and social support] Zeitschrift für Gesundheitspsychologie. 1996;4:137–151. German. [Google Scholar]
- 30.Bandell-Hoekstra IE, Abu-Saad HH, Passchier J, Frederiks CM, Feron FJ, Knipschild P. Coping and quality of life in relation to headache in Dutch schoolchildren. Eur J Pain. 2002;6:315–321. doi: 10.1053/eujp.2002.0343. [DOI] [PubMed] [Google Scholar]
- 31.Lateef TM, Merikangas KR, He J, et al. Headache in a national sample of American children: prevalence and comorbidity. J Child Neurol. 2009;24:536–543. doi: 10.1177/0883073808327831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laimi K, Metsähonkala L, Anttila P, et al. Outcome of headache frequency in adolescence. Cephalalgia. 2006;26:604–612. doi: 10.1111/j.1468-2982.2004.01084.x. [DOI] [PubMed] [Google Scholar]
- 33.Rhee H. Prevalence and predictors of headaches in US adolescents. Headache. 2000;40:528–538. doi: 10.1046/j.1526-4610.2000.00084.x. [DOI] [PubMed] [Google Scholar]
- 34.Mustard CA, Kalcevich C, Frank JW, Boyle M. Childhood and early adult predictors of risk of incident back pain: Ontario Child Health Study 2001 follow-up. Am J Epidemiol. 2005;162:779–786. doi: 10.1093/aje/kwi271. [DOI] [PubMed] [Google Scholar]
- 35.Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain. 2004;8:187–199. doi: 10.1016/j.ejpain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 36.Deacon BJ, Valentiner DP, Gutierrez PM, Blacker D. The Anxiety Sensitivity Index For Children: factor structure and relation to panic symptoms in an adolescent sample. Behav Res Ther. 2002;40:839–852. doi: 10.1016/s0005-7967(01)00076-6. [DOI] [PubMed] [Google Scholar]
- 37.Hasenbring MI, Rusu AC, Turk DC, editors. From Acute to Chronic Back Pain: Risk Factors, Mechanisms, and Clinical Implications. Oxford: Oxford University Press; 2012. [Google Scholar]
- 38.Nagel A. Schmerzkatastrophisierung bei Kindern und Jugendlichen mit Kopfschmerzen: Validierung einer Deutschen Version der Pain Catastrophizing Scale for Children [Pain Catastrophizing in Children and Adolescents with Headache: Validity of a German Version of the Pain Catastrophizing Scale for Children] [diploma thesis] Göttingen: Georg-August-Universität Göttingen; 2006. German. [Google Scholar]
- 39.Kröner-Herwig B, Morris L, Heinrich M. Biopsychosocial correlates of headache: what predicts pediatric headache occurrence? Headache. 2008;48:529–544. doi: 10.1111/j.1526-4610.2007.00945.x. [DOI] [PubMed] [Google Scholar]
- 40.Höfler M. Statistik in der Epidemiologie psychischer Störungen[Statistics in the Epidemiology of Mental Disorders] Berlin: Springer Verlag; 2004. German. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Instruments with which the predictor variables (wave 2) were measured
| Predictor variable | Example item | Number of items | Item source | Internal consistency (Cronbach’s α) |
|---|---|---|---|---|
| Dysfunctional stress coping strategies | If other children put me under pressure or I am under pressure in school … Examples: … I would like to pretend to be ill. … I complain about everything. |
5 | SVF-KJ1 | 0.73 |
| Pain catastrophizing | When I am in pain, I worry all the time about whether the pain will end. | 13 | PCS-C5,6 | 0.88 |
| Anxiety sensitivity | It scares me when my heart beats rapidly. | 4 | ASI3,4 | 0.72 |
| Somatosensory amplification | I can sometimes hear my pulse or my heartbeat throbbing in my ear. | 4 | SSAS2 | 0.71 |
Abbreviations: SVF-KJ, German Coping Questionnaire for Children and Adolescents; SSAS, Somatosensory Amplification Scale; ASI, Anxiety Sensitivity Index; PCS-C, Pain Catastrophizing Scale for Children.