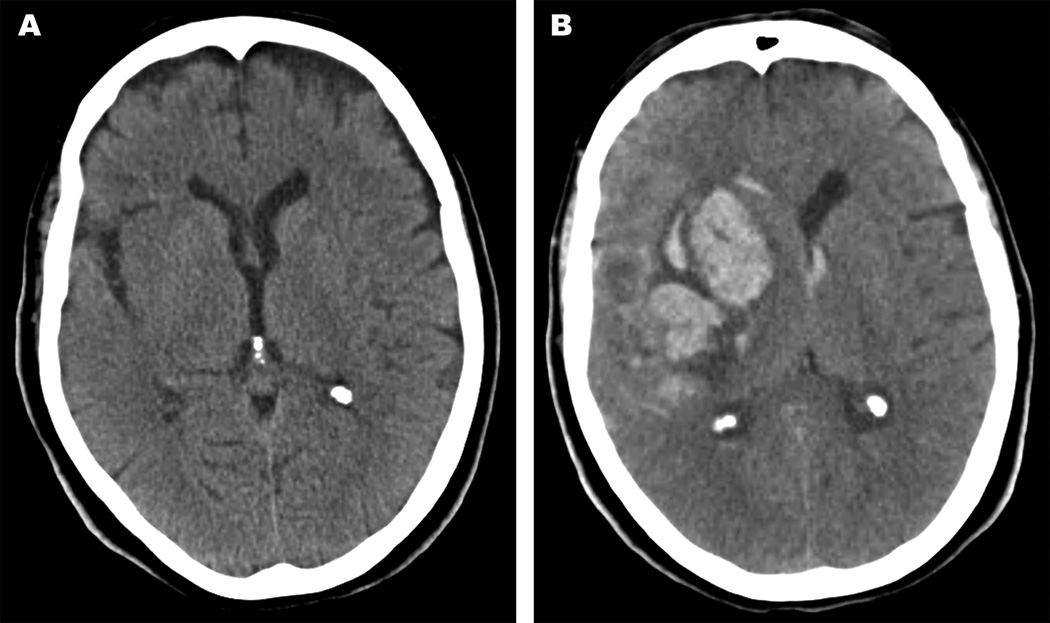
Figure 2.
A 70-year old female presented with acute ischemic stroke in the right middle cerebral artery distribution and an admission NIHSS of 6. There was no evidence of ICH at presentation (Figure 2A). She underwent thrombolysis with tPA and post-thrombolysis NIHSS was 1. Digital subtraction angiography demonstrated 75% stenosis in the proximal right internal carotid artery, and she underwent carotid endarterectomy 3 days after presentation. The patient experienced acute mental status decline and left hemiparesis on post-operative day 1, and head CT showed an ICH (Figure 2B). A craniotomy and clot evacuation was emergently performed, resulting in improved neurological status. However, the patient developed additional complications following her craniotomy including repeat sICH as well as ventriculitis resulting in further deterioration of her neurological status. Ultimately, the family withdrew care and the patient died 38 days after presentation.