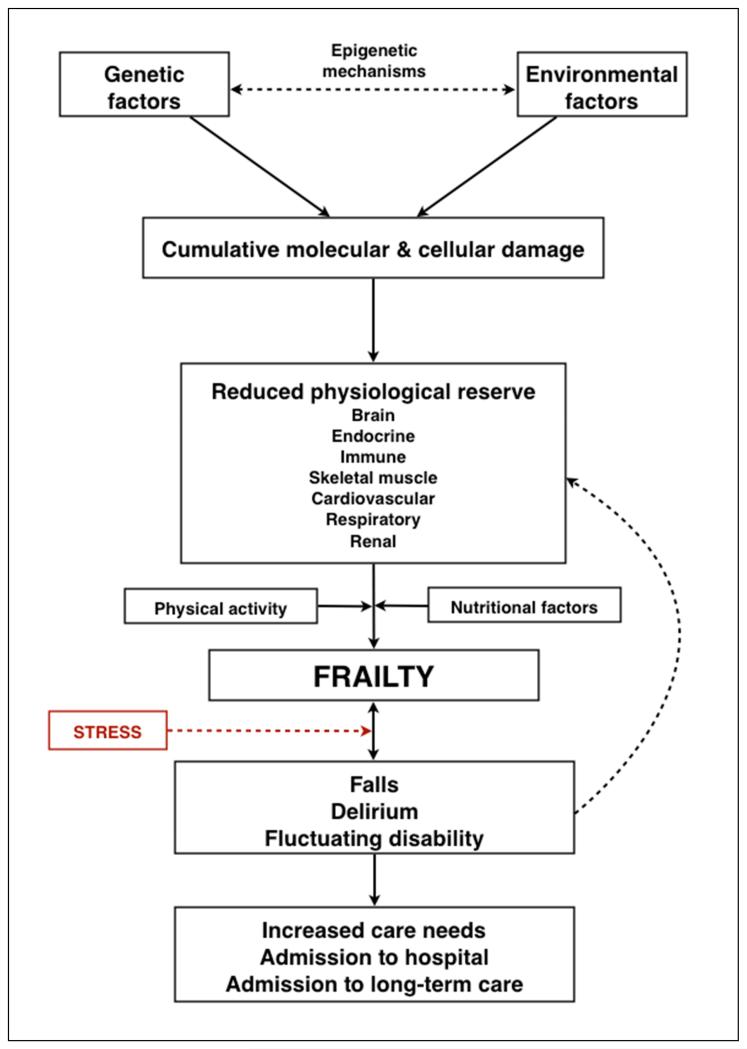
Figure 2.
A schematic representation of the pathophysiology of frailty.
Ageing is considered to result from the lifelong accumulation of molecular and cellular damage caused by multiple mechanisms regulated by a complex maintenance and repair network under the influence of genetic, environmental and epigenetic mechanisms. There is uncertainty regarding the precise level of cellular damage required to cause impaired organ physiology but, importantly, many organ systems exhibit considerable redundancy, which provides the physiological reserve required to compensate for age and disease-related changes. The brain, endocrine system, immune system and skeletal muscle are intrinsically inter-related and are currently the organ systems best studied in the development of frailty. Loss of physiological reserve in other systems including the cardiovascular, respiratory and renal systems also contributes. Influenced by level of physical activity and nutritional factors, cumulative loss of physiological reserve in these organ systems can lead to frailty, which is characterised by increased vulnerability to poor resolution of homeostasis following a stress, increasing the risk of adverse outcomes including falls, delirium and disability. These are common clinical presentations of frailty, are common reasons for admission to hospital and can accelerate further decline. Both frailty itself and these common clinical presentations identify those at increased risk of requiring care at home and long-term care admission.