Abstract
Background
The effect of donor-recipient human leukocyte antigen (HLA) matching on outcomes remains relatively unexplored in pediatric patients. The objective of this study was to investigate the effects of donor-recipient HLA matching on graft survival in pediatric heart transplantation.
Methods and Results
The UNOS database was queried for heart transplants occurring between October 31, 1987 to December 31, 2012 in a recipient aged ≤ 17 with at least one postoperative follow-up visit. Retransplants were excluded. Transplants were divided into 3 donor-recipient matching groups: no HLA matches (HLA-no), 1 or 2 HLA matches (HLA-low), and 3-6 HLA matches (HLA-high). Primary outcome was graft loss. 4471 heart transplants met study inclusion criteria. High degree of donor-recipient HLA matching occurred infrequently; (HLA-high n=269 (6 %) v. HLA-low n=2683 (60%) v. HLA-no n=1495 (34%). There were no differences between HLA matching groups in frequency of coronary vasculopathy (p=0.19) or rejection in the first post-transplant year (p=0.76). Improved graft survival was associated with a greater degree of HLA donor-recipient matching: HLA-high median survival 17.1yrs (14.0-20.2yrs, 95%CI), HLA-low median survival 14.2yrs (13.1-15.4), and HLA-no median survival 12.1yrs (10.9-13.3), p<0.01 log rank test. In Cox-regression analysis, HLA matching was independently associated with decreased graft loss [HLA-low v. HLA-no HR 0.86 (0.74-0.99, 95%CI), p=0.04; HLA-high v. HLA-no 0.62 (0.43-0.90, 95%CI), p<0.01].
Conclusions
Decreased graft loss in pediatric heart transplantation was associated with a higher degree of donor-recipient HLA matching, although a difference in the frequency of early rejection or development of coronary artery vasculopathy was not seen.
Keywords: heart transplantation, outcome, pediatric
Human leukocyte antigen (HLA) typing of potential donors and recipients is standard of care in pediatric heart transplantation. Advancing knowledge of HLA antibodies has improved the accuracy of virtual crossmatch in sensitized patients1, reducing the need for prospective crossmatches and leading to reduced waitlist mortality.2 These improvements in HLA technology have likely led to improved outcomes in pediatric heart transplantation by optimizing donor selection.1
Despite improved outcomes through the virtual crossmatch, the effect of donor-recipient HLA matching on outcomes remains relatively unexplored in pediatric heart transplantation. Opelz et al. reviewed the impact of HLA compatibility on 150,000 kidney, heart and liver transplants and found that kidney and heart transplant outcomes were improved with higher degrees of HLA matching.3 A previous report by Opelz and Wujciak showed that HLA matching of 3 or more loci was associated with improved outcomes in an exclusively heart transplant cohort.4 There are other reports that indicate that HLA matching is associated with a decreased risk of rejection in the first post-transplant year, decrease incidence of coronary vasculopathy as well as improved graft survival.5, 6
However, other studies indicate HLA matching does not improve outcomes in heart transplantion. Tenderich et al. performed a single center retrospective review of 923 adult heart transplants from 1989 to 2005 and found that the degree of HLA donor-recipient matching was not associated with short or long-term survival.7 Similarly, a single center retrospective study of 243 heart transplants over a 13-year period, did not find a relationship between HLA matching and survival, rejection episodes or post-transplant infections.8 The latter study included adolescents between ages 12 to 18, but no subgroup analysis was performed on this pediatric group.8
The only previous report exploring an association between HLA matching and outcomes in an exclusively pediatric population found no improvement in survival but was a single center study reported more than 20 years ago involving 87 patients.9 The aim of this study was to investigate possible associations between HLA matching and graft survival in an exclusively pediatric cohort.
Methods
A retrospective analysis was performed on data obtained from the UNOS Standard Transplant Analysis and Research (STAR) files. The Medical University of South Carolina Institutional Review Board approved the study. Heart transplants performed in the United States between October 1,1987 through December 31, 2012 were included for analysis. The database was queried for pediatric heart transplants (age 17 or younger) who underwent heart transplant and had HLA typing of the recipient and donor at the A, B, and DR locus. Transplants were included if there was at least one follow-up visit documented. Transplants were excluded if the recipient had a previous heart transplantation. Primary endpoint for the study was graft loss, which includes patient death and retransplantation.
HLA matching was defined as the number of donor HLA antigens that were also present in the recipient. Transplants were divided into three groups, no HLA matching [0 of 6 potential matches (HLA-no)], low level of HLA matching [1-2 of 6 potential matches (HLA-low)] and high level of HLA matching [3-6 potential matches (HLA-high)]. Patient specific variables evaluated between groups included: recipient supported by inotropic medications, extracorporeal membrane oxygenation (ECMO), ventricular assist device (VAD), and/or mechanical ventilation immediately prior to transplant; cardiac diagnosis (cardiomyopathy, congenital heart disease, or other), recipient race, age, serum creatinine and bilirubin at transplant, ischemic time, donor-recipient weight ratio, crossmatch results, and year of transplant. For VADs, the type of VAD (LVAD, RVAD and BiVAD) is noted. Given the small total number of VADs, for statistical purposes all types of VADs were grouped together. These variables have been previously been shown to be associated with graft survival.10-12
Secondary endpoints included the development of coronary vasculopathy throughout the life of the graft and rejection requiring treatment in the first year post-transplant year. In order to allow for at least one year following transplant for the assessment of rejection or the development coronary vasculopathy, only transplants prior to December 31, 2011 were included for analysis of these endpoints. Rejection in the first transplant year was treated as dichotomous outcome (1 or more episode of rejection versus no episodes).
An additional analysis compared outcomes in patients based upon the presence of matching HLA at each individual locus (A, B, DR). Each individual locus was analyzed separately independent of matching at other locus (no A-locus matching versus at least one A-locus match; no B-locus matching versus at least one B-locus match; no DR-locus matching versus at least one DR-locus match).
To investigate the relationship between the race of donor and donor:recipient racial matching on HLA matching, recipients and donors were classified by the following groups: Caucasian, African-American, Hispanic, Asian or Other. Degree of HLA matching was compared between groups based upon recipient race as well as if there was donor:recipient racial matching.
Statistical Analysis
Data from the UNOS STAR files were imported into SPSS®, version 21.0 (IBM© Armonk, NY) for analysis. Demographic and patient variable data are reported as medians with intra quartile ranges, or ninety-five percent confidence interval, or as percentages as appropriate. Demographics and patient variables were compared among the 3 groups using Kruskis-Wallis test for continuous variables as data had nonparametric distribution. Categorical variables were compared between HLA donor-recipient matching groups using chi-square test. Cox proportional hazard models were used to assess hazard ratios of graft loss between HLA match groups while controlling for age, year of transplant; recipient on ECMO, VAD, IV inotropes or mechanical ventilation immediately prior to transplant, cardiac diagnosis, serum bilirubin and creatinine, donor-recipient weight ratio and pro- or retrospective crossmatch results. For the purpose of the multivariate cox-regression analysis continuous variables of transplant year and age were divided to create categorical variables: early transplant year (1987-1999) versus late transplant year (2000-2012); infant (<1 year of age), child (1-10 years) and adolescent (11-17 years). Positive and indeterminate retrospective crossmatches were combined into one category for multivariate analysis. Recipient race was divided into Caucasian and non-Caucasian. Only data sets with complete data were used in the Cox proportional hazard models, missing data was not interpolated. HLA-no was the reference group in multivariable analysis.
In additional analysis of matching at each individual HLA locus, demographic and patient variable data were compared between groups using Wilcoxon-rank sum test for continuous variables. For categorical variables, comparisons between groups were performed using the chi-square test. Cox proportional hazard models were performed in the same manner as previously described. A p-value of <0.05 was set as statistically significant.
When analyzing race and HLA matching, degree of HLA-matching and frequency of donor:recipient racial matching was compared between recipient racial groups using Chi-Square test. Graft survival was compared using log rank test.
Results
There were 4471 pediatric heart transplants that met study inclusion criteria. Median recipient age of the study population was 5 years (IQR 0-13) with 1291 transplants having a recipient age <1 year, 1635 with recipient age from 1-10 years, and 1521 transplants with recipient age between 11-17 years of age. An underlying diagnosis of cardiomyopathy existed in 2311, 1943 had congenital heart disease, and 193 were reported to have other cardiac diagnoses. Median serum creatinine was 0.5 mg/dL (IQR 0.4-0.8); median serum bilirubin was 0.7 mg/dL (0.4-1.3). Median donor-recipient weight ratio was 1.27 (IQR 1.0-1.7). Median ischemic time was 3.5 hours (IQR 2.8-4.3). One hundred sixty-four (4%) of recipients were on ECMO at the time of transplant, 702 (16%) were on mechanical ventilation and 1878 (42%) were on inotropic support. A total of 228 (5%) patients were on a VAD at time of transplant (109 LVADs, 1 RVAD, 3 Total Artificial Heart, 56 BiVAD and 59 not specified.) Median graft survival for the entire cohort was 13.5 years (12.7-14.4, 95% CI).
A high degree of HLA matching occurred infrequently [HLA-high n=269 (6%) v. HLA-low n=2683 (60%) v. HLA-no n=1495 (34%)]. Patient specific factors did not differ between HLA matching groups (Table 1), except that the HLA-high group was more likely to be on ECMO at the time of transplant (7% HLA-high v. 4% HLA-low v. 3% HLA-no, p<0.01) and more likely to be Caucasian (70.3% HLA-high v. 60.5% v. 54.6%, p<0.01). Median graft survival differed between groups (Figure, p<0.01); the HLA-high group had an estimated median survival of 17.1yrs (14.0-20.2yrs, 95%CI), versus HLA-low of 14.2 years (13.1-15.4yrs, 95%CI), and HLA-no of 12.1 years (10.9-13.3, 95%CI).
Table 1.
Patient Characteristics and HLA matching group
| No HLA match (n=1592) | Low HLA match (1-2 matches, n=2852) | High HLA match (3-6 matches, n=287) | P-value | |
|---|---|---|---|---|
| Recipient Age (years) | 5 (0-13) | 5 (0-13) | 5 (0-13) | 0.97 |
| Recipient Race (% Caucasian) | 54.6 | 60.5 | 70.3 | <0.01 |
| Transplant Year | 2005 (1996-2009) | 2005 (1996-2009) | 2006 (1996-2010) | 0.69 |
| Serum Creatinine (mg/dL) | 0.5 (0.4-0.7) | 0.5 (0.4-0.7) | 0.5 (0.3-0.7) | 0.52 |
| Total Bilirubin (mg/dL) | 0.7 (0.4-1.3) | 0.7 (0.4-1.3) | 0.7 (0.5-1.3) | 0.81 |
| Ischemic Time (hours) | 3.5 (2.8-4.3) | 3.5 (2.8-4.2) | 3.5 (2.8-4.2) | 0.81 |
| Donor-Recipient weight ratio | 1.3 (1.0-1.6) | 1.3 (1.0-1.6) | 1.3 (1.0-1.6) | 0.76 |
| IV* Inotropes | 635 (43%) | 1131 (42%) | 112 (42%) | 0.96 |
| Recipient on Ventilator | 233 (16%) | 422 (16%) | 47 (18%) | 0.73 |
| VAD support | 69 (5%) | 136 (5%) | 16 (6%) | 0.61 |
| Recipient on ECMO | 46 (3%) | 99 (4%) | 19 (7%) | <0.01 |
| Positive or Indeterminate Crossmatch | 96 (7%) | 172 (7%) | 17 (7%) | 0.99 |
| Cardiac Diagnosis | ||||
| Cardiomyopathy | 811 (54%) | 1374 (51%) | 126 (47%) | |
| Congenital Heart Disease | 621 (42%) | 1189 (44%) | 133 (49%) | 0.17 |
| Other | 63 (4%) | 120 (5%) | 10 (4%) |
IV=intravenous
HLA matching group (no, low, and high) had similar characteristics except that HLA-high was more likely to be on ECMO and Caucasian.
Figure. Graft Survival by HLA Matching Group.
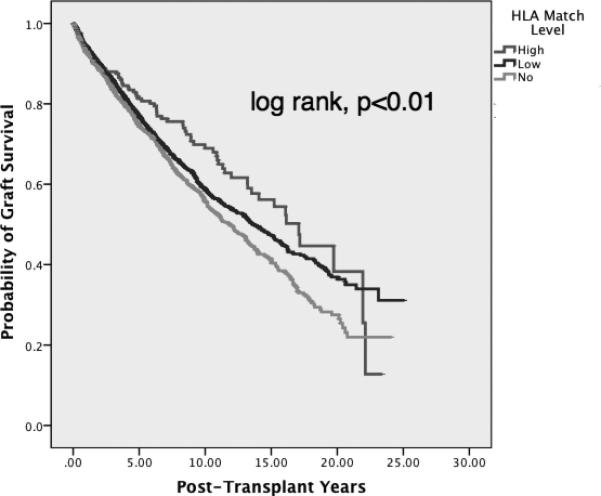
Kaplan-Meier survival curves comparing 3 groups of HLA donor-recipient matches. Higher degree of HLA matching was associated with improved survival (p<0.01, log rank)
Of the 4471 heart transplants with at least one follow-up post-transplant visit, 4330 were performed prior to December 31, 2011 and comprised the group that was assessed for coronary vasculopathy and rejection. The frequency of coronary vasculopathy did not differ between groups, 25% (n=67) for HLA-high, 21% for HLA-low (n=558) and 22% (n=335) for HLA-no (p=0.19). The frequency of treated rejection in the first post transplant year also did not differ between groups, 20% (n=55) for HLA-high, 22% for HLA-low (n=588) and 23% (n=342) for HLA-no (p=0.76). Neither frequency of coronary vasculopathy nor rejection within the first year was associated with HLA matching when the cohort was divided in infants (<1year of age) and non-infants (≥1year of age)
Multivariable Cox-regression analysis was performed on all 2852 of 4447 transplants with no missing data. Differences between the transplants with complete datasets and those with incomplete datasets are summarized in Table 2. HLA matching was independently associated with graft survival. When compared to the HLA-no, HLA-low had a hazard ratio of 0.86 (95% CI: 0.74-0.99,p=0.04) for graft loss and HLA-high had a hazard ratio of 0.62 (95%CI: 0.43-0.90, p=0.01) for graft loss. When patients with no HLA matching were excluded, HLA-high had a hazard ratio for graft loss of 0.7 (0.5-1.0, 95%CI, p=0.07) compared HLA-low. When analyzing infants separately (recipient age<1yr, n=1291) there was no difference in graft survival between HLA-no (14.9yrs) v. HLA-low (16.3yrs) v. HLA-high (15.7yrs), p=0.47. In multivariable cox-regression analysis of infants, HLA matching class was not associated with graft survival. However, in patients >1 year, associations with graft survival were similar to the entire cohort.
Table 2.
Comparison of transplants with missing data versus complete data for multivariate analysis
| Missing Data (n=1595) | Compete Data (n=2852) | p-value | |
|---|---|---|---|
| Recipient Age (years) | 6 (0-13) | 5 (0-13) | <0.01 |
| Recipient Race (% Caucasian) | 61.6 | 57.7 | <0.01 |
| Transplant Year | 2003 (1998-2006) | 2006 (2000-2009) | <0.01 |
| Serum Creatinine (mg/dL) | 0.5 (0.4-0.8) | 0.5 (0.4-0.7) | 0.25 |
| Total Bilirubin (mg/dL) | 0.7 (0.4-1.2) | 0.7 (0.4-1.3) | 0.54 |
| Ischemic Time (hours) | 3.6 (2.7-4.5) | 3.5 (2.8-4.2) | 0.58 |
| Donor-Recipeint weight ratio | 1.3 (1.1-1.6) | 1.3 (1.0-1.6) | 0.01 |
| IV* Inotropes | 447 (28%) | 1431 (50%) | <0.01 |
| Recipient on Ventilator | 237 (15%) | 465 (16%) | 0.21 |
| VAD Support | 50 (3%) | 171 (6%) | <0.01 |
| Recipient on ECMO | 38 (2.4%) | 126 (4.4%) | <0.01 |
| Positive or Indeterminate | |||
| Crossmatch | 67 (6%) | 218 (8%) | 0.07 |
| Cardiac Diagnosis | |||
| Cardiomyopathy | 779 (49%) | 1532 (54%) | |
| Congenital Heart Disease | 748 (47%) | 1195 (62%) | <0.01 |
| Other | 68 (4%) | 125 (4%) | |
| HLA match level | |||
| No match | 590 560 (35%) | 1002 935 (33%) | |
| Low match (1-2 matches) | 986 938 (59%) | 1866 1745 (61%) | |
| High match (3-6 matches) | 103 97 (6%) | 184 172 (6%) | 0.27 |
IV=intravenous
Patients not included in multivariable analysis due to missing data points were less likely to be ECMO, VAD, or on IV inotropes, more likely to have congenital heart disease, Caucasian and tended to be younger.
Additional analysis of graft survival was performed between matching at each individual HLA locus. Transplants that had 1 or 2 matches at the A-locus (n=1772) had a longer estimated median graft survival, in univariate analysis, of 15.2 years (95%CI: 13.5-16.9) versus transplants that had no match (n=2675), 12.9 years (11.9-13.9, p<0.01 log rank test). In multivariable Cox regression analysis, matching at the A-locus had a hazard ratio of 0.88 (0.76-1.02, p=0.11) for graft loss compared to no matching (Table 3). In univariate analysis, matching at the B-locus did not lead to statistically significant longer median graft survival. However, in multivariable Cox regression analysis matching at the B-locus was independently associated with lower hazard ratio of graft loss when compared to no match group (HR 0.80, 95%CI: 0.67-0.97, p=0.03). Matching at the DR-locus was associated with longer estimated median graft survival in univariate analysis, 15.1yrs (95%CI: 13.7-16.7) for transplants with one match vs. 13.0yrs (12.0-14.0yrs) for transplants with no match (p<0.01), but in Cox-regression analysis this association was no longer significant (Table 3).
Table 3.
Graft survival multivariable analysis by HLA locus
| Hazard ratio for graft loss (95%CI) | p-value | |
|---|---|---|
| A-locus | ||
| ≥ 1 match versus no match | 0.88 (0.76-1.02) | 0.11 |
| B-locus | ||
| ≥ 1 match versus no match | 0.80 (0.67-0.97) | 0.03 |
| DR-locus | ||
| ≥ 1 match versus no match | 0.91 (0.78-1.1) | 0.19 |
Matching at A and B-loci was associated with better graft survival in multivariable Cox regression analysis
The race of the entire transplant recipient cohort was 59.1% Caucasian, 19.7% African-American, 15.5% Hispanic, 3.1% Asian and 2.6% other. Donor race was Caucasian in 59.1% of transplants, 19.7% African-American, 15.5% Hispanic, 3.1% Asian, and 2.5% other. Two donors did not have race recorded. Caucasian recipients received the same race donor 64.3% of the time versus, 22.2% for African-Americans, 26.5% for Hispanics, 0.7% for Asians, and 0.9% for other (p<0.01). Transplants with donor-recipient racial matching were more likely to be in HLA-high (8.4% v. 4.0%, p<0.01). African-Americans and Asians were the most likely to have no HLA matches (42.2 and 41.3%, respectively) versus Caucasians and Hispanic recipients (31.1% and 32.2%, respectively, p<0.01). Median graft survival was lowest for African-Americans (7.8yrs, 95% C.I. 6.8-8.8), while Caucasians, Hispanics and Asians had similar median graft survival (15.1yrs, 17.1 and 15.6, respectively), the shorter graft survival for African-Americans met statistical significance (p<0.01, log rank).
Discussion
This represents the first report to specifically investigate the association between HLA donor-recipient matching utilizing a multi-institutional database in pediatric heart transplant patients. We found an association between improved survival and a higher degree of donor-recipient HLA matching. The reason for improved graft survival with increased HLA matching in pediatric heart transplantation is an area that needs further study. Early reports in adult heart transplantation, reported that HLA matching decreased the frequency of rejection as well as the incidence of steroid resistant rejection.13 More recent studies have found that HLA matching is associated with a lower incidence of rejection within the first year for adult heart transplant recipients.5, 14 However, the present study did not find a difference in the rate of rejection in the first year related to degree of HLA matching. The fact that HLA matching was not associated with improved graft survival in infants indicates a possible immunological etiology for the improved graft survival. Due to an immature and developing immune systems, infants are more likely to develop graft “tolerance” and less likely to mount a strong immunological response to the transplanted graft.15 However, determining the exact mechanism that of how donor-recipient matching leads to improved outcomes is important as it could lead to targeted therapies post-transplant in patients with low degree or no HLA matching. This is most likely to be accomplished by linking multiple pediatric heart transplantation databases.
HLA matching has been associated with improved outcomes in adult heart transplantation. However, the impact of HLA matching on graft survival appears to be stronger in the adult population compared to our results of a completely pediatric population.4, 14 Possible explanations to why there is a difference between age groups, include differences in development of the immune system as well as influence of other factor such as medical adherence. In the infant population, HLA matching was not associated with graft survival likely due to the infant's immature immune system and the development of graft “tolerance”. Also, the relatively high rate of medical non-adherence seen in adolescence is known to lead to increased risk of graft loss and therefore will decrease the impact of HLA matching on graft survival.16
The importance of matching at different HLA loci has been extensively researched in pediatric kidney transplantation. HLA-DR matching has been associated with improved graft survival and lower incidence of lymphoma.17-19 HLA-DR matching has been suggested to improve outcomes in adult heart transplant recipients.14 The current study suggests that matching at the B locus is independently associated with improved survival, however the hazard ratio 95% confidence interval which approached 1, while matching at the A and DR locus were associated with improved graft survival in univariate analysis. These results suggest that the number of total matches should be given more influence than matching at an individual locus. Our study included typing of HLA-A, B, and DR loci as these loci were routinely typed during the entirety of our study. Typing of the HLA-DQ and C loci is now routine. Therefore over time, more data will be available to analyze the effects of matching at these loci in pediatric heart transplantation.
We did not find an association between HLA matching and the development of coronary vasculopathy. This is in contrast to findings in adult heart transplantation in which a higher degree of HLA matching has been reported to be associated with lower incidence of transplant coronary vasculopathy.14 Coronary vasculopathy is a time dependent process, with steadily increasing incidence as time from transplantation increases. In our analysis, the HLA matching groups had similar years of transplant, and therefore similar time to develop coronary vasculopathy as well as similar recipient age, a known risk factor for coronary vasculopathy.20, 21 Our findings were consistent with another report on pediatric heart transplantation from a multi-institutional database which did not find a link between HLA matching and coronary vasculopathy.21 In kidney transplantation, HLA matching, specifically matching at the B-locus has been associated with decreasing rates of post-transplant lymphoproliferative disease.22 The exact mechanism that lead to the improved graft survival through HLA matching in the pediatric heart transplant population could not be determined with the available database. Elucidating the protective mechanism of HLA matching on graft survival should be the subject of further investigations as this knowledge could help guide diagnostic and therapeutic interventions in patients with a high degree of HLA mismatching.
HLA matching is currently not a factor in heart transplant donor allocation. Authors of previous reports have argued that HLA matching should be considered in cardiac donor allocation due to improved outcomes.14 HLA matching has been used in organ allocation in kidney transplantation.23 However, after decreasing the importance of HLA matching in Canada and the UK, reports have indicated decreased waitlist times.23, 24 While pediatric heart transplant waitlist mortality has decreased over the past 20 years, it still remains elevated at 13%.25 Other considerations in donor allocation, such a donor-recipient size, ischemic time, surgical complexity, and rising rates of HLA sensitization in listed patients, make adding HLA matching to donor allocation algorithms very difficult. Based upon the kidney transplant data, addition of HLA matching could possibly lead to increased waitlist mortality.23, 24 Therefore, prior to any consideration of HLA matching in pediatric heart transplant donor allocation, effects of waitlist time and mortality must be evaluated.
The higher degree of HLA matching seen when donors and recipients were of the same race is not surprising as HLA haplotypes are often conserved within racial groups.26 Donor-recipient race matching has been associated with increased graft survival in all races in pediatric heart transplantation.27 The graft survival associated with donor:recipient race matching is likely due to increasing degree of HLA matching when donor and recipient race are the same.
The reason that African-Americans and Asians were more likely to have no HLA matches compared to Caucasians and Hispanics is due to an interaction between race of donors as well as shared haplotypes between races. Caucasian and Hispanics made up the largest two racial categories of donors, 79.5% of donors when combined. Also, HLA haplotypes that are commonly found in Caucasian and Hispanics in the United States are frequently seen in other racial groups.26 However, this is not true for Asians and African-Americans, common HLA haplotypes in these populations are rarely found in other populations.26 Therefore, less donors of the same race and decrease change of having a HLA match from another race leads Asians and African-Americans being more likely to receive a heart without HLA matching. African-Americans being more likely to have no HLA matches and the fact the HLA-no group had the shortest graft survival provides a possible reason that previously reported graft survival is worse for African-Americans even after controlling for socioeconomic status.12
Limitations
The influence on HLA matching in donor evaluation by transplant centers is not known, therefore, the distribution of HLA matching may not represent actual random chance but be influenced by decision making processes not accounted for. There was no set definition of transplant coronary vasculopathy or rejection within the first year and therefore reporting of this information was solely left to the discrimination of the reporting institution. The methods and frequency of surveillance for transplant coronary vasculopathy are not known and could have varied greatly between institutions influencing the reporting of coronary vasculopathy. The database is dependent upon accurate reporting from participating institutions. The type of rejection, cellular versus antibody-mediated versus mixed, was not reported in the database and therefore limited the authors’ ability to discern associations between HLA matching and frequency of specific types of rejection, such as antibody-mediated rejection. A lack of consistent late reporting of rejection in the database prevented the authors from assessing associations between HLA matching and late rejection.
Conclusion
A greater degree of HLA donor-recipient (3 or more matches) occurs relatively infrequently in pediatric heart transplants, but is associated with improved graft survival. This information can help the transplant team identify patients who are higher risk for graft loss. Further studies into the etiology of HLA matching's association with improved graft survival will help the transplant team tailor therapeutics to transplant with low or no HLA matching.
Supplementary Material
Acknowledgments
Sources of Funding
This work was supported in part by Health Resources and Services Administration contract 234-2005-370011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. Data represented is based on OPTN data as of December 31, 2012. This work was supported by NRSA Grant 5T32-HL07710-17 (author: RB)
Footnotes
Disclosures
None.
References
- 1.Stehlik J, Islam N, Hurst D, Kfoury AG, Movsesian MA, Fuller A, Delgado JC, Hammond ME, Gilbert EM, Renlund DG, Bader F, Fisher PW, Bull DA, Singhal AK, Eckels DD. Utility of virtual crossmatch in sensitized patients awaiting heart transplantation. J Heart Lung Transplant. 2009;28:1129–1134. doi: 10.1016/j.healun.2009.05.031. [DOI] [PubMed] [Google Scholar]
- 2.Feingold B, Park SY, Comer DM, Moore CG, Webber SA, Bryce CL. Outcomes after listing with a requirement for a prospective crossmatch in pediatric heart transplantation. J Heart Lung Transplant. 2013;32:56–62. doi: 10.1016/j.healun.2012.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Opelz G. The effect of tolerance to noninherited maternal hla antigens on the survival of renal transplants from sibling donors. N Engl J Med. 1999;340:1369–1370. doi: 10.1056/NEJM199904293401715. [DOI] [PubMed] [Google Scholar]
- 4.Opelz G, Wujciak T. The influence of hla compatibility on graft survival after heart transplantation. The collaborative transplant study. N Engl J Med. 1994;330:816–819. doi: 10.1056/NEJM199403243301203. [DOI] [PubMed] [Google Scholar]
- 5.Kilic A, Weiss ES, Allen JG, Conte JV, Shah AS, Baumgartner WA, Yuh DD. Simple score to assess the risk of rejection after orthotopic heart transplantation. Circulation. 2012;125:3013–3021. doi: 10.1161/CIRCULATIONAHA.111.066431. [DOI] [PubMed] [Google Scholar]
- 6.Kaczmarek I, Deutsch MA, Rohrer ME, Beiras-Fernandez A, Groetzner J, Daebritz S, Schmoeckel M, Spannagl M, Meiser B, Reichart B. Hla-dr matching improves survival after heart transplantation: Is it time to change allocation policies? J Heart Lung Transplant. 2006;25:1057–1062. doi: 10.1016/j.healun.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Tenderich G, Zittermann A, Prohaska W, Koerfer R. No evidence for an improvement of long-term survival by hla matching in heart transplant recipients. Transplant Proc. 2007;39:1575–1579. doi: 10.1016/j.transproceed.2007.01.083. [DOI] [PubMed] [Google Scholar]
- 8.Almenar L, Maeso ML, Martinez-Dolz L, Rueda J, Palomar CG, Saez AO, Vives MA, Tort MD, Perez MP. Influence of hla matching on survival in heart transplantation. Transplant Proc. 2005;37:4001–4005. doi: 10.1016/j.transproceed.2005.09.145. [DOI] [PubMed] [Google Scholar]
- 9.Alonso de Begona J, Gundry SR, Nehlsen-Cannarella SL, Fullerton DA, Kawauchi M, Razzouk AJ, Vigesaa R, Kanakriyeh M, Boucek M, Bailey LL. Hla matching and its effect on infant and pediatric cardiac graft survival. The loma linda pediatric cardiac transplant team. Transplant Proc. 1991;23:1139–1141. [PubMed] [Google Scholar]
- 10.Benden C, Edwards LB, Kucheryavaya AY, Christie JD, Dipchand AI, Dobbels F, Kirk R, Rahmel AO, Stehlik J, Hertz MI, International Society of H, Lung T. The registry of the international society for heart and lung transplantation: Fifteenth pediatric lung and heart-lung transplantation report--2012. J Heart Lung Transplant. 2012;31:1087–1095. doi: 10.1016/j.healun.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Dipchand AI, Kirk R, Edwards LB, Kucheryavaya AY, Benden C, Christie JD, Dobbels F, Lund LH, Rahmel AO, Yusen RD, Stehlik J, International Society for H, Lung T. The registry of the international society for heart and lung transplantation: Sixteenth official pediatric heart transplantation report-2013; focus theme: Age. J Heart Lung Transplant. 2013;32:979–988. doi: 10.1016/j.healun.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Mahle WT, Kanter KR, Vincent RN. Disparities in outcome for black patients after pediatric heart transplantation. J Pediatr. 2005;147:739–743. doi: 10.1016/j.jpeds.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 13.DiSesa VJ, Kuo PC, Horvath KA, Mudge GH, Collins JJ, Jr., Cohn LH. Hla histocompatibility affects cardiac transplant rejection and may provide one basis for organ allocation. Ann Thorac Surg. 1990;49:220–223. doi: 10.1016/0003-4975(90)90141-r. discussion 223-224. [DOI] [PubMed] [Google Scholar]
- 14.Kaczmarek I, Deutsch MA, Rohrer ME, Beiras-Fernandez A, Groetzner J, Daebritz S, Schmoeckel M, Spannagl M, Meiser B, Reichart B. Hla-dr matching improves survival after heart transplantation: Is it time to change allocation policies? J Heart Lung Transplant. 2006;25:1057–1062. doi: 10.1016/j.healun.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Urschel S, Campbell PM, Meyer SR, Larsen IM, Nuebel J, Birnbaum J, Netz H, Tinckam K, Kauke T, Derkatz K, Coe JY, Platt JL, West LJ. Absence of donor-specific anti-hla antibodies after abo-incompatible heart transplantation in infancy: Altered immunity or age? American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2010;10:149–156. doi: 10.1111/j.1600-6143.2009.02877.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oliva M, Singh TP, Gauvreau K, Vanderpluym CJ, Bastardi HJ, Almond CS. Impact of medication non-adherence on survival after pediatric heart transplantation in the u.S.A. J Heart Lung Transplant. 2013;32:881–888. doi: 10.1016/j.healun.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 17.Opelz G, Dohler B. Pediatric kidney transplantation: Analysis of donor age, hla match, and posttransplant non-hodgkin lymphoma: A collaborative transplant study report. Transplantation. 2010;90:292–297. doi: 10.1097/TP.0b013e3181e46a22. [DOI] [PubMed] [Google Scholar]
- 18.Barocci S, Valente U, Gusmano R, Torre F, Basile G, Fontana I, Arcuri V, Olmi F, Angelini G, Nocera A. Hla matching in pediatric recipients of a first kidney graft. A single center analysis. Transplantation. 1996;61:151–154. doi: 10.1097/00007890-199601150-00029. [DOI] [PubMed] [Google Scholar]
- 19.Gralla J, Tong S, Wiseman AC. The impact of human leukocyte antigen mismatching on sensitization rates and subsequent retransplantation after first graft failure in pediatric renal transplant recipients. Transplantation. 2013;95:1218–1224. doi: 10.1097/TP.0b013e318288ca14. [DOI] [PubMed] [Google Scholar]
- 20.Pahl E, Naftel DC, Kuhn MA, Shaddy RE, Morrow WR, Canter CE, Kirklin J, Pediatric Heart Transplant S. The impact and outcome of transplant coronary artery disease in a pediatric population: A 9-year multi-institutional study. J Heart Lung Transplant. 2005;24:645–651. doi: 10.1016/j.healun.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 21.Kobayashi D, Du W, L'Ecuyer T J. Predictors of cardiac allograft vasculopathy in pediatric heart transplant recipients. Pediatric transplantation. 2013;17:436–440. doi: 10.1111/petr.12095. [DOI] [PubMed] [Google Scholar]
- 22.Bakker NA, van Imhoff GW, Verschuuren EA, van Son WJ, van der Heide JJ, Lems SP, Veeger NJ, Kluin PM, Kluin-Nelemans HC, Hepkema BG. Hla antigens and post renal transplant lymphoproliferative disease: Hla-b matching is critical. Transplantation. 2005;80:595–599. doi: 10.1097/01.tp.0000173793.03228.bd. [DOI] [PubMed] [Google Scholar]
- 23.Crafter SR, Bell L, Foster BJ. Balancing organ quality, hla-matching, and waiting times: Impact of a pediatric priority allocation policy for deceased donor kidneys in quebec. Transplantation. 2007;83:1411–1415. doi: 10.1097/01.tp.0000266580.19614.f7. [DOI] [PubMed] [Google Scholar]
- 24.Johnson RJ, Fuggle SV, Mumford L, Bradley JA, Forsythe JL, Rudge CJ. Kidney Advisory Group of NHSB, Transplant. A new uk 2006 national kidney allocation scheme for deceased heart-beating donor kidneys. Transplantation. 2010;89:387–394. doi: 10.1097/TP.0b013e3181c9029d. [DOI] [PubMed] [Google Scholar]
- 25.Singh TP, Almond CS, Piercey G, Gauvreau K. Trends in wait-list mortality in children listed for heart transplantation in the united states: Era effect across racial/ethnic groups. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2011;11:2692–2699. doi: 10.1111/j.1600-6143.2011.03723.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maiers M, Gragert L, Klitz W. High-resolution hla alleles and haplotypes in the united states population. Hum Immunol. 2007;68:779–788. doi: 10.1016/j.humimm.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 27.Kanter KR, Berg AM, Mahle WT, Vincent RN, Kilgo PD, Kogon BE, Kirshbom PM. Donor-recipient race mismatch and graft survival after pediatric heart transplantation. Ann Thorac Surg. 2009;87:204–209. doi: 10.1016/j.athoracsur.2008.09.074. discussion 209-210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


