Abstract
Background and Objectives
Research shows that interventions for substance use disorders may be helpful in reducing internalizing disorders in adolescents. This paper examines the prevalence and reductions of anxiety and depression symptoms among youth receiving substance use treatment.
Methods
Four hundred eighty adolescents ages 12–17 who received treatment for substance abuse as part of the Brief Strategic Family Therapy effectiveness trial were screened for anxiety and depression using the Diagnostic Interview Schedule for Children-Predictive Scales (DISC-PS). Twelve-month post-randomization assessments were completed by 327 parents and 315 youth. Sixty-five percent of the sample was found to have probability of at least one anxiety disorder or depression diagnosis.
Results
Significant reduction of anxiety and depressive symptoms and significant reductions in probable anxiety and depression diagnoses were observed at follow-up. Few differences by treatment type and by ethnic group were noticed.
Conclusions and Scientific Significance
Findings indicate that substance use interventions might help reduce the prevalence of anxiety and depressive symptoms and the probability of these disorders.
INTRODUCTION
Adolescent drug abuse continues to represent one of the most pressing public health issues in the United States.1 According to the National Survey on Drug Use and Health, drug use increased by 9% in 2009, reversing downward trends since 2002.2 Without effective treatments, these adolescents are at increased risk for serious medical and legal problems, incarceration, suicide, school difficulties, unemployment, and poor interpersonal relationships.3–5 While effective interventions for youth substance use disorders (SUDs) exist,6 substance using adolescents are likely to experience both immediate and long-term emotional and physical consequences. In particular, as many as 75% of adolescents with SUDs have some additional form of mental health problem (eg, conduct disorder, depression)5,7–10 and in most clinical samples psychiatric comorbidity is more common than SUD alone.11,12 In addition, substance using youth with comorbid disorders start using earlier and experience more severe social and family dysfunction, lower levels of commitment to school, more legal problems, suicidal behavior, sexual, or physical abuse, have parents who use drugs and have serious mental health problems.11–13
Externalizing problems such as Conduct Disorder, ADHD, and Oppositional Defiant Disorder (ODD) are the most commonly reported and investigated comorbid disorders with SUD, but internalizing problems such as anxiety disorders and major depression and SUD are also common.14 For example, the research literature reveals current prevalence rates of depression with substance using disorders ranging from 11% to 32% and anxiety disorders with substance using disorders ranging from 7% to 40%.13,15 While there are proven effective treatments for depression and anxiety in adolescents,16,17 and there is both clinical and empirical evidence that supports integrating substance abuse treatment and comorbid disorders;15 unfortunately, there are well-documented barriers to the delivery of integrated treatment.5 Moreover, existing studies have not yet been able to address the separate and combined influences of pharmacotherapy and behavioral interventions for comorbid psychiatric and SUDs.18
Several models have been proposed for the development of co-occurring mental health and SUD in adolescence, inevitably attempting to find a causal relationship between them.19–21 Reviews of these describe: (a) common factor development in which shared common factors predispose adolescents to both mental health problems and SUDs; (b) secondary SUDs; (c) secondary mental/psychiatric disorder; and (d) bidirectional models. Therefore, it is possible that interventions for one disorder may help reduce the incidence of the other disorder, either by changing a common risk factor (family environment) or via reduction of a maintaining disorder (anxiety fostering substance abuse). In fact, the effects of depression treatment carry over to anxiety symptoms22 and treatment of psychiatric comorbidity often helps to alleviate the SUD as well.23 A theoretical basis for the possibility of effects on anxiety and depression via substance abuse intervention is derived from a number of hypotheses. These hypotheses generally stress the reciprocal relation between a number of child, parental/ familial, and environmental factors. For example, interventions for substance abuse may foster positive perceptions of self efficacy (a protective mechanism for both anxiety and depression) directly by fostering positive self-perceptions and perceptions of personal success.24 Family therapy can shape a positive parental attitude, which in turn may be a powerful contributor to self-worth in childhood/adolescence and could target many of the family risk factors for youth depression.25,26 It is also possible that interventions for these psychiatric disorders such as depression and anxiety and SUDs target similar mechanisms of behavior change through common components of treatment.26,27
Research is needed to examine if interventions for SUDs may help reduce the incidence of comorbid internalizing disorders. Whereas there are a relatively large number of studies on the impact of psychiatric comorbidity on substance abuse treatment outcomes, to date only few studies11,28–31 have examined the effects of substance use treatment on anxiety disorders and depression in youth. While these studies have shown a reduction in such symptoms, they have several limitations: (1) with a few exceptions (ie, n = 88;32 n = 11431) they have studied a relatively small sample size (eg, n = 32;28,29 n = 5630); (2) have been implemented as one site efficacy studies; (3) have reported the internalizing disorders as part of other comorbid disorders;11,33,34 and (4) have presented findings mostly on youth who are involved in juvenile justice and are mainly male and African American33,34 or Hispanic.31,32 The purpose of this article is to build on the existing literature by examining the reductions in anxiety and depression symptoms in drug using adolescents receiving substance abuse treatment in a multi-site randomized study conducted in eight community treatment agencies. This article is a secondary analysis of the Brief Strategic Family Therapy (BSFT) effectiveness study, main study design and results have been presented by Robbins et al.35,36
Adolescents randomly received either Treatment As Usual (TAU) or a family intervention, BSFT. For this secondary analysis, we first hypothesized that anxiety and depression would be highly prevalent in the sample. We next hypothesized that drug abuse treatment (both BSFT and TAU) would have a significant impact in reducing anxiety and depression levels and in reducing the prevalence of probable anxiety and depression diagnoses, and that these changes would be greatest in BSFT. We expected effect sizes greater than those that might be expected on the basis of normal reductions in symptoms over time;37 but smaller than those typically found in childhood anxiety disorder treatment studies. 38,39 Given the established impact of BSFT in parenting and family functioning, and potential benefits that these could bring on anxiety and depression symptoms, we expected differential effects for BSFT versus TAU. The BSFT effectiveness study used ethnicity as a variable for randomization, and was designed to maximize the chance that a sufficient number of Hispanic and African American adolescents would be included to allow valid subgroup comparisons40. Therefore, the design of the main study allows us to explore the effects of ethnicity as moderators of change as part of this secondary analysis. In addition, because cases got additional services beyond drug abuse treatment, we also examined the potential effects of outside treatment and the amount of intervention received.
MATERIALS AND METHODS
Participants and Design
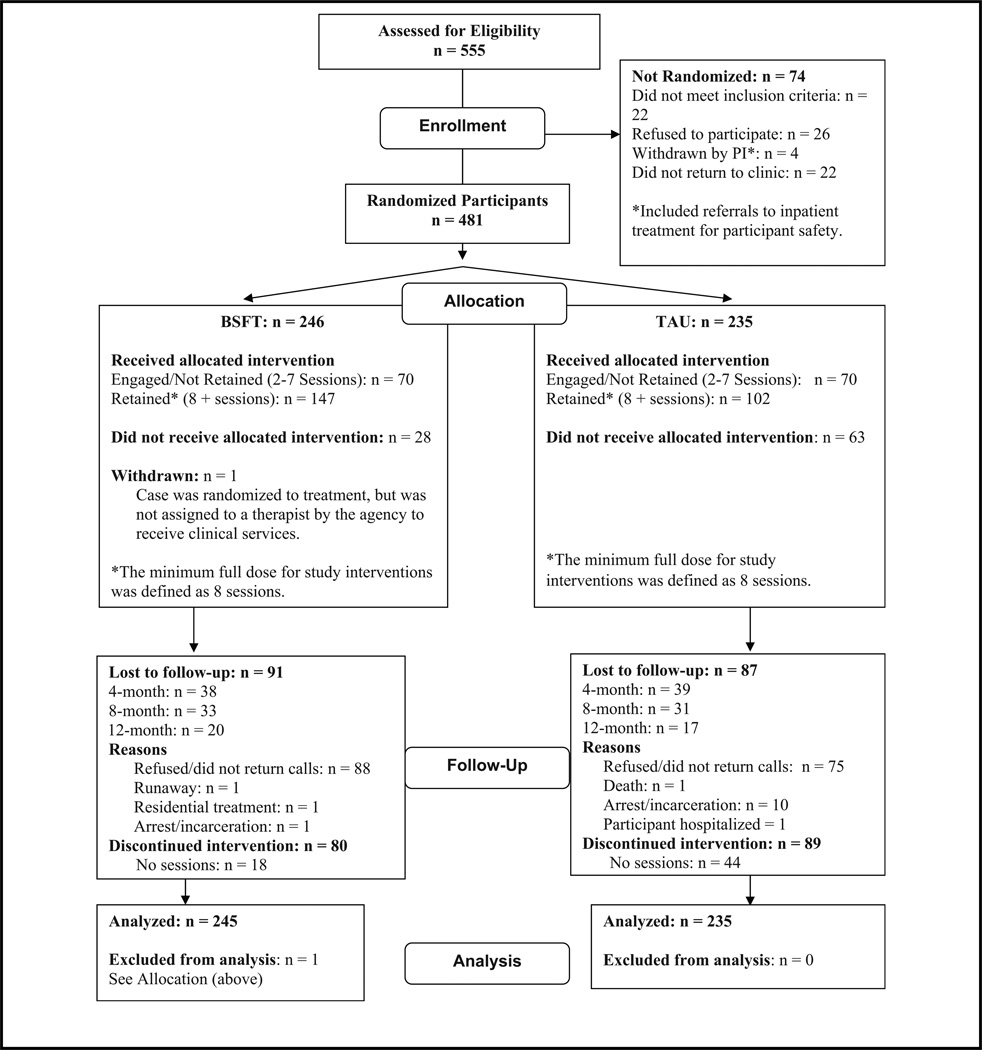
This article uses data from the BSFT effectiveness study conducted in the NIDA’s National Drug Abuse Treatment Clinical Trials Network.35 The BSFT effectiveness study utilized a prospective, longitudinal, randomized design. Four-hundred eighty adolescents and their families were randomly assigned to BSFT or TAU for the treatment of drug abuse in eight outpatient community treatment centers (CTPs) across the country. Figure 1 presents a consort flow diagram for the BSFT effectiveness study. To enroll in the study, adolescent participants had to self-report illicit drugs (other than alcohol and tobacco) in the 30-day period that preceded the baseline assessment or were referred from an institution (eg, detention, residential treatment, court, etc.) for the treatment of substance abuse. Also, the adolescent had to assent and a parent or legal guardian had to consent to participate in therapy.
FIGURE 1.
Consort flow diagram for BSFT effectiveness study.
After providing consent/assent for their participation, adolescents and their families in both conditions were asked to participate in follow-up assessments for a period of 12 months following randomization. Youth and parents were screened for comorbid psychiatric diagnoses pre-treatment (Time 1) and again at 12 months (Time 2).
The sample was aged 12–17 years (mean age 15.4 years) and was 78.5% male. Ethnic composition was as 44% Hispanic (n = 213), 31% White (n = 148), 23% African American (n = 110), and 2% (n = 9) youth were of other ethnicities. Seventy-two percent were referred to treatment by the court. Sixty-nine percent met diagnostic criteria for any substance abuse or dependence by the Diagnostic Interview Schedule for Children-Substance Abuse (DISC SA).
A total of 327 primary guardians and 315 youth completed the 12-month anxiety and depression assessment. Comparison of the youth who completed both the Time 1 and Time 2 assessments versus the youth who only completed the Time 1 assessment revealed no statistically significant differences on child age, gender, child reported anxiety, child reported depression, and parent reported depression. The only significant differences were for ethnicity and parent reported anxiety. Specifically, the youth lost to attrition had relatively lower Time 1 parent reported anxiety, and relatively more African Americans were lost to attrition.
Measures
The Diagnostic Interview Schedule for Children-Predictive Scales (DISC-PS41) was used to assess anxiety and depression symptoms and to identify probable presence of Simple Phobia, Social Phobia, Agoraphobia, Panic Disorder, Separation Anxiety Disorder, Generalized Anxiety Disorder, Obsessive-Compulsive Disorder, and Major Depressive Disorder based on DSM IV criteria. This measure was administered to both youth and parents to assess the adolescent’s psychiatric symptoms and probability of psychiatric diagnoses in the past 12 months. This instrument has demonstrated excellent sensitivity and specificity compared to the full Diagnostic Interview Schedule for Children.41 Reported test–retest reliabilities of the scales are generally good and had intraclass correlation coefficients ranging from .52 for obsessive-compulsive disorder to .82 for conduct disorder. For this article, we created six continuous scales from the symptom items [ie, anxiety symptoms reported by the child (34 items, in this sample coefficient alpha was .85 Time 1 and .84 Time 2) and the parent (36 items, in this sample coefficient alpha was .86 Time 1 and .89 Time 2); depressive symptoms reported by the child (7 items, in this sample coefficient alpha was .72 Time 1 and .76 Time 2) and parent (9 items, in this sample coefficient alpha was .78 Time 1 and .82 Time 2)] as well as externalizing symptoms (Conduct Disorder, ODD, and ADHD) reported by the child (21 items, in this sample coefficient alpha was .82 Time 1 and .87 Time 2) and parent (38 items, in this sample coefficient alpha was .91 Time 1 and .94 Time 2). These six continuous scales created for this analysis were used to examine reductions in anxiety and depressive symptoms. We also examined probability of diagnoses based on the symptoms criteria reported in Lucas et al.41 and exclusionary criteria in the interview. We used the most stringent cutoffs reported for each diagnoses. For example, diagnosis was met if child participants endorsed more than one symptom for Simple Phobia, more than one for Social Phobia, more than three for Generalized Anxiety Disorder, more than four for Major Depressive Disorder, or more than two for Conduct Disorder. Additional details on the symptom criteria can be found in Tables 1–3 of Lucas et al.41
TABLE 1.
Means, standard deviations, and estimates of effect size for anxiety and depression symptoms at pre- and post-treatment
| Pre | Post | |||
|---|---|---|---|---|
| M (SD), Min–Max scores | M (SD), Min–Max scores | t | d | |
| Anxiety child BSFT | 5.64 (4.9), 0–25 | 3.88 (4.2), 0–21 | 5.08*** | .40 |
| Anxiety child TAU | 5.61 (5.1), 0–26 | 3.48 (4.1), 0–22 | 6.85*** | .56 |
| Depression child BSFT | 2.32 (1.8), 0–7 | 1.86 (1.8), 0–7 | 3.09** | .24 |
| Depression child TAU | 2.13 (1.9), 0–7 | 1.64 (1.8), 0–6 | 3.40** | .28 |
| Anxiety parent BSFT | 5.40 (4.9), 0–21 | 4.88 (6.1), 0–29 | 3.76*** | .29 |
| Anxiety parent TAU | 5.90 (4.7), 0–20 | 3.48 (3.7), 0–27 | 7.52*** | .60 |
| Depression parent BSFT | 3.73 (2.4), 0–9 | 2.79 (2.6), 0–9 | 5.01*** | .39 |
| Depression parent TAU | 3.77 (2.3), 0–9 | 2.58 (2.4), 0–8 | 6.25*** | .49 |
Means reported are non-transformed; inferential statistics and effect sizes are computed from transformed parent and child anxiety. BSFT = Brief Strategic Family Therapy; TAU = Treatment As Usual.
p < .01
p < .001.
TABLE 3.
Change in anxiety and depression in youth without child reported comorbid externalizing diagnoses (n = 158)
| Mean change pre to post | Standard error | t | p-value | |
|---|---|---|---|---|
| Child reported anxiety | .07 | .02 | 4.21 | .000 |
| Parent reported anxiety | .07 | .01 | 4.97 | .000 |
| Child reported depression | .11 | .12 | .85 | .394 |
| Parent reported depression | .78 | .19 | 4.04 | .000 |
Interventions
Brief Strategic Family Therapy
BSFT is a manualized intervention42 that integrates structural and strategic theory and intervention techniques to address systemic (primarily family) interactions that are associated with adolescent substance use and related behavior problems. BSFT considers adolescent symptomatology to be rooted in maladaptive family interactions, inappropriate family alliances, overly rigid or permeable family boundaries, and parents’ tendency to believe that a single individual (usually the adolescent) is responsible for the family’s troubles. BSFT operates according to the assumption that transforming family interactions will help improve the youth’s presenting problem. The emphasis is on identifying the nature of the interactions in the family and changing those interactions that are maladaptive. BSFT consists of 12–16 sessions over a 4-month period, and up to 8 “booster” sessions. The actual number of sessions/ length of service is based on the therapist’s ability to achieve necessary improvements in specific behavioral criteria (eg, drug use and family interactions) and the severity of family problems. Therapists were permitted to conduct “booster sessions” after the 12–16 sessions with cases that relapse, present adverse events during follow-up assessments, or in response to a family petition. The majority of therapy sessions were expected to involve multiple family members. Services were planned to include a systematic assessment and plan for involving individuals from other relevant systems in which the adolescent is involved (eg, school, peer, justice). Finally, location of services was flexible to ensure that location was not an obstacle to the delivery of BSFT interventions. As described by Nunes et al.,43 given that BSFT is a comprehensive stand alone intervention for drug-abusing adolescents, it was suited to be tested against TAU, where TAU in this design was substituted entirely by the BSFT.
Treatment as Usual
TAU varied depending on the treatment programs at participating CTPs. TAU in CTPs included one or more of the following: individual and/or group therapy, parent training groups, non-manualized family therapy, and case management. At least 1 intervention session per week was typical, as well as participation in ancillary services (eg, case management, AA, etc.). However, CTPs providing weekly, manualized family therapy sessions were excluded. A prerequisite for participation in this protocol was that the community agency’s TAU had to minimally include at least 12–16 scheduled sessions to ensure that differences in dose between BSFT and TAU were not the result of different planned treatment parameters.
Therapy Dose
Dose in both conditions was tracked through monthly therapists’ interviews. Using the participant’s clinical charts, therapists in both conditions reported on the clinical status of cases, recommended dose, and the number of sessions that were actually delivered during the past month (or since last interview). During these interviews, in addition to the study intervention dose, the therapists reported on additional treatment services (therapy sessions) that their assigned cases received. Total dose was constructed as the sum of all therapy sessions conducted by any therapist (not just the study-therapist) at the agency, thus allowing us to track delivery of psychiatric services. It should be noted that the mean expected dose in both conditions in the BSFT effectiveness study ended up being higher than anticipated because the average length of treatment was much longer than expected (approximately 8 months).
Data Analyses
Preliminary and comorbidity pattern analyses were conducted with descriptive statistics, cross tabulations, and chi-square analyses. Formal tests of the effects of the intervention were conducted using a set of 2 (treatment group; BSFT vs. TAU) by 2 (time; pre to 12-month follow-up) mixed factorial ANOVA’s. In this type of analysis, the critical effect expected is a significant effect of time and a significant interaction effect to demonstrate differential effect of the type of treatment (or effect of other moderators) and significant effect of time to demonstrate a decrease in symptoms. Significant interactions were decomposed with single degree of freedom contrasts as recommended by Jaccard and Guilamo-Ramos.44
We also examined the size of changes within each treatment group. The parent and child were considered families of analysis and so the alpha was set at (p < .025). Cohen’s d was used to estimate effect size. Based on expected effect sizes (d between .2 and .6) power was well above .8045 for these analyses even with the attrition from Time 1 to Time 2. Given significant reductions in symptoms using the continuous measure, we examined the clinical significance of the findings by examining reduction in the prevalence of probable diagnoses using the DISC predictive scales for the various anxiety disorders and major depression. Reductions in the prevalence of probable anxiety and depression diagnosis were examined using the binomial test and tested change in prevalence for disorders with greater than a 5% initial (Time 1) prevalence estimate. Analyses were also conducted to examine whether change in anxiety and depression symptoms would still be evident among youth without comorbid externalizing disorders by conducting a set of 2 (treatment group; BSFT vs. TAU) by 2 (time; pre to 12-month follow-up) mixed factorial ANOVA’s to examine change in pre- to post-treatment among only youth without comorbid externalizing disorders based on child report (based on parent report the sample was too small).
RESULTS
Preliminary and Descriptive Analyses
Examination of the anxiety and depression scores’ ranges and skew indicated acceptable levels for the planned analyses for the depression and externalizing scales but significant skew on anxiety symptoms (child skew = 1.47; parent skew = 1.15). Square root transformation normalized the distribution (child skew = .06; parent skew = −.02) and one outlier for child reported anxiety and one outlier for parent reported anxiety were removed before conducting the main analyses.
Anxiety and depression diagnoses were highly prevalent in the sample. Fifty-two percent of the sample had at least probability of one anxiety or depression disorder in the past 12 months by child report and 65% by parent report. Forty-one percent had probability of depression according to parent report (of these 73% had at least one comorbid anxiety disorder), and 26% had probable depression via child report (of these 67% had at least one comorbid anxiety disorder). Fifty-four percent had at least one probable anxiety disorder by parent report and 32% had at least two probable anxiety disorders. Specific parent reported anxiety disorders included Social Anxiety Disorder (32.5%), Generalized Anxiety Disorder (29.8%), Separation Anxiety Disorder (20.4%), Specific Phobia (14.8%), Panic (14.4%), Obsessive Compulsive Disorder (.6%), and Agoraphobia (.4%). Forty-four percent of the sample had at least one anxiety disorder by child report and 17% had at least two anxiety disorders. Specific child reported anxiety disorders included Specific Phobia (24.6%), Social Anxiety Disorder (18.3%), Separation Anxiety Disorder (14.6%), Panic (7.9%), Obsessive Compulsive Disorder (3.1%), Agoraphobia (2.1%), and Generalized Anxiety Disorder (2.1%).
Effect of the Intervention on Continuous Symptom Scores
Results of the intervention (pre- to post-treatment) were first analyzed with repeated measures ANOVAs [two time (ie, the repeated measures factor) by two treatment (BSFT vs. TAU a between subjects factor)] or mixed factorial ANOVAs. Table 1 presents pre- and post-treatment means by type of treatment with Cohen’s d effect size estimates for anxiety and depression. Results on child reported depression indicated a significant effect of time [F(1, 313) = 22.01,p < .001] but no significant treatment group × time interaction [F(1, 313) = .08,p > .1]. Results on parent reported depression indicated a significant effect of time [F(1, 325) = 63.35,p < .001] but no significant treatment × time interaction [F(1, 325) = .87, p > .1]. Results on child reported anxiety indicated a significant effect of time [F(1, 313) = 70.09, p < .001] but no significant treatment group × time interaction [F(1, 313) = 1.26, p > .1]. There were no significant between treatment group effects in any of these analyses. Results on parent reported anxiety indicated a significant effect of time [F(1, 325) = 63.45, p < .001], and a significant treatment group × time interaction [F(1, 325) = 6.98, p < .01] but no between subjects effect [F(1, 325) = .09, p > .1]. Follow-up paired samples t-tests indicated significant decreases in parent reported anxiety for both groups [BSFT t(168) = 3.76, p <.001, d = .29; TAU t(157) = 7.52, p < .001, d = .60], so the nature of the interaction can be understood by the larger effect size in TAU. Effect sizes for each of the measures reported in Table 1 indicate small to medium sized effects.
Additional analyses were run to test the effects of age, ethnicity, and sex. Because the reduction of symptoms could have been explained by differences in services by condition to target anxiety and depression, we ran additional models to test the effects of the additional outside intervention/services. Results indicated no differential effects based on age, sex, amount of treatment sessions, nor did these variables interact with treatment type. Amount of outside treatment was not a significant covariate and did not predict change in symptoms.
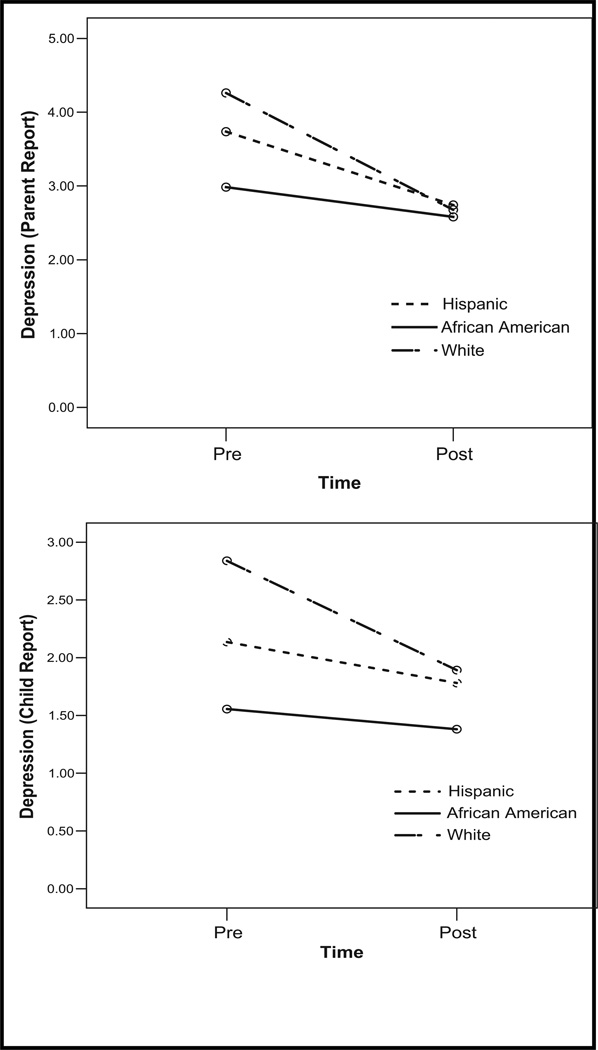
There were significant effects of ethnicity. These analyses were conducted excluding the youth classified as “other” due to the small sample size. Results indicated that there were significant ethnicity by time interactions for child reported depression [F(2, 308) = 4.43, p < .025]; child reported anxiety [F(2, 308) = 3.15, p < .05]; and parent reported depression [F(2, 318) = 4.81, p < .01]. Follow-up tests decomposed the significant interactions and are reported in Table 2. Pre- to post-changes for each ethnic group were tested with simple t-tests on change and differences between ethnic groups were tested with ANOVAs followed by single degree of freedom Bonferroni corrected comparisons. In general, the pattern of findings indicated that there were significant differences in pre-treatment depression and smaller and less consistent effects for non-white youth. These were most evident for depressive symptoms where African American youth tended to start treatment with lower depression and show little decrease. The pattern of ethnicity findings is illustrated in Fig. 2 for parent and child report of depression symptoms.
TABLE 2.
Contrasts for the significant ethnicity by time interactions
| 95% Confidence interval |
|||||||
|---|---|---|---|---|---|---|---|
| Mean change pre to post | Standard error | Lower | Upper | t | p-value | ||
| Hispanic | Child reported anxiety | .07 | .01 | .04 | .10 | 5.18 | .000 |
| Child reported depression† | .36 | .14 | .08 | .64 | 2.53 | .012 | |
| Parent reported depression | .99 | .19 | .62 | 1.37 | 5.26 | .000 | |
| African American | Child reported anxiety | .10 | .03 | .03 | .16 | 3.06 | .003 |
| Child reported depression† | .15 | .21 | −.28 | .57 | .68 | .501 | |
| Parent reported depression* | .40 | .23 | −.06 | .87 | 1.73 | .088 | |
| White | Child reported anxiety | .14 | .02 | .09 | .18 | 5.55 | .000 |
| Child reported depression† | .93 | .20 | .53 | 1.34 | 4.63 | .000 | |
| Parent reported depression* | 1.58 | .26 | 1.06 | 2.11 | 6.02 | .000 | |
White significantly higher than African American Time 1
White significantly higher than African American and Hispanic Time 1.
FIGURE 2.
Illustration of the ethnicity by time interaction for depression.
One additional set of supplemental analyses were conducted to examine whether change in anxiety and depression symptoms would still be evident among youth without comorbid externalizing disorders (ie, change in anxiety and depression might simply be a function of change in externalizing problems). Externalizing diagnoses were also highly prevalent at baseline. Ninety-three percent had probability of at least one of conduct disorder (63%), ODD (89%) or ADHD (76%) by parent report and 56% had probability of at least two disorders. Since the DSM-IV (American Psychiatric Association, 1994) excludes ODD when Conduct Disorder (CD) is met, the prevalence of ODD diagnosis was 26%. Fifty percent had at least one of CD (24%), ODD (41%), or ADHD (13%) by child report and 22% had probability of at least two disorders. Again, since DSM-IV excludes ODD when CD is met, the prevalence of ODD diagnosis was 24%. Thus, we conducted analyses examining change in pre- to post-treatment among only youth without comorbid externalizing disorders based on child report (based on parent report the sample was too small). Results are presented in Table 3 —these indicate significant changes in both parent and child reported anxiety and parent reported depressive symptoms.
Changes in Diagnostic Status
Reductions in the prevalence of probable anxiety and depression diagnoses were examined using the binomial test on disorders with greater than a 5% Time 1 prevalence estimate. Test proportions were based on Time 1 prevalence for each specific disorder using only participants for which both Time 1 and Time 2 data were available. Given the multiple tests alpha was set at .01 and so p-values <.01 indicate a significant reduction in prevalence. In terms of parent reported disorders Time 2 incidence was for probable Major Depression (26%, p < .001), Social Anxiety Disorder (22%, p < .001), Generalized Anxiety Disorder (22%, p < .001), Separation Anxiety Disorder (16%, p = .002), Specific Phobia (10%, p = .01), Panic (13% p > .1). In terms of child reported disorders Time 2 incidence was for probable Major Depression (20%, p = .002), Specific Phobia (18%, p < .001), Social Anxiety Disorder (9.6%, p < .001), Separation Anxiety Disorder (8.6%, p =.002), Panic (4.5%, p = .018), Conduct Disorder (9%, p < .001).
DISCUSSION
This article makes a novel contribution to the literature by showing that community-based drug abuse treatments may help reduce the prevalence of anxiety and depression symptoms and probability of diagnoses among adolescents. Adolescents with comorbid substance use and mental health problems constitute a unique clinical population at a very high risk for comorbid problems into adulthood to the extent that it has become one of the most pressing issues in developing and testing effective interventions for drug abuse.12,46 Results of this study suggest that there were significant reductions in symptoms after treatment and the effect sizes were in the small to medium range, even when controlling for other services that these adolescents might have received for these problems. Moreover, results show significant reductions in the prevalence of probable diagnosis for Major Depression, Social Anxiety, and Separation Anxiety based on parent and child report. In addition, reductions were most significant for the white group. Findings suggest similar effects for BSFT and TAU; however, TAU was more effective in reducing parent reported anxiety, but not child. Many factors could account for this difference but the exact reason cannot be known.
Findings were consistent with previous research indicating that substance abuse treatments are effective in reducing internalizing symptoms.11,31,47 Estimated effect sizes based on the reported mean changes in Waldron et al.31 are of .53 (4-month post-treatment) and .63 (7-month post-treatment). However, this single site trial reflected mean changes for all internalizing disorders. Our study extends research in a number of ways. First, the design and data collection of this study (effectiveness trial) helps establish the generalizibility of the findings. This study included a large sample of adolescents (N = 480) and their families from a community treatment sample where both parent and adolescents reported for psychiatric comorbidity. In addition, randomization was balanced for ethnic groups, thus resulting in a sample with 44% Hispanic (n = 213), 31% White (n = 148), 23% African American (n = 110), and 2% (n = 9) youth were of other ethnicities. The sample also included 103 girls.
Certain limitations in this study need to be acknowledged. First, the study relied on a measure of probability of diagnoses, the Diagnostic Interview Schedule for Children-Predictive Scales (DISC PS). However, we were able to use both parent and adolescent reports on this measure. Second, the data were collected at only two time points; baseline and 12-month post-randomization, only allowing a pre–post examination. Third, this study did not include a randomized control group that received no intervention. However, the control group for this study (TAU), also improved. Fourth, family therapies, and in particular BSFT, have yet to be proven efficacious in the treatment of anxiety or depressive disorder in youth. However, Restifo and Bögels25 demonstrate that family factors at all levels of family systems play a role in youth depression. A systemic and structural model such as BSFT, targets all the family risk factors implied in the literature, as they are inherent to its conceptual model. Lastly, 34% of the sample was lost to follow-up. However, it is important to note that the comparison of the youth who completed both the Time 1 and Time 2 assessments versus the youth who only completed the Time 1 assessment revealed no statistically significant differences on child age, gender, and child reported anxiety, child reported depression, and parent reported depression.
The results of this study have important clinical implications. It evidences that both treatments for adolescent drug abuse reduce anxiety and depression symptoms and their probable diagnoses, therefore, suggesting that their scope of intervention is broader than the drug use and abuse. Future research needs to address the mechanisms that could explain the improvements observed. For BSFT, it is possible that these improvements could be related to improvements in family functioning, given that improvement in family functioning is the mechanism by which BSFT mediates its effects. However, there could be some other mechanisms involved that need to be explored. This article presents parent and child report of anxiety and depression separately, given that there are differences in their reports. However, both parent and children are largely agreeing on improvement. Further research will have to examine if there are changes in agreement as a function of treatment. Finally, future research should also take into account parental psychopathology as a context for the incidence and trajectories of internalizing disorders of drug abusing adolescents.
Acknowledgments
This work supported by grant U10 DA 13720 from the National Institutes of Health, Bethesda, MD, José Szapocznik, Principal Investigator, NCT00095303.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
REFERENCES
- 1.Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings. Bethesda, MD: National Institute on Drug Abuse; 2009. [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies, NSDUH Series H-36; 2010. HHS Publication No. SMA 09-4434. [Google Scholar]
- 3.Fergusson DM, Boden JM. Cannabis use and later life outcomes. Addiction. 2008;103:969–978. doi: 10.1111/j.1360-0443.2008.02221.x. [DOI] [PubMed] [Google Scholar]
- 4.Hair EC, Park MJ, Long TL, et al. Risky behaviors in late adolescence: Co-occurrence, predictors, and consequences. J Adolesc Health. 2009;45:253–261. doi: 10.1016/j.jadohealth.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Hawkins EH. A tale of two systems: Co-occurring mental health and substance abuse disorders treatment for adolescents. Annu Rev Psychol. 2009;60:197–227. doi: 10.1146/annurev.psych.60.110707.163456. [DOI] [PubMed] [Google Scholar]
- 6.Robbins MS, Mayorga CC, Mitrani VB, et al. Adolescent and parent alliances with therapists in brief strategic family therapy with drug-using hispanic adolescents. J Marital Fam Ther. 2008;34:316–328. doi: 10.1111/j.1752-0606.2008.00075.x. [DOI] [PubMed] [Google Scholar]
- 7.Chan YF, Dennis ML, Funk RR. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. J Subst Abuse Treat. 2008;34:14–24. doi: 10.1016/j.jsat.2006.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Costello EJ, Armstrong TD, Erkanli A. Report on the developmental epidemiology of comorbid psychiatric and substance use disorders; Paper presented to National Institute on Drug Abuse; Durham, NC: Duke University Medical Center, Center for Developmental Epidemiology; 2000. pp. 1–34. Available from: http://archives.drugabuse.gov/meetings/Childhood/Commissioned/Costello_Armstrong_Erkanli/Costello_Armstrong_Er-kanli.pdf. [Google Scholar]
- 9.Kaminer Y, Connor D, Curry J. Comorbid adolescent substance use and major depressive disorders: A review. Psychiatry. 2007;4:32–43. [PMC free article] [PubMed] [Google Scholar]
- 10.Kaminer Y, Connor DF, Curry JF. Treatment of comorbid adolescent cannabis use and major depressive disorder. Psychiatry. 2008;5:34–39. [PMC free article] [PubMed] [Google Scholar]
- 11.Grella CE, Hser YI, Joshi V, et al. Drug treatment outcomes for adolescents with comorbid mental and substance use disorders. J Nerv Ment Dis. 2001;189:384–392. doi: 10.1097/00005053-200106000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Rowe CL, Liddle HA, Greenbaum PE, et al. Impact of psychiatric comorbidity on treatment of adolescent drug abusers. J Subst Abuse Treat. 2004;26:129–140. doi: 10.1016/S0740-5472(03)00166-1. [DOI] [PubMed] [Google Scholar]
- 13.Couwenbergh C, van den Brink W, Zwart K, et al. Comorbid psychopathology in adolescents and young adults treated for substance use disorders: A review. Eur Child Adolesc Psychiatry. 2006;15:319–328. doi: 10.1007/s00787-006-0535-6. [DOI] [PubMed] [Google Scholar]
- 14.Anthenelli RM, Schuckit MA. Affective and anxiety disorders and alcohol and drug dependence: Diagnosis and treatment. J Addict Dis. 1993;12:73–87. doi: 10.1300/J069v12n03_07. [DOI] [PubMed] [Google Scholar]
- 15.Riggs PD. Treating adolescents for substance abuse and comorbid psychiatric disorders. Sci Pract Perspect. 2003;2:18–29. doi: 10.1151/spp032118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brent DA, Maalouf FT. Pediatric depression: Is there evidence to improve evidence-based treatments? J Child Psychol Psychiatry. 2009;50:143–152. doi: 10.1111/j.1469-7610.2008.02037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mufson L, Sills R. Interpersonal psychotherapy for depressed adolescents (IPT-A): An overview. Nord J Psychiatry. 2006;60:431–437. doi: 10.1080/08039480601022397. [DOI] [PubMed] [Google Scholar]
- 18.Riggs P, Levin F, Green AI, et al. Comorbid psychiatric and substance abuse disorders: Recent treatment research. Subst Abus. 2008;29:51–63. doi: 10.1080/08897070802218794. [DOI] [PubMed] [Google Scholar]
- 19.Kessler RC. The epidemiology of dual diagnosis. Biol Psychiatry. 2004;56:730–737. doi: 10.1016/j.biopsych.2004.06.034. [DOI] [PubMed] [Google Scholar]
- 20.Mueser KT, Drake RE, Wallach MA. Dual diagnosis: A review of etiological theories. Addict Behav. 1998;23:717–734. [PubMed] [Google Scholar]
- 21.Mueser KT, Kavanagh DJ, Brunette M. Implications of research on comorbidity for the nature and management of substance misuse. In: Miller PM, Kavanagh DJ, editors. Translation of Addictions Science into Practice. Amsterdam: Pergamon/Elsevier; 2007. pp. 461–472. [Google Scholar]
- 22.Weisz J, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychol B. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deas D, Brown ES. Adolescent substance abuse and psychiatric comorbidities. J Clin Psychiatry. 2006;67:e02. doi: 10.4088/jcp.0706e02. [DOI] [PubMed] [Google Scholar]
- 24.Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37:122–147. [Google Scholar]
- 25.Restifo K, Bögels S. Family processes in the development of youth depression: Translating the evidence to treatment. Clin Psychol Rev. 2009;29:294–316. doi: 10.1016/j.cpr.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Sander JB, McCarty CA. Youth depression in the family context: Familial risk factors and models of treatment. Clin Child Fam Psychol Rev. 2005;8:203–219. doi: 10.1007/s10567-005-6666-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCarty CA, Weisz JR. Effects of psychotherapy for depression in children and adolescents: What we can (and can’t) learn from meta-analysis and component profiling. J Am Acad Child Psychiatry. 2007;46:879–886. doi: 10.1097/chi.0b013e31805467b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Azrin NH, McMahon PT, Donohue B, et al. Behavior therapy for drug abuse: A controlled treatment outcome study. Behav Res Ther. 1994;32:857–866. doi: 10.1016/0005-7967(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 29.Azrin NH, Donohue B, Teichner GA, et al. A controlled evaluation and description of individual-cognitive problem solving and family-behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. J Child Adolesc Subst. 2001;11:1–43. [Google Scholar]
- 30.Kaminer Y, Burleson JA. Psychotherapies for adolescent substance abusers: 15-month follow-up of a pilot study. Am J Addict. 1999;8:114–119. doi: 10.1080/105504999305910. [DOI] [PubMed] [Google Scholar]
- 31.Waldron HB, Slesnick N, Brody JL, et al. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. J Consult Clin Psychol. 2001;69:802–813. [PubMed] [Google Scholar]
- 32.Kaminer Y, Burleson JA, Goldberger R. Cognitive-behavioral coping skills and psychoeducation therapies for adolescent substance abuse. J Nerv Ment Dis. 2002;190:737–745. doi: 10.1097/00005053-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Liddle HA, Dakof GA, Parker K, et al. Multidimensional family therapy for adolescent drug abuse: Results of a randomized clinical trial. Am J Drug Alcohol Abuse. 2001;27:651–688. doi: 10.1081/ada-100107661. [DOI] [PubMed] [Google Scholar]
- 34.Rowe CL, Liddle HA, Dakof GA. Classifying clinically referred adolescent substance abusers by level of externalizing and internalizing symptoms. J Child Adolesc Subst. 2001;11:41–66. [Google Scholar]
- 35.Robbins MS, Szapocznik J, Horigian VE, et al. Brief strategic family therapy for adolescent drug abusers: A multi-site effectiveness study. Contemp Clin Trials. 2009;30:269–278. doi: 10.1016/j.cct.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robbins MS, Feaster DJ, Horigian VE, et al. Brief Strategic Family Therapy™ versus Treatment As Usual: Results of a multisite randomized trial for substance using adolescents. J Counsel Clin Psychol. 2011;79:713–727. doi: 10.1037/a0025477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fleming CB, Mason WA, Mazza JJ, et al. Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychol Addict Behav. 2008;22:186–197. doi: 10.1037/0893-164X.22.2.186. [DOI] [PubMed] [Google Scholar]
- 38.David-Ferdon C, Kaslow NJ. Evidence-based psychosocial treatments for child and adolescent depression. J Clin Child Adolesc Psychol. 2008;37:62–104. doi: 10.1080/15374410701817865. [DOI] [PubMed] [Google Scholar]
- 39.Silverman WK, Ortiz CD, Viswesvaran C, et al. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. J Clin Child Adolesc Psychol. 2008;37:156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- 40.Feaster DJ, Robbins MS, Henderson C, et al. Equivalence of family functioning and externalizing behaviors in adolescent substance use of different race, ethnicity. J Subst Abuse Treat. 2010;38:S113–S124. doi: 10.1016/j.jsat.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 41.Lucas CP, Zhang H, Fisher PW, et al. The DISC predictive scales (DPS): Efficiently screening for diagnoses. J Am Acad Child Adolesc Psychiatry. 2001;40:443–449. doi: 10.1097/00004583-200104000-00013. [DOI] [PubMed] [Google Scholar]
- 42.Szapocznik J, Hervis O, Schwartz S. Brief Strategic Family Therapy for Adolescent Drug Abuse. Bethesda, MD: National Institute on Drug Abuse; 2003. NIH publication No. 03-4751. [Google Scholar]
- 43.Nunes EV, Ball S, Booth R, et al. Multisite effectiveness trials of treatments for substance abuse and co-occurring problems: Have we chosen the best designs? J Subst Abuse Treat. 2010;38(Suppl. 1):S97–S112. doi: 10.1016/j.jsat.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jaccard J, Guilamo-Ramos V. Analysis of variance frameworks in clinical child and adolescent psychology: Advanced issues and recommendations. J Clin Child Adolesc Psychol. 2002;31:278–294. doi: 10.1207/S15374424JCCP3102_13. [DOI] [PubMed] [Google Scholar]
- 45.Erdfelder E, Faul F, Buchner A. GPOWER: A general power analysis program. Behav Res Meth Ins C. 1996;28:1–11. [Google Scholar]
- 46.Onken LS, Blaine JD, Genser S, et al., editors. Treatment of Drug-Dependent Individuals with Comorbid Mental Disorders. Washington, DC: National Institute on Drug Abuse, US Government Printing Office; 1997. p. 172. National Institute on Drug Abuse Research Monograph Number. [Google Scholar]
- 47.Liddle HA. Advances in family based therapy for adolescent substance abuse. In: Harris LS, editor. Problems of Drug Dependence 2001: Proceedings of the 63rd Annual Scientific Meeting. Vol. NIH publication no. 02-5097. NIDA monograph no. Vol. 182. Bethesda, MD: National Institute on Drug Abuse; 2002. pp. 113–115. [Google Scholar]