Abstract
This article presents a comprehensive review of the menthol cigarette dependence-related literature and results from an original analysis of the Total Exposure Study (TES), which included 1,100 menthol and 2,400 nonmenthol adult smokers. The substantial scientific evidence available related to age of first cigarette, age of regular use, single-item dependence indicators (smoking frequency, cigarettes per day, time to first cigarette, night waking to smoke), smoking duration, numerous validated and widely accepted measures of nicotine/cigarette dependence, and our analysis of the TES do not support that menthol smokers are more dependent than nonmenthol smokers or that menthol increases dependence.
Keywords: Menthol, smoking, dependence, addiction, FTND, CPD, TTFC
INTRODUCTION
A decade ago, concerns were raised that the addition of menthol to cigarettes may enhance addiction to smoking.1 In 2009, Congress passed the Family Smoking Prevention and Tobacco Control Act (FSPTCA), which gave the Food and Drug Administration (FDA) authority to regulate tobacco products based on a public health standard. The FSPTCA directed the FDA to refer “the issue of the impact of the use of menthol in cigarettes on the public health” to the Tobacco Products Scientific Advisory Committee (TPSAC).2 The TPSAC provided its report to the FDA in March 2011.3 Since that time, the FDA has published its own Preliminary Scientific Assessment of Menthol in cigarettes.4 Regarding the impact of menthol on dependence, both reports make conclusions suggesting that menthol is associated with increased dependence. Both reports relied heavily on unpublished and unadjusted analyses. The TPSAC report has not been updated since 2011 and much of the relevant dependence literature, including studies with validated dependence measures and menthol comparisons, is not included in the FDA preliminary report or reference addendum. We believe a thorough assessment of the scientific evidence demonstrates that menthol does not increase cigarette dependence. Our analysis of data from the Total Exposure Study (TES) further supports that menthol smokers are not more dependent on smoking compared with nonmenthol smokers.
In our assessment of the topic, we rely on the peer-reviewed published scientific evidence.4 Studies that included dependence predictors, indicators, and validated dependence measures, which are widely accepted in the scientific community, are included in our review. We also considered the type of statistical testing, whether adjustments were made to control for differences between groups, whether results were statistically significant, and whether there was sufficient detail provided to be able to reproduce the study or analysis. For completeness, we included all identified dependence-related menthol literature results. Those with nonvalidated measures and incomplete descriptions are included in the discussion.
In this article, we also present original results from an analysis of data collected as part of the TES. The TES included 3,585 adult smokers from 31 states across the United States. The TES data were used to estimate exposure to tobacco smoke constituents,6 examine differences in exposure by machine-derived tar yield categories and menthol status,7,8 and compare biomarkers of potential harm in adult smokers and nonsmokers.9 This specific analysis examines Fagerström Test for Nicotine Dependence (FTND) scores, FTND questions, and the Heaviness of Smoking Index (HSI) among 1,104 menthol and 2,481 nonmenthol adult smokers.
Predictor of Cigarette Dependence
The relationship between age of smoking initiation and dependence has been well studied. Early onset of smoking is associated with greater likelihood of developing dependence.10 Hu et al.11 reported that “early age of smoking onset [was]…significantly correlated with daily smoking and lifetime nicotine dependence.” Breslau et al.12 found that after “controlling for sex and race, persons who smoked their first cigarette at 14 to 16 years of age were 1.6 times more likely to become dependent than those who initiated smoking at an older age (P = 0.03).” The relationship between early onset of smoking and dependence was also examined in the National Cancer Institute's (NCI) Monograph 20, which reported that “In terms of smoking trajectories, early smoking onset has been associated with steeper acceleration in smoking rate, greater persistence over time, and greater likelihood of developing dependence.”10,13–15 In a large study examining the presence of dependence among smokers, Donny and Dieker16 found that “non-dependent smokers initiated smoking and daily smoking at a later age.” More recently, Kendler et al.16 concluded that “controlling for genetic and familial-environmental effects, age at onset of regular smoking predicted level of nicotine dependence.” Later smoking initiation is associated with lower cigarette consumption (frequency and cigarettes per day [CPD]), higher rates of smoking cessation, shorter smoking duration, and lower dependence.10,13,18–25 Therefore, comparisons of age of first cigarette and age of daily smoking between menthol and nonmenthol smokers could be useful as a predictor of differences in dependence.
Indicators of Cigarette Dependence
Commonly used single-item dependence indicators include frequency of smoking, CPD, and time to first cigarette (TTFC). More recently, night waking to smoke has been identified as a dependence indicator. Smoking daily, smoking more cigarettes per day, smoking within 30 minutes, and night waking to smoke are listed as the “associated features” of tobacco use disorder in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-IV).26 Non-daily or intermittent smokers often do not meet established dependence criteria. According to the DSM-IV, approximately 50% of daily smokers met DSM-IV criteria for nicotine dependence.26 CPD and TTFC are the 2 main factors that drive FTND scores and together comprise the HSI.27 TTFC is also associated with cigarette consumption, and CPD is associated with night waking to smoke.28 CPD has been described as a proxy for dependence and scientists have evaluated “the importance of phenotype definition (i.e., CPD versus FTCD score as a measure of nicotine dependence) on genome-wide association studies of nicotine dependence.”29 Rice et al.29 concluded that “daily cigarette consumption and the Fagerström Test for Cigarette Dependence show different associations with polymorphisms in genetic loci” associated with nicotine dependence.
The authors who analyzed the National Health Interview Survey (NHIS)30 reported that “In 2011, an estimated 19.0% (43.8 million) of U.S. adults were current cigarette smokers. Of these, 77.8% (34.1 million) smoked every day, and 22.2% (9.7 million) smoked some days.” Recent estimates from the National Survey on Drug Use and Health (NSDUH)31 suggest that among current cigarette smokers aged 12 years or older in 2011, 60.7% were daily smokers. Non-daily smokers often do not meet established dependence criteria, and studies have reported lower scores for intermittent smokers on multiple dependence measures.32,33
Smoking frequency, CPD, TTFC, and night waking to smoke have all been reported as significant predictors of cessation outcomes but are not always consistent across studies.25,28,34,35 For example, the Baker et al.35 analysis reported TTFC predicted cessation, but TTFC was not a significant predictor of cessation in other studies.28,36 Smoking duration has also been associated with cessation outcomes and dependence.10,37,38 Researchers have used other dependence-related statements, questions, and nonvalidated scales to compare menthol and nonmenthol smokers. However, in the current review, we focus on widely accepted and validated indicators and measures.
Validated and Widely Accepted Measures of Cigarette Dependence
Widely used and validated measures of dependence have been described and reviewed by authoritative sources including the U.S. Surgeon General's Report,37 the NCI's Monograph 20,10 and the World Health Organization's International Agency for Research on Cancer39 report. These measures include the following: FTND,40 Fagerström Tolerance Questionnaire,41,42 Cigarette Dependence Scale (CDS-12 and CDS-5),43–45 HSI,46 Nicotine Dependence Syndrome Scale,47,48 Hooked on Nicotine Checklist,49 Wisconsin Inventory of Smoking Dependence Motives,50 DSM-IV,51 and the International Classification of Diseases.52
The FTND has been one of the most widely used extensively studied measures of dependence. The FTND and DSM-IV have been described as the “two gold standard measures for nicotine dependence.”10 The FTND includes 6-items: number of cigarettes smoked per day, time to first cigarette, difficulty refraining from smoking when forbidden, smoking when ill in bed most of the day, which cigarette would hate most to give up, and smoking frequency40,42 Based on the score, nicotine dependence has been classified as very low (0–2), low (3–4), medium (5), high (6–7), or very high (8–10).53 Other researchers have used different classifications in their analysis, such as low/medium (0–5) vs. high (6–10) and low (0–3), medium (4–5), and high (6–10).54 Recently, Dr. Fagerström has proposed that the FTND be renamed to the Fagerström Test for Cigarette Dependence (FTCD).55 We use the FTND when results were reported as such. The HSI, which includes the FTND categories of TTFC and CPD,46 is the shortest widely accepted and validated measure of dependence.
LITERATURE REVIEW METHODS
Identifying Menthol and Dependence Related Scientific Literature
In early 2010 and 2011, we conducted two detailed searches of PubMed and Scopus for any publication with the words “menthol” and “cigarettes” or “smoking.” Since 2011, we have continued to search the literature on a quarterly basis. This review is inclusive of publications that were available in English, either online or in print, prior to January 2014. We have attempted to be inclusive of all articles and all results relevant to nicotine/cigarette dependence in menthol and non-menthol smokers. Dependence measures and indicators are often reported as part of the sample characteristics in articles not focused on dependence.
LITERATURE REVIEW
Cigarette Dependence Predictor Results
Age of Initiation and Progression among Menthol and Nonmenthol Smokers We identified 16 articles that compared the age of initiation or progression to regular smoking among menthol and nonmenthol smokers. These studies reported the mean age of first cigarette, mean age at first regular smoking, or compared the percentage of menthol and nonmenthol smokers in age categories for these two outcomes. Among the 9 studies we identified that examined age of first cigarette use among menthol and nonmenthol smokers, 7 reported no difference in mean age overall and among various subgroups56–62 and 2 reported later age of first cigarette among menthol smokers.62,63
In terms of age of regular smoking, we identified 9 studies. Seven reported no difference in the age of onset of regular smoking between menthol and nonmenthol smokers57,60,65–69 and 3 reported a later average age of regular smoking for menthol smokers.67,70,71 Overall, these studies consistently reported that menthol smokers have the same or later mean age of first use and the same or later mean age of regular smoking.
Cigarette Dependence Indicator Results
In this section, the menthol literature which includes commonly used single-item dependence indicators include frequency of smoking, CPD, TTFC, night waking to smoke, and smoking duration is reviewed.
Smoking Frequency (Daily vs. Non-daily) We identified 8 publications that included information on daily and non-daily smoking among menthol and nonmenthol smokers. Five studies reported that menthol smokers are less likely to be daily smokers.67,70,72–74 Three other large scale analyses reported no difference in daily vs. non-daily smoking among menthol and non-menthol smokers.63,71,75
Cigarettes per Day We identified 30 studies and dozens of analyses within these manuscripts that provide information on CPD among menthol and nonmenthol smokers. With the exception of 1 publication,76 these authors consistently report that menthol smokers smoke the same or fewer CPD compared with nonmenthol smokers.
Dozens of analyses have reported no difference in CPD for menthol versus nonmenthol smokers among daily and non-daily smokers77 by race/ethnicity;65 within specific racial/ethnic groups, including African American/Black,62,67,78,79 White,58,62,67 Hispanic,67,78,79 American Indian/Alaskan Native,67 and Asian/Pacific Islander smokers;67 among both men and women;65,80 and overall.54,57,60,62,68,80–84
Other studies and analyses found that menthol smokers reported statistically significantly fewer CPD compared with nonmenthol smokers. These analyses have reported fewer CPD among menthol versus nonmenthol smokers at baseline;66 within specific racial/ethnic groups of smokers, including African American/Black,58,85,86 Hispanic,58,86 and White smokers;78,79,85,86 among both men and women;87 among White women, African American women, and African American men;88 among former smokers and current smokers;69,78 and overall.36,58,61,63,64,67,70,79,89–91
The one analysis that reported higher cigarette consumption among menthol smokers may have had an error in the coding/analysis. Muilenburg and Legge76 reported that menthol cigarette smokers, and specifically that African American underage menthol cigarette smokers, had the highest rates of cigarette consumption. However, the authors also reported that 81% of the African American smokers in the analysis reported smoking nonmenthol cigarettes. Such a high percentage of nonmenthol use among African American smokers is inconsistent with all other published analyses of the sociodemographic patterns of menthol cigarette use.
Time to First Cigarette (TTFC) We identified 19 publications and dozens of analyses of TTFC among menthol and nonmenthol smokers. For ease in comparing findings of the various studies, the results of the analyses are reviewed in sections on the first 30 minutes versus later, FTND TTFC categories, mean TTFC, and then other TTFC categorizations.
TTFC Within First 30 Minutes vs. after 30 Minutes of Waking. With the exception of one published unadjusted analysis among African Americans81 and one unadjusted analysis among non-daily smokers,77 all other published studies report no difference for menthol versus nonmenthol smoking for TTFC within the first 30 minutes versus after 30 minutes of waking. Nine studies, which included studies with large diverse samples and multivariate analyses, report no difference in TTFC ≤30 minutes versus >30 minutes for menthol and nonmenthol smokers.36,54,57,67,70,77,84,92,93
TTFC FTND categories (≤5, 6–30, 31–60, and >60 Minutes). Two studies reported the percentage of menthol and nonmenthol smokers in the original FTND TTFC categories. In one unadjusted analysis, Collins and Moolchan82 reported a higher percentage of menthol smokers in the TTFC ≤5 minutes category, but no significant differences in the percentage of menthol and nonmenthol in the 6–30, 31–60, or >60 minutes TTFC groups.82 The TTFC ≤5 minutes comparison was based on 12 nonmenthol smokers. The study was limited by an unequal sample size, small overall number of nonmenthol smokers (n = 41), and the lack of adjustment for differences between groups. Jones et al.63 reported 4,603 adults, aged 20+ years who participated in the NHANES 1999-2010. The authors reported no statistically significant difference in the weighted percentage of menthol and nonmenthol smokers in the TTFC ≤5, 6–30, 31–60, and >60 minutes categories.63
Mean TTFC. Two small studies and one large study reported mean TTFC among menthol and nonmenthol smokers. In a sample of 95 women, menthol smokers had a shorter mean TTFC.94 Another study analyzed data from 127 adult smokers (60 menthol smokers and 67 nonmenthol smokers) and found no significant difference.95 In an analysis of data from 46,273 current adult smokers, White menthol smokers had statistically significantly longer mean TTFC compared with White nonmenthol smokers (21 vs. 20 minutes), African American menthol smokers had statistically significantly shorter mean TTFC compared with African American nonmenthol smokers (21 vs. 25 minutes), and no other statistically significant differences were found for any other race/ethnicity groups.70
Other TTFC categorizations. Five additional studies reported various other TTFC categorizations. These studies generally report findings that are mixed, with some results suggesting shorter TTFC, some longer TTFC, and some with no difference in TTFC for menthol versus nonmenthol smokers.62,96,97
One publication included a cohort of 13,268 adult smokers with 5 years follow-up and found baseline menthol use was associated with smoking >60 minutes after waking and menthol smokers were statistically significantly less likely to report smoking within 10 minutes of waking at follow-up.66 An analysis of 46,273 current smokers aged 18 years and older found no overall difference in the percentage of menthol vs. nonmenthol smokers who smoked in the first 5 minutes (22.27 vs. 22.17, respectively), in 6–10 minutes (9.11 vs. 9.51, respectively), 11–15 minutes (7.03 vs. 7.50, respectively), or 16+ minutes (59.09 vs. 58.52, respectively).70 Of the nine CPD TTFC comparisons, only one was significant by menthol status, which was TTFC ≤5 minutes for those who smoked 6–10 CPD.70
Night Waking to Smoke Two studies reported on night waking to smoke among menthol and nonmenthol smokers. Bover et al.28 report that “Night-smoking status was determined by an answer of ‘yes’ to the question ‘Do you sometimes awaken at night to have a cigarette or use tobacco?’” In their multivariate analysis of predictors, menthol smokers had an increased Adjusted Odds Ratio (AOR) for night waking to smoke compared with nonmenthol (AOR, 1.497 [95% confidence interval [CI], 1.195–1.874]); however, menthol was specifically tested and was not a significant predictor of 26-week cessation outcomes.28 An unadjusted analysis from another study reported that a higher percentage of menthol smokers reported sometimes waking at night to smoke.58
Smoking Duration As mentioned in the introduction, smoking duration is associated with nicotine dependence and cessation outcomes.10,36,38 Twelve studies were identified that included smoking duration comparisons by menthol status. Three studies reported no difference,62,84,98 one study reported no difference and shorter duration for two different groups of menthol smokers,83 and the other 8 studies reported shorter smoking duration among menthol versus nonmenthol smokers.57,70,80,85,87,89,90,99
Validated and Widely Accepted Measures of Cigarette Dependence Results
We identified 23 articles in our review.32,56,57,60,68,73,74,80–84,89,92,95,97,98,100–105 Seventeen published studies included validated measures and a menthol comparison, 1 analysis included partial FTND scores, and 5 studies compared validated dependence measures among smokers in racial/ethnic groups with disproportionately high and low menthol use. These studies are summarized in Table 1.
TABLE 1.
Studies with Validated and Widely Accepted Measures of Nicotine/Cigarette Dependence
| Study Authors | Population/Sample | Findings Related to Validated and Widely Accepted Measures of Nicotine/Cigarette Dependence |
|---|---|---|
| Allen & Unger56 | 432 adult AA smokers | No significant difference by menthol status in odds of higher score on FTND for both women and men. |
| Benowitz et al.95 | 127 adult smokers | No significant difference by menthol status in FTND scores. |
| Brody et al.105 | 63 adult smokers | No statistically significant difference in FTND scores for menthol (mean, 4.1; SD±2.1) and nonmenthol (mean, 3.9; SD±2.4) smokers. |
| Collins & Moolchan82 | 572 adolescent smokers (531 smoked menthol) | No difference in FTND scores. |
| DiFranza et al.102 | 237 adolescents | No difference between menthol and nonmenthol on the HONC. |
| Duncan et al.101 | 1,376 adolescents and young adults (12–33 years), 768 AA (56%) and 610 White | Among ever smokers, AA were statistically significantly less likely to be DSM-IV dependent as compared to White (19.82 vs. 32.81, respectively, p<0.001). |
| Faseru et al.57 | 540 AA light smokers (≤10 cigarettes per day) in a clinical trial for smoking cessation | No significant difference between menthol and nonmenthol smokers on numerous measures, including FTND. |
| Hooper et al.103 | 3,396 current smokers from the Florida 2007 BRFSS | Menthol smokers had statistically significantly lower mean scores on the NDSS in the unadjusted analysis. No significant difference between menthol and nonmenthol smokers in AOR of dependence (NDSS) in the multivariate analysis. |
| Kandel & Chen38 | 12,550 White, 4,903 AA, 4,839 Hispanic current smokers (ages 12 and older) from the NHSDA | Despite higher percentage of menthol, minorities smoked significantly fewer CPD compared with Whites. Whites more likely than African-Americans to be DSM-IV dependent even controlling for CPD. |
| Li et al.74 | 14 and 15 year olds in New Zealand. 2,387 menthol and 11,071 nonmenthol. | The authors reported that the “multiple linear regression model did not find a significant result linking reported HONC score to menthol preference (coef. = –.21, P = .165).” |
| Luo et al.92 | 2,925 White and AA adult smokers (not menthol specific) | African-American smokers had lower FTND scores compared with Whites. |
| Marsh et al.73 | New Zealand youth surveys from 2004 (N = 564), 2006 (N = 334), and 2008 (N = 325) | The authors found, “there was no evidence of an association between use of menthol and HONC scores.” Authors state “However, those preferring menthol-only had lower HONC scores than those preferring only nonmenthol.” Lower HONC scores among menthol-only as compared to those who smoke both types of cigarettes. |
| Moolchan et al.100 | 115 treatment seeking adolescents | African American adolescents had significantly lower FTND scores as compared with those who were not African-Americans. |
| Frost-Pineda et al. reported here | 3,585 adult smokers (1,104 menthol and 2,481 nonmenthol) | No significant increased odds of menthol use for any of the FTND questions. Menthol cigarette smoking did not increase the odds of higher FTND scores regardless of how scores were categorized. Higher FTND scores were not associated with increased odds of smoking menthol cigarettes. |
| Muscat et al.97 | 525 adult smokers | No significant increased odds of high FTND scores vs. low/medium FTND scores among menthol as compared to nonmenthol smokers (OR, 1.1, 95% CI, 0.6, 2.1). |
| Murray et al.80 | 5,887 adult smokers | Among males and among females, respectively, there was no significant effect of menthol on partial FTND scores. |
| Mustonen et al.88 | 307 White and AA adult smokers in a clinical study of NRT. Smoked at least 10 CPD | No difference in FTQ scores between White males, White females, African-American males or African-American females. |
| Okuyemi et al.81 | 600 AA smokers in a bupropion trial | No significant difference in FTND scores for menthol compared to nonmenthol. |
| Okuyemi et al.60 | 480 adult AA smokers at an inner-city health center | No significant difference in FTND scores between menthol and nonmenthol cigarette smokers. |
| Okuyemi et al.68 | 755 AA smokers in smoking cessation trial | No significant difference between menthol and nonmenthol on the NDSS or MNWS (a withdrawal scale). |
| Reitzel et al.104 | ||
| 183 adult smokers (83 menthol and 100 nonmenthol) | There was no statistically significant difference in mean HSI score between menthol (3.60) and nonmenthol (3.73) smokers. | |
| Reitzel et al.98 | 1,067 adult smokers | Menthol smokers had statistically significantly lower mean dependence scores as measured by the HSI (p = .01). |
| Rojewski et al.84 | 166 adult smokers | No significant difference between menthol and nonmenthol smokers in mean FTND scores. |
| Winhusen et al.83 | 510 adult smokers | No statistically significant difference in FTND scores by menthol status. |
AA = African American; AI = American Indian; AN = Alaska Native; AOR = adjusted odds ratio; BRFSS = Behavioral Risk Factor Surveillance System; CPD = cigarettes per day; FTND = Fagerström Test for Nicotine Dependence; FTQ = Fagerström Tolerance Questionnaire; HONC, Hooked on Nicotine Checklist; HSI = Heaviness of Smoking Index; MNWS = Minnesota Nicotine Withdrawal Scale; NDSS = Nicotine Dependence Syndrome Scale; NHIS = National Health Interview Survey; NHSDA = National Household Survey on Drug Abuse; NRT = nicotine replacement therapy; PI = Pacific Islander; TTFC = time to first cigarette; TUS CPS = Tobacco Use Supplements to the Current Population Surveys
Whereas the percentage of menthol smokers is higher, studies have reported that African American adolescent smokers have lower FTND scores and DSM-IV dependence compared with Whites.38,100,101 Among adults as well, African American smokers were reported to have lower FTND scores and DSM-IV dependence compared with White smokers.38,92
Among adolescents, studies have found no difference by menthol status on the Hooked on Nicotine Checklist,73,74,102 and lower Hooked on Nicotine Checklist scores for adolescent preferring only menthol vs. only nonmenthol and compared to those who smoked both.73 No difference by menthol status on the FTND was reported in another study of adolescents.82
Other studies have reported no significant effect of menthol on partial FTND scores among adult men and women,80 no difference by menthol status by race and gender in Fagerström Tolerance Questionnaire scores,88 and no difference by menthol status on the Nicotine Dependence Syndrome Scale among adults.68,103 Menthol smokers are also reported to score the same or lower on the HSI.97,103 Nine studies among adults have found no difference by menthol status on the FTND.54,56,57,60,81,83,84,95,105
TES METHODS
Study Design and Conduct
The TES was a cross-sectional, multi-center, ambulatory study conducted at 39 clinical sites across the United States. Details about the design of the study have been reported elsewhere.6,7,106 Covance Clinical Research Unit Inc. managed the recruitment of participants and study conduct. Healthy men and women who were aged at least 21 years at study entry were screened for enrollment. Adult smokers must have reported smoking at least one manufactured cigarette per day for at least the past year. They could not have used any other nicotine-containing products and must not have changed brands or have reported smoking more than 10% of their daily cigarette consumption outside their regular brand's tar yield category for the 3 months preceding visit 1. Participants were not eligible for inclusion if they were pregnant or nursing. Good Clinical Practice and the principles of the Declaration of Helsinki107 were followed in all aspects of the TES. The study was Institutional Review Board–approved and informed consent was documented prior to participation.
Statistical Methods for FTND and HSI Scores between Menthol and Nonmenthol Smokers
Logistic regression models were used to examine the relationships between menthol smoking status and the FTND. The response variables were measures of nicotine dependence (FTND) for Model A and menthol smoking status for Model B. Model B was used to compare the results with previous publications in the literature. The explanatory factors included in the models were age (21–34 years, 35–49 years, 50 + years), gender (male or female), race (African American/Black or White), education level (<high school graduate, high school graduate, college graduate), annual household income (<$20,000, $20,000–$49,999, $50,000+) and machine-measured tar yield category (T1: ≤2.9; T2: 3.0–6.9; T3: 7.0–12.9; T4: ≥ 13.0 mg).
In Model A, in addition to using the conventional FTND levels as the response variable, several other FTND categories were used. In addition, the interaction term menthol status by race was included in Model A with the other mentioned explanatory factors. Each question of the FTND was also analyzed individually. In Model B, the probability of being a menthol smoker was modeled. In a separate model, TTFC was compared between menthol and nonmenthol smokers. In another model, the effect of menthol status on the HSI was tested.
The SAS PROC LOGISTICS procedure was used to run the logistic regression models. Statistical significance was evaluated at P < .05. Missing values for any of the variables required for a specific analysis resulted in the observation being excluded from the analysis. SAS version 9.1.3 software was used to perform the statistical analysis.
TES Results
In the TES study, 30% of adult smokers reported they smoked menthol cigarettes. Twenty-two percent of White smokers and 73% of African American smokers smoked menthol cigarettes. Descriptive statistics for sociodemographic characteristics and smoking-related variables of menthol and nonmenthol smokers is presented in Table 2. Results are reported for African American and White smokers as there were few respondents from other Racial groups.
TABLE 2.
Descriptive Statistics for Demographics and Smoking History
| Characteristic | Menthol (n = 1044) | Nonmenthol (n = 2297) |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 41.8 (12.1) | 42.0 (13.0) |
| Range (min, max) | (21, 76) | (21, 80) |
| Gender, No. (%) | ||
| Female | 664 (63.6) | 1258 (54.8) |
| Male | 380 (36.4) | 1039 (45.2) |
| Race, No. (%) | ||
| African American | 448 (42.9) | 166 (7.2) |
| White | 596 (57.1) | 2131 (92.8) |
| BMI (kg/m2) | ||
| Mean (SD) | 28.57 (7.33) | 27.31 (6.29) |
| Range (min, max) | (16.0, 66.7) | (15.0, 70.0) |
| Annual Household Income, No. (%) | ||
| <$20,000 | 374 (36.0) | 604 (26.4) |
| $20,000–$49,999 | 451 (43.4) | 1083 (47.3) |
| ≥$50,000 | 214 (20.6) | 603 (26.3) |
| Number missing | 5 | 7 |
| Education, No. (%) | ||
| <High school graduate | 114 (11.0) | 163 (7.1) |
| High school graduate | 756 (72.8) | 1745 (76.4) |
| College graduate | 168 (16.2) | 375 (16.4) |
| Number missing | 6 | 14 |
| Region, No. (%) | ||
| Midwest | 203 (19.4) | 525 (22.9) |
| Northeast | 179 (17.1) | 251 (10.9) |
| South | 471 (45.1) | 745 (32.4) |
| West | 191 (18.3) | 776 (33.8) |
| Cigarettes smoked per day, Mean (SD) and No. (%) | ||
| Mean (SD) | 15.0 (8.7) | 16.8 (9.0) |
| Range (min, max) | (1, 54) | (1, 84) |
| 1–10 CPD | 374 (35.8) | 594 (25.9) |
| 11–20 CPD | 442 (42.3) | 1054 (45.9) |
| 21–30 CPD | 168 (16.1) | 479 (20.9) |
| <30 CPD | 59 (5.7) | 165 (7.2) |
| Number missing | 1 | 5 |
| Tar category, No. (%) | ||
| ≤2.9 mg | 154 (14.8) | 326 (14.2) |
| 3.0–6.9 mg | 198 (19.0) | 694 (30.2) |
| 7.0–12.9 mg | 239 (22.9) | 753 (32.8) |
| ≥13.0 mg | 453 (43.4) | 524 (22.8) |
Results for FTND and HSI Analysis
Mean FTND scores were similar for menthol (4.5 [SD, 2.13]) and nonmenthol adult smokers (4.6 [SD, 2.14]). A histogram of the FTND scores is presented in Figure 1. After adjusting for covariates, the following factors were associated with higher odds of smoking menthol cigarettes in the logistic regression model: women compared with men; African Americans compared with Whites; smoking a cigarette ≥13 mg tar yield compared with cigarettes ≤2.9 mg tar yield and being aged 34–49 years versus aged 21–31 years (Table 3). No significant increased odds of menthol use for any of the FTND questions were found (Table 3).
FIGURE 1.
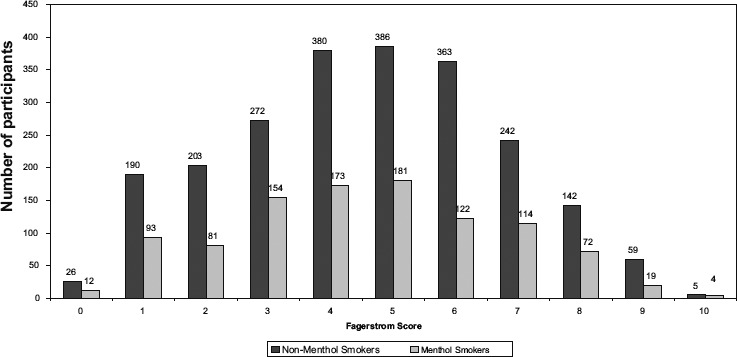
Histogram of FTND scores for menthol and nonmenthol smokers.
TABLE 3.
Odds of Menthol Use in the Total Exposure Study
| Characteristic | No. | Percentage menthol | OR for menthol* | 95% CI |
|---|---|---|---|---|
| Gender | ||||
| Male | 1419 | 26.8 | 1.00 | Reference |
| Female | 1922 | 34.6 | 2.13 | 1.78 to 2.56 |
| Age | ||||
| 21–34 years | 1041 | 29.3 | 1.00 | Reference |
| 35–49 years | 1328 | 35.8 | 1.31 | 1.07 to 1.62 |
| 50+ years | 972 | 27.2 | 1.13 | 0.90 to 1.42 |
| Race | ||||
| White | 2727 | 21.9 | 1.00 | Reference |
| African American | 614 | 73 | 9.53 | 7.52 to 12.09 |
| Education | ||||
| <High school graduate | 277 | 41.2 | 1.00 | Reference |
| High school graduate | 2501 | 30.2 | 0.85 | 0.62 to 1.16 |
| College graduate | 543 | 30.9 | 1.25 | 0.86 to 1.82 |
| Income | ||||
| <$20,000 | 978 | 38.2 | 1.00 | Reference |
| $20,000–$49,999 | 1534 | 29.4 | 1.04 | 0.84 to 1.27 |
| ≥$50,000 | 817 | 26.2 | 1.08 | 0.84 to 1.39 |
| Tar Yield Category | ||||
| ≤2.9 mg | 480 | 32.1 | 1.00 | Reference |
| 3.0–6.9 mg | 892 | 22.2 | 0.98 | 0.73 to 1.30 |
| 7.0–12.9 mg | 992 | 24.1 | 1.26 | 0.95 to 1.66 |
| ≥13.0 mg | 977 | 46.4 | 2.25 | 1.72 to 2.96 |
| Time until first cigarette | ||||
| ≤5 minutes | 997 | 33.8 | 0.88 | 0.62 to 1.25 |
| 6–30 minutes | 1421 | 31.3 | 0.90 | 0.66 to 1.23 |
| 30–60 minutes | 486 | 24.5 | 0.70 | 0.50 to 0.98 |
| ≥60 minutes | 428 | 32.2 | 1.00 | Reference |
| Hate most to give up | ||||
| First in the morning | 1592 | 34.2 | 1.10 | 0.91 to 1.32 |
| All other | 1736 | 27.9 | 1.00 | Reference |
| How many smoked/day | ||||
| 10 or less | 740 | 40 | 1.00 | Reference |
| 11–20 | 1624 | 29.9 | 0.97 | 0.76 to 1.24 |
| 21–30 | 725 | 25.7 | 1.04 | 0.76 to 1.41 |
| 31 or more | 230 | 30.4 | 1.40 | 0.93 to 2.10 |
| ↑ during 1 h waking/rest of day | ||||
| No | 1917 | 30.9 | 1.00 | Reference |
| Yes | 1405 | 31.3 | 0.94 | 0.78 to 1.14 |
| Refrain forbidden places | ||||
| No | 2480 | 30.8 | 1.00 | Reference |
| Yes | 844 | 32.4 | 1.08 | 0.88 to 1.32 |
| Ill in bed most of the day | ||||
| No | 2010 | 30 | 1.00 | Reference |
| Yes | 1317 | 32.8 | 1.11 | 0.92 to 1.34 |
Odds ratio from logistic regression model adjusting for all other factors listed in the Table.
CI = confidence interval; OR = odds ratio.
Menthol cigarette smoking did not increase the odds of higher FTND scores regardless of how the FTND scores were categorized (i.e., in 5 categorizes, 3 or 2 categories [Table 4]).
TABLE 4.
Effect of Menthol Status on FTND Scores and Time to First Cigarette (Model A)
| Menthol status | Odds ratio | 95% CI |
|---|---|---|
| Fagerström's categorization of the scoresa | ||
| Menthol | 1.05 | 0.91 to 1.22 |
| Nonmenthol | 1 | Reference |
| Low/Medium (0–5) vs. high (6–10) scores | ||
| Menthol | 0.94 | 0.79 to 1.13 |
| Nonmenthol | 1 | Reference |
| Low (0–3), medium (4–5), and high (6–10) scores | ||
| Menthol | 0.97 | 0.83 to 1.13 |
| Nonmenthol | 1 | Reference |
| Time to first cigarette: >30 minutes, ≤ 30 minutes | ||
| Menthol | 0.88 | 0.72 to 1.05 |
| Nonmenthol | 1 | Reference |
5 categories: very low: 0–2 points, low: 3–4 points, medium: 5 points, high: 6–7 points, very high: 8–10 points.
Note: Adjusted for age, race, gender, education and tar yield category.
No statistically significant difference was observed.
CI = confidence interval.
The interaction term menthol smoking status (i.e., menthol or nonmenthol) by race (i.e., African American/Black or White) was not statistically significant in Model A. This indicates that there is no evidence that menthol smoking status affects FTND scores differently in African Americans/Blacks and Whites.
Higher FTND scores were not associated with increased odds of smoking menthol cigarettes (Table 5).
TABLE 5.
Effect of the FTND Scores and Time to First Cigarette on Menthol Status (Model B)
| Measure | Nonmenthol | Menthol | Odds Ratio | 95% CI |
|---|---|---|---|---|
| 5 categories: very low: 0–2 points, low: 3–4 points, medium: 5 points, high: 6–7 points, very high: 8–10 points | ||||
| Very Low FTND | 419 | 186 | 0.84 | 0.64 to 1.12 |
| Low FTND | 652 | 327 | 0.96 | 0.75 to 1.24 |
| Medium FTND | 386 | 181 | 1 | Reference |
| High FTND | 605 | 236 | 0.89 | 0.69 to 1.16 |
| Very High FTND | 206 | 95 | 1.32 | 0.95 to 1.83 |
| 2 categories: low/medium (0–5) and high (6–10) scores | ||||
| Low/Medium FTND | 1457 | 694 | 1 | Reference |
| High FTND | 811 | 331 | 1.05 | 0.88 to 1.26 |
| 3 categories: low (0–3), medium (4–5) and high (6–10) scores | ||||
| Low FTND | 691 | 340 | 1 | Reference |
| Medium FTND | 766 | 354 | 1.01 | 0.82 to 1.24 |
| High FTND | 811 | 331 | 1.06 | 0.86 to 1.31 |
| Time to First Cigarette (TTFC) | ||||
| TTFC > 30 minutes | 657 | 257 | 1 | Reference |
| TTFC ≤ 30 minutes | 1636 | 782 | 1.17 | 0.96 to 1.42 |
Note: Adjusted for age, race, gender, education and tar yield category. No statistical significance was observed at a P value < .05.
CI = confidence interval; FTND = Fagerström Test for Nicotine Dependence
Menthol smokers have about the same odds of smoking their first cigarette more than 30 minutes after they wake up as nonmenthol smokers when adjusted for the other factors (Tables 4 and 5). In addition, the interaction term, menthol smoking status (i.e., menthol or nonmenthol) by race (i.e., African-American/Black or White) was not statistically significant in Model A. No statistically significant effect of menthol was observed on HSI scores (Table 6).
TABLE 6.
Effect of Menthol Status on Heaviness of Smoking Index (HSI) Score
| Menthol status | Odds ratio | 95% CI |
|---|---|---|
| HSI score | ||
| Menthol | 1 | Reference |
| Nonmenthol | 1.13 | 0.95 to 1.34 |
Note: Adjusted for age, race, gender, education, income and tar yield category.
No statistically significant difference was observed.
CI = confidence interval.
DISCUSSION
Our review of the scientific evidence included widely accepted predictors, indicators, and validated measures of nicotine/cigarette dependence that have been published in the peer-reviewed literature. We are aware of 4 other menthol analyses in the literature that include incomplete descriptions and measures that are not listed among validated measures.10,37,39 These publications include three analyses of the National Youth Tobacco Survey by Wackowski and Delnevo107 and Hersey et al.109,110 and a report by Nonnemaker et al.111 Mixed findings were reported in the odds of endorsing three110 or four108 dependence-related statements. It is problematic that although the models in both of these publications did not adjust for socioeconomic status, both did adjust their dependence-related statement analyses for frequency of smoking in the past 30 days and CPD, both of which are dependence indicators. Hersey et al.109 reported that menthol smokers had a significantly higher odds of being above the median on a nicotine dependence scale for adolescents but no details about the scores (medians, means, SD or 95% CI) are provided. Nonnemaker et al.111 reported a statistically significant association between menthol and higher levels of dependence in the third wave of the survey (β = 1.25; 95% CI, 0.10–2.4). However, it is not clear from the data presented whether this is a meaningful difference in scores. The analyses included a scale that was not validated, scores for menthol and nonmenthol smokers were not provided, and no adjustment was made for socioeconomic status.111 Mean scores on the questionnaire were similar for White and African American adolescent smokers despite the difference in the proportion who reported menthol.110
We note there are several instances where validated dependence measure comparisons between menthol and nonmenthol smokers have been made and presented to the FDA and TPSAC at public meetings, but the results are not included in subsequent publications. For example, Reitzel112–114 presented analyses from 3 studies with 3 different populations to the TPSAC and the FDA Center for Tobacco Products showing that menthol smokers were not more dependent as measured by the Wisconsin Inventory of Smoking Dependence Motives (WISDM-68) and that there was no statistically significant difference on any of the 13 WISDM subscales in their multivariate analyses. These results are available online and are referenced in the TPSAC's report to the FDA Center for Tobacco Products,3 but are not mentioned in the subsequent publications.98,104,115
In the current study, we reviewed dependence-related predictors, indicators, and validated dependence measures in menthol versus nonmenthol smokers. We note that menthol cigarette smokers are not a homogenous population. There are notable sociodemographic differences between menthol smokers and nonmenthol smokers, and these differences (and differences in subgroups of menthol and nonmenthol cigarette smokers), if not controlled for, could affect measures of disease risk and behavioral outcomes. Analyses of national surveys report that menthol smokers are “mainly female, aged 45–64, non-Hispanic white, married, blue-collar workers, smokers who lived in the South and metropolitan areas and who reported having attained a high school diploma or GED.”70
Based on the 2006/2007 Tobacco Use Supplement to the Current Population Survey, approximately 27% of current adult smokers in the United States report smoking menthol cigarettes.115 The percentage of menthol use within each sociodemographic group varies. Specifically, the percentage of adult smokers who smoke menthol cigarettes is higher (>27% and non-overlapping 95% CI with other groups) among the following:
Women compared with men.
Those between ages 18–24 and 45–64 years compared with those who are aged 24–44 years and those who are 65+ years.
African Americans compared with every other race/ethnicity group.
Those who have a family income of <$25,000 per year compared with all other income groups.
Those with some high school education compared with those in other educational attainment groups.
Service workers compared with blue- and white-collar workers.
The unemployed compared with those who are employed and those who are not in the labor force.
Studies that adjust for these differences between menthol and nonmenthol smokers are better able to assess the impact of menthol on outcomes.
Numerous publications have reported the different patterns of menthol use in various groups (by gender, race/ethnicity, age, etc.),65,67,70,71,72 provided reasons for different patterns of use,56,59,117,118 and commented on initiation among menthol and nonmenthol smokers.102,111 Although this literature is important to understanding the overall public health implications of menthol versus nonmenthol smoking, it is beyond the scope of this review, which is focused on dependence.
Because measures of dependence are often associated with measures of cessation, a comprehensive review of the cessation-related menthol literature would also be useful for the scientific community and regulatory agencies. Briefly, we recognize that there are numerous studies with cessation-related indicators and outcomes, such as quit intentions, thinking about quitting, confidence in quitting, motivation to quit, desire to quit, reasons for not quitting, quit attempts, relapse, length of abstinence, and short- and long-term cessation outcomes by menthol status that are also informative. A review of studies with long-term cessation outcomes (6 months to >5 years) also supports the conclusion that menthol does not increase dependence. Many studies have reported that there is no difference in cessation and no effect of menthol on various long-term cessation outcomes overall28,61,66,68,80,81,85,96,104,115,119–123 or in specific subgroups, such as among White and Hispanic smokers58 and among those who received placebo gum or motivational interview.68 Fu et al.35 reported that menthol smokers who received an intervention had increased odds of cessation as compared to nonmenthol smokers. The Hyland et al.66 and Murray et al.80 studies are particularly noteworthy because they included the largest cohorts and long length of follow-up (5 years).
In our review of the dependence-related menthol scientific literature, we found 16 publications that compared age of initiation or progression among menthol and nonmenthol smokers. Overall, these studies consistently reported that menthol smokers have the same or later mean age of first use and the same or later mean age of regular smoking. Of the 8 publications that included information on smoking frequency, 5 reported menthol smokers were less likely to be daily smokers and more likely to be some day smokers as compared to nonmenthol smokers, and 3 reported no difference in smoking frequency. We identified 30 studies and dozens of analyses that provide information on CPD among menthol and nonmenthol smokers. More than two dozen analyses found no difference in CPD for menthol versus nonmenthol, including various subgroup analyses and in the overall sample. More than two dozen other analyses found fewer CPD for menthol versus nonmenthol smokers. Only 1 publication reported a higher cigarette consumption among menthol smokers, but it appears there may have been an error in the menthol/nonmenthol coding or analysis. With that one exception, all other studies and analyses report that menthol smokers smoke the same or fewer CPD compared with nonmenthol smokers.
Our review included 19 publications and dozens of analyses of TTFC among menthol and nonmenthol smokers. The published literature related to TTFC includes various TTFC categories. Some publications have focused on the TTFC ≤5 minutes comparisons, whereas the TTFC >60 minutes comparison is equally important as a predictor of cessation outcomes.35
Most studies that have examined TTFC within the first 30 minutes of waking and found no difference between menthol and nonmenthol smokers. Of the 2 studies that compared FTND TTFC categories, 1 had a small and unequal sample size of nonmenthol smokers and the other large study found no difference in any of the four TTFC categories. Studies that included other categorizations of TTFC and studies examining mean TTFC have reported mixed results, including shorter, longer, and no difference in TTFC. The available studies with large, diverse samples and multivariate analyses do not support that menthol smokers overall have shorter TTFC, and some results suggest longer TTFC. Of the 2 studies available that included a measure of night waking to smoke, both studies reported a higher percentage of menthol smokers reporting they sometimes wake at night to smoke compared with nonmenthol smokers. Of these 2 studies, 1 did not adjust for the differences between groups and the other found that menthol was not a predictor of cessation. Among 12 studies that examined smoking duration, 4 reported no difference in smoking duration and the other 8 reported shorter smoking duration among menthol versus nonmenthol smokers. Every published study available with validated and widely accepted dependence measures consistently found that menthol smokers scored the same or lower on established measures of nicotine/cigarette dependence as compared to nonmenthol smokers.
The main limitation of this review and analysis is that most studies were not specifically designed to address the impact of menthol on cigarette dependence. Some studies had small and unequal sample sizes of menthol and nonmenthol smokers, and other studies did not control for differences between the menthol and nonmenthol groups. Although we attempted to be inclusive, there may be additional articles that include dependence measures or indicators as part of the description of sample characteristics that were not identified in our literature search. This review was focused on dependence related analysis and therefore is not inclusive of other menthol-related studies. Although the TES was not designed specifically to assess the effect of menthol status on dependence scores, to our knowledge, this analysis contains the largest sample to date for which overall FTND scores, the HSI, and the results for each of the FTND questions are examined.
SUMMARY AND CONCLUSIONS
The published literature does not support that menthol smokers are more dependent than nonmenthol smokers. Menthol smokers do not have an earlier age of first cigarette smoked or an earlier age of progression to regular smoking compared with nonmenthol smokers. Menthol smokers are not more likely to smoke daily, do not smoke greater CPD, do not consistently have shorter TTFC, and do not have longer duration of smoking. Most directly relevant to answering the questions surrounding menthol and dependence, the published literature consistently demonstrated that menthol smokers do not score higher on validated measures of nicotine/cigarette dependence. Our analysis of the TES data is consistent with the literature in that menthol status also had no statistically significant effect on any single item, the HSI, or overall FTND scores regardless of how the FTND scores were categorized. These results strengthen the existing scientific evidence which demonstrates menthol does not have an effect on nicotine/cigarette dependence.
ACKNOWLEDGEMENTS
The authors thank Lynn Downing, MLS, for her assistance in identifying potentially relevant literature and reference formatting.
FUNDING
This work was supported by Altria Client Services Inc.
REFERENCES
- 1.Henningfield JE, Benowitz NL, Ahijevych K, Garrett BE, Connolly GN, Wayne GF. Does menthol enhance the addictiveness of cigarettes? An agenda for research. Nicotine Tob Res. 2003;5:9–11. doi: 10.1080/1462220031000070543. [DOI] [PubMed] [Google Scholar]
- 2.Tobacco Products Scientific Advisory Committee. Menthol cigarettes and public health: review of the scientific evidence andrecommendations. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/TobaccoProductsScientificAdvisoryCommittee/UCM269697.pdf (accessed May 13, 2014)
- 3.Family Smoking Prevention and Tobacco Control Act. Section 907 of the Federal Food, Drug, and Cosmetic Act – Tobacco Product Standards. http://www.fda.gov/tobaccoproducts/guidancecomplianceregulatoryinformation/ucm263053.htm (accessed May 8, 2014)
- 4.Food and Drug Administration. Preliminary scientific evaluation of the possible public health effects of menthol versus nonmenthol cigarettes. http://www.fda.gov/downloads/ScienceResearch/SpecialTopics/PeerReviewofScientificInformationandAssessments/UCM361598.pdf (accessed May 13, 2014)
- 5.Committee on the Development of the Third Edition of the Reference Manual on Scientific Evidence, Committee on Science TLC, Policy and Global Affairs (PGA), Federal Judicial Center, National Research Council. Reference manual on scientific evidence. 3rd ed. Washington, DC: The National Academies Press; 2011. [Google Scholar]
- 6.Roethig HJ, Munjal S, Feng S, et al. Population estimates for biomarkers of exposure to cigarette smoke in adult U.S. cigarette smokers. Nicotine Tob Res. 2009;11:1216–25. doi: 10.1093/ntr/ntp126. [DOI] [PubMed] [Google Scholar]
- 7.Mendes P, Liang Q, Frost-Pineda K, Munjal S, Walk RA, Roethig HJ. The relationship between smoking machine derived tar yields and biomarkers of exposure in adult cigarette smokers in the US. Regul Toxicol Pharmacol. 2009;55:17–27. doi: 10.1016/j.yrtph.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Roethig HJ, Appleton S, Werley M, Muhammad-Kah R, Mendes P. The effect of menthol containing cigarettes on adult smokers’ exposure to nicotine and carbon monoxide. Regul Toxicol Pharmacol. 2010;57:24–30. doi: 10.1016/j.yrtph.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Frost-Pineda K, Liang Q, Liu J, et al. Biomarkers of potential harm among adult smokers and nonsmokers in the total exposure study. Nicotine Tob Res. 2011;13:182–93. doi: 10.1093/ntr/ntq235. [DOI] [PubMed] [Google Scholar]
- 10.National Cancer Institute. Phenotypes and endophenotypes: foundations for genetic studies of nicotine use and dependence. In: Swan GE, Baker TB, Chassin L, Conti DV, Lerman C, Perkins KA, editors. Tobacco Control Monograph No. 20. NIH Publication No. 09-6366. Washington, DC: National Institutes of Health, National Cancer Institute; 2009. U.S. Department of Health and Human Services. [Google Scholar]
- 11.Hu MC, Davies M, Kandel DB. Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. Am J Public Health. 2006;96:299–308. doi: 10.2105/AJPH.2004.057232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breslau N, Fenn N, Peterson EL. Early smoking initiation and nicotine dependence in a cohort of young adults. Drug Alcohol Depend. 1993;33:129–37. doi: 10.1016/0376-8716(93)90054-t. [DOI] [PubMed] [Google Scholar]
- 13.Breslau N, Peterson EL. Smoking cessation in young adults: age at initiation of cigarette smoking and other suspected influences. Am J Public Health. 1996;86:214–20. doi: 10.2105/ajph.86.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chassin L, Presson CC, Pitts SC, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychol. 2000;19:223–31. [PubMed] [Google Scholar]
- 15.Riggs NR, Chou CP, Li C, Pentz MA. Adolescent to emerging adulthood smoking trajectories: when do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine Tob Res. 2007;9:1147–54. doi: 10.1080/14622200701648359. [DOI] [PubMed] [Google Scholar]
- 16.Donny EC, Dierker LC. The absence of DSM-IV nicotine dependence in moderate-to-heavy daily smokers. Drug Alcohol Depend. 2007;89:93–6. doi: 10.1016/j.drugalcdep.2006.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kendler KS, Myers J, Damaj MI, Chen X. Early smoking onset and risk for subsequent nicotine dependence: a monozygotic co-twin control study. Am J Psychiatry. 2013;170:408–13. doi: 10.1176/appi.ajp.2012.12030321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Department of Health and Human Services. Preventing tobacco use among youth and young adults: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- 19.National Cancer Institute. Cancer Trends Progress Report—2011/2012 Update. Bethesda, MD: National Cancer Institute, NIH, DHHS; 2012. [Google Scholar]
- 20.Storr CL, Zhou H, Liang KY, Anthony JC. Empirically derived latent classes of tobacco dependence syndromes observed in recent-onset tobacco smokers: epidemiological evidence from a national probability sample survey. Nicotine Tob Res. 2004;6:533–45. doi: 10.1080/14622200410001696493. [DOI] [PubMed] [Google Scholar]
- 21.Khuder SA, Dayal HH, Mutgi AB. Age at smoking onset and its effect on smoking cessation. Addict Behav. 1999;24:673–7. doi: 10.1016/s0306-4603(98)00113-0. [DOI] [PubMed] [Google Scholar]
- 22.D'Avanzo B, La Vecchia C, Negri E. Age at starting smoking and number of cigarettes smoked. Ann Epidemiol. 1994;4:455–9. doi: 10.1016/1047-2797(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 23.Chen J, Millar WJ. Age of smoking initiation: implications for quitting. Health Rep. 1998;9:39–46. [PubMed] [Google Scholar]
- 24.Everett SA, Warren CW, Sharp D, Kann L, Husten CG, Crossett LS. Initiation of cigarette smoking and subsequent smoking behavior among U.S. high school students. Prev Med. 1999;29:327–33. doi: 10.1006/pmed.1999.0560. [DOI] [PubMed] [Google Scholar]
- 25.Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Control. 1997;6(Suppl 2):S57–S62. doi: 10.1136/tc.6.suppl_2.s57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, DSM-5. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 27.Kozlowski LT, Porter CQ, Orleans CT, Pope MA, Heatherton T. Predicting smoking cessation with self-reported measures of nicotine dependence: FTQ, FTND, and HSI. Drug Alcohol Depend. 1994;34:211–6. doi: 10.1016/0376-8716(94)90158-9. [DOI] [PubMed] [Google Scholar]
- 28.Bover MT, Foulds J, Steinberg MB, Richardson D, Marcella SW. Waking at night to smoke as a marker for tobacco dependence: patient characteristics and relationship to treatment outcome. Int J Clin Pract. 2008;62:182–90. doi: 10.1111/j.1742-1241.2007.01653.x. [DOI] [PubMed] [Google Scholar]
- 29.Rice JP, Hartz SM, Agrawal A, et al. CHRNB3 is more strongly associated with Fagerström test for cigarette dependence-based nicotine dependence than cigarettes per day: phenotype definition changes genome-wide association studies results. Addiction. 2012;107:2019–28. doi: 10.1111/j.1360-0443.2012.03922.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agaku I, King B, Dube SR. Current cigarette smoking among adults–United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:889–94. [PubMed] [Google Scholar]
- 31.Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: summary of national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. HHS Publication No. (SMA) 12-4713. [Google Scholar]
- 32.Shiffman S, Dunbar MS, Scholl SM, Tindle HA. Smoking motives of daily and non-daily smokers: a profile analysis. Drug Alcohol Depend. 2012;126:362–8. doi: 10.1016/j.drugalcdep.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shiffman S, Ferguson SG, Dunbar MS, Scholl SM. Tobacco dependence among intermittent smokers. Nicotine Tob Res. 2012;14:1372–81. doi: 10.1093/ntr/nts097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction. 2005;100:299–303. doi: 10.1111/j.1360-0443.2004.00995.x. [DOI] [PubMed] [Google Scholar]
- 35.Baker RR, Piper M, McCarthy D, et al. Time to first cigarette in the morning as an index of ability to quit smoking: implications for nicotine dependence. Nicotine Tob Res. 2007;9(Suppl 4):S555–S570. doi: 10.1080/14622200701673480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fu SS, Okuyemi KS, Partin MR, et al. Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine Tob Res. 2008;10:457–62. doi: 10.1080/14622200801901914. [DOI] [PubMed] [Google Scholar]
- 37.U.S. Department of Health and Human Services. How tobacco smoke causes disease: The biology and behavioral basis for smoking – attributable disease: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [PubMed] [Google Scholar]
- 38.Kandel DB, Chen K. Extent of smoking and nicotine dependence in the United States: 1991–1993. Nicotine Tob Res. 2000;2:263–74. doi: 10.1080/14622200050147538. [DOI] [PubMed] [Google Scholar]
- 39.International Agency for Research on Cancer. Methods for Evaluating Cancer Control Policies. Vol. 12. Lyon, France: International Agency for Research on Cancer; 2008. IARC Handbooks of Cancer Prevention. [Google Scholar]
- 40.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 41.Fagerström KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav. 1978;3:235–41. doi: 10.1016/0306-4603(78)90024-2. [DOI] [PubMed] [Google Scholar]
- 42.Fagerström KO, Schneider NG. Measuring nicotine dependence: a review of the Fagerström Tolerance Questionnaire. J Behav Med. 1989;12:159–82. doi: 10.1007/BF00846549. [DOI] [PubMed] [Google Scholar]
- 43.Etter JF, Le Houezec J, Perneger TV. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology. 2003;28:359–70. doi: 10.1038/sj.npp.1300030. [DOI] [PubMed] [Google Scholar]
- 44.Etter JF, Le Houezec J, Huguelet P, Etter M. Testing the Cigarette Dependence Scale in 4 samples of daily smokers: psychiatric clinics, smoking cessation clinics, a smoking cessation website and in the general population. Addict Behav. 2009;34:446–50. doi: 10.1016/j.addbeh.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 45.Okuyemi KS, Pulvers KM, Cox LS, et al. Nicotine dependence among African American light smokers: a comparison of three scales. Addict Behav. 2007;32:1989–2002. doi: 10.1016/j.addbeh.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84:791–800. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 47.Shiffman S, Waters AJ, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6:327–48. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- 48.Shiffman S, Sayette MA. Validation of the nicotine dependence syndrome scale (NDSS): a criterion-group design contrasting chippers and regular smokers. Drug Alcohol Depend. 2005;79:45–52. doi: 10.1016/j.drugalcdep.2004.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.DiFranza JR, Savageau JA, Rigotti NA, et al. Trait anxiety and nicotine dependence in adolescents: a report from the DANDY study. Addict Behav. 2004;29:911–9. doi: 10.1016/j.addbeh.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 50.Piper ME, Piasecki TM, Federman EB, et al. a multiple motives approach to tobacco dependence: the Wisconsin Inventory of Smoking Dependence Motives (WISDM-68) J Consult Clin Psychol. 2004;72:139–54. doi: 10.1037/0022-006X.72.2.139. [DOI] [PubMed] [Google Scholar]
- 51.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 52.World Health Organization. International Statistical Classification of Diseases and Related Health Problems – 10th revision. Geneva Switzerland: World Health Organization; 2010. [Google Scholar]
- 53.Lubin JH, Caporaso N, Hatsukami DK, Joseph AM, Hecht SS. The association of a tobacco-specific biomarker and cigarette consumption and its dependence on host characteristics. Cancer Epidemiol Biomarkers Prev. 2007;16:1852–7. doi: 10.1158/1055-9965.EPI-07-0018. [DOI] [PubMed] [Google Scholar]
- 54.Muscat JE, Chen G, Knipe A, Stellman SD, Lazarus P, Richie JP., Jr Effects of menthol on tobacco smoke exposure, nicotine dependence, and NNAL glucuronidation. Cancer Epidemiol Biomarkers Prev. 2009;18:35–41. doi: 10.1158/1055-9965.EPI-08-0744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fagerström KO. Determinants of tobacco use and renaming the FTND to the Fagerström test for cigarette dependence. Nicotine Tob Res. 2012;14:75–8. doi: 10.1093/ntr/ntr137. [DOI] [PubMed] [Google Scholar]
- 56.Allen B, Jr., Unger JB. Sociocultural correlates of menthol cigarette smoking among adult African Americans in Los Angeles. Nicotine Tob Res. 2007;9:447–51. doi: 10.1080/14622200701239647. [DOI] [PubMed] [Google Scholar]
- 57.Faseru B, Choi WS, Krebill R, et al. Factors associated with smoking menthol cigarettes among treatment-seeking African American light smokers. Addict Behav. 2011;36:1321–4. doi: 10.1016/j.addbeh.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gandhi KK, Foulds J, Steinberg MB, Lu SE, Williams JM. Lower quit rates among African American and Latino menthol cigarette smokers at a tobacco treatment clinic. Int J Clin Pract. 2009;63:360–7. doi: 10.1111/j.1742-1241.2008.01969.x. [DOI] [PubMed] [Google Scholar]
- 59.Hymowitz N, Corle D, Royce J, et al. Smokers’ baseline characteristics in the COMMIT trial. Prev Med. 1995;24:503–8. doi: 10.1006/pmed.1995.1080. [DOI] [PubMed] [Google Scholar]
- 60.Okuyemi KS, Ebersole-Robinson M, Nazir N, Ahluwalia JS. African-American menthol and nonmenthol smokers: differences in smoking and cessation experiences. J Natl Med Assoc. 2004;96:1208–11. [PMC free article] [PubMed] [Google Scholar]
- 61.Pletcher MJ, Hulley BJ, Houston T, Kiefe CI, Benowitz N, Sidney S. Menthol cigarettes, smoking cessation, atherosclerosis, and pulmonary function: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arch Intern Med. 2006;166:1915–22. doi: 10.1001/archinte.166.17.1915. [DOI] [PubMed] [Google Scholar]
- 62.Rosenbloom J, Rees VW, Reid K, Wong J, Kinnunen T. A cross-sectional study on tobacco use and dependence among women: does menthol matter? Tob Induc Dis. 2012;10:19. doi: 10.1186/1617-9625-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jones MR, Apelberg BJ, Tellez-Plaza M, Samet JM, Navas-Acien A. Menthol cigarettes, race/ethnicity, and biomarkers of tobacco use in U.S. adults: the 1999–2010 National Health and Nutrition Examination Survey (NHANES) Cancer Epidemiol Biomarkers Prev. 2013;22:224–32. doi: 10.1158/1055-9965.EPI-12-0912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jain RB. Trends in serum cotinine concentrations among daily cigarette smokers: data from NHANES 1999–2010. Sci Total Environ. 2014;472:72–7. doi: 10.1016/j.scitotenv.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 65.Cubbin C, Soobader MJ, LeClere FB. The intersection of gender and race/ethnicity in smoking behaviors among menthol and non-menthol smokers in the United States. Addiction. 2010;105(Suppl 1):32–8. doi: 10.1111/j.1360-0443.2010.03191.x. [DOI] [PubMed] [Google Scholar]
- 66.Hyland A, Garten S, Giovino GA, Cummings KM. Mentholated cigarettes and smoking cessation: findings from COMMIT. Tob Control. 2002;11:135–9. doi: 10.1136/tc.11.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lawrence D, Rose A, Fagan P, Moolchan ET, Gibson JT, Backinger CL. National patterns and correlates of mentholated cigarette use in the United States. Addiction. 2010;105(Suppl 1):13–31. doi: 10.1111/j.1360-0443.2010.03203.x. [DOI] [PubMed] [Google Scholar]
- 68.Okuyemi KS, Faseru B, Sanderson Cox L, Bronars CA, Ahluwalia JS. Relationship between menthol cigarettes and smoking cessation among African American light smokers. Addiction. 2007;102:1979–86. doi: 10.1111/j.1360-0443.2007.02010.x. [DOI] [PubMed] [Google Scholar]
- 69.Stahre M, Okuyemi KS, Joseph AM, Fu SS. Racial/ethnic differences in menthol cigarette smoking, population quit ratios and utilization of evidence-based tobacco cessation treatments. Addiction. 2010;105(Suppl 1):75–83. doi: 10.1111/j.1360-0443.2010.03200.x. [DOI] [PubMed] [Google Scholar]
- 70.Fagan P, Moolchan ET, Hart A, Jr, Rose A, Lawrence D, Shavers VL, Gibson JT. Nicotine dependence and quitting behaviors among menthol and non-menthol smokers with similar consumptive patterns. Addiction. 2010;105(Suppl 1):55–74. doi: 10.1111/j.1360-0443.2010.03190.x. [DOI] [PubMed] [Google Scholar]
- 71.Fernander A, Rayens MK, Zhang M, Adkins S. Are age of smoking initiation and purchasing patterns associated with menthol smoking? Addiction. 2010;105(Suppl 1):39–45. doi: 10.1111/j.1360-0443.2010.03188.x. [DOI] [PubMed] [Google Scholar]
- 72.Alexander LA, Crawford T, Mendiondo MS. Occupational status, work-site cessation programs and policies and menthol smoking on quitting behaviors of US smokers. Addiction. 2010;105(Suppl 1):95–104. doi: 10.1111/j.1360-0443.2010.03227.x. [DOI] [PubMed] [Google Scholar]
- 73.Marsh L, McGee R, Gray A. A refreshing poison: one-quarter of young New Zealand smokers choose menthol. Aust New Zealand J Public Health. 2012;36:495–6. doi: 10.1111/j.1753-6405.2012.00926.x. [DOI] [PubMed] [Google Scholar]
- 74.Li J, Paynter J, Arroll B. A cross-sectional study of menthol cigarette preference by 14- to 15-year-old smokers in New Zealand. Nicotine Tob Res. 2012;14:857–63. doi: 10.1093/ntr/ntr299. [DOI] [PubMed] [Google Scholar]
- 75.Giovino GA, Villanti AC, Mowery PD, et al. Differential trends in cigarette smoking in the USA: Is menthol slowing progress? Tob Control. [Epub ahead of print September 27, 2013] [DOI] [PubMed]
- 76.Muilenburg JL, Legge JS., Jr African American adolescents and menthol cigarettes: smoking behavior among secondary school students. J Adolesc Health. 2008;43:570–5. doi: 10.1016/j.jadohealth.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 77.Ahijevych K, Ford J. The relationships between menthol cigarette preference and state tobacco control policies on smoking behaviors of young adult smokers in the 2006–07 Tobacco Use Supplements to the Current Population Surveys (TUS CPS) Addiction. 2010;105(Suppl 1):46–54. doi: 10.1111/j.1360-0443.2010.03201.x. [DOI] [PubMed] [Google Scholar]
- 78.Mendiondo MS, Alexander LA, Crawford T. Health profile differences for menthol and non-menthol smokers: findings from the National Health Interview Survey. Addiction. 2010;105(Suppl 1):124–40. doi: 10.1111/j.1360-0443.2010.03202.x. [DOI] [PubMed] [Google Scholar]
- 79.Rostron B. NNAL exposure by race and menthol cigarette use among U.S. smokers. Nicotine Tob Res. 2013;15:950–6. doi: 10.1093/ntr/nts223. [DOI] [PubMed] [Google Scholar]
- 80.Murray RP, Connett JE, Skeans MA, Tashkin DP. Menthol cigarettes and health risks in Lung Health Study data. Nicotine Tob Res. 2007;9:101–7. doi: 10.1080/14622200601078418. [DOI] [PubMed] [Google Scholar]
- 81.Okuyemi KS, Ahluwalia JS, Ebersole-Robinson M, Catley D, Mayo MS, Resnicow K. Does menthol attenuate the effect of bupropion among African American smokers? Addiction. 2003;98:1387–93. doi: 10.1046/j.1360-0443.2003.00443.x. [DOI] [PubMed] [Google Scholar]
- 82.Collins CC, Moolchan ET. Shorter time to first cigarette of the day in menthol adolescent cigarette smokers. Addict Behav. 2006;31:1460–4. doi: 10.1016/j.addbeh.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 83.Winhusen TM, Adinoff B, Lewis DF, et al. A tale of two stimulants: Mentholated mentholated cigarettes may play a role in cocaine, but not methamphetamine, dependence. Drug Alcohol Depend. 2013;133:845–51. doi: 10.1016/j.drugalcdep.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rojewski AM, Toll BA, O'Malley SS. Menthol cigarette use predicts treatment outcomes of weight-concerned smokers. Nicotine Tob Res. 2014;16:115–9. doi: 10.1093/ntr/ntt137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Blot WJ, Cohen SS, Aldrich M, McLaughlin JK, Hargreaves MK, Signorello LB. Lung cancer risk among smokers of menthol cigarettes. J Natl Cancer Inst. 2011;103:810–6. doi: 10.1093/jnci/djr102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Muscat JE, Richie JP, Jr, Stellman SD. Mentholated cigarettes and smoking habits in whites and blacks. Tob Control. 2002;11:368–71. doi: 10.1136/tc.11.4.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sidney S, Tekawa IS, Friedman GD, Sadler MC, Tashkin DP. Mentholated cigarette use and lung cancer. Arch Intern Med. 1995;155:727–32. [PubMed] [Google Scholar]
- 88.Mustonen TK, Spencer SM, Hoskinson RA, Sachs DP, Garvey AJ. The influence of gender, race, and menthol content on tobacco exposure measures. Nicotine Tob Res. 2005;7:581–90. doi: 10.1080/14622200500185199. [DOI] [PubMed] [Google Scholar]
- 89.Brooks DR, Palmer JR, Strom BL, Rosenberg L. Menthol cigarettes and risk of lung cancer. Am J Epidemiol. 2003;158:609–16. doi: 10.1093/aje/kwg182. [DOI] [PubMed] [Google Scholar]
- 90.Jones MR, Apelberg BJ, Samet JM, Navas-Acien A. Smoking, menthol cigarettes, and peripheral artery disease in U.S. adults. Nicotine Tob Res. 2013;15:1183–9. doi: 10.1093/ntr/nts253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rostron B. Lung cancer mortality risk for U.S. menthol cigarette smokers. Nicotine Tob Res. 2012;14:1140–4. doi: 10.1093/ntr/nts014. [DOI] [PubMed] [Google Scholar]
- 92.Luo Z, Alvarado GF, Hatsukami DK, Johnson EO, Bierut LJ, Breslau N. Race differences in nicotine dependence in the Collaborative Genetic study of Nicotine Dependence (COGEND) Nicotine Tob Res. 2008;10:1223–30. doi: 10.1080/14622200802163266. [DOI] [PubMed] [Google Scholar]
- 93.Hickman NJ, 3rd, Delucchi KL, Prochaska JJ. Menthol use among smokers with psychological distress: findings from the 2008 and 2009 National Survey on Drug Use and Health. Tob Control. 2014;23:7–13. doi: 10.1136/tobaccocontrol-2012-050479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ahijevych K, Parsley LA. Smoke constituent exposure and stage of change in black and white women cigarette smokers. Addict Behav. 1999;24:115–20. doi: 10.1016/s0306-4603(98)00031-8. [DOI] [PubMed] [Google Scholar]
- 95.Benowitz NL, Dains KM, Dempsey D, Havel C, Wilson M, Jacob P., 3rd Urine menthol as a biomarker of mentholated cigarette smoking. Cancer Epidemiol Biomarkers Prev. 2010;19:3013–9. doi: 10.1158/1055-9965.EPI-10-0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.D'Silva J, Boyle RG, Lien R, Rode P, Okuyemi KS. Cessation outcomes among treatment-seeking menthol and nonmenthol smokers. Am J Prev Med. 2012;43(5 Suppl 3):S242–S248. doi: 10.1016/j.amepre.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 97.Muscat JE, Liu HP, Stellman SD, Richie JP., Jr Menthol smoking in relation to time to first cigarette and cotinine: results from a community-based study. Regul Toxicol Pharmacol. 2012;63:166–70. doi: 10.1016/j.yrtph.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Reitzel LR, Etzel CJ, Cao Y, Okuyemi KS, Ahluwalia JS. Associations of menthol use with motivation and confidence to quit smoking. Am J Health Behav. 2013;37:629–34. doi: 10.5993/AJHB.37.5.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jones MR, Tellez-Plaza M, Navas-Acien A. Smoking, menthol cigarettes and all-cause, cancer and cardiovascular mortality: evidence from the National Health and Nutrition Examination Survey (NHANES) and a meta-analysis. PLoS One. 2013;8:e77941. doi: 10.1371/journal.pone.0077941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Moolchan ET, Berlin I, Robinson ML, Cadet JL. African-American teen smokers: Issues to consider for cessation treatment. J Natl Med Assoc. 2000;92:558–62. [PMC free article] [PubMed] [Google Scholar]
- 101.Duncan AE, Lessov-Schlaggar CN, Sartor CE, Bucholz KK. Differences in time to onset of smoking and nicotine dependence by race/ethnicity in a Midwestern sample of adolescents and young adults from a high risk family study. Drug Alcohol Depend. 2012;125:140–5. doi: 10.1016/j.drugalcdep.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.DiFranza JR, Savageau JA, Fletcher K, et al. Recollections and repercussions of the first inhaled cigarette. Addict Behav. 2004;29:261–72. doi: 10.1016/j.addbeh.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 103.Hooper MW, Zhao W, Byrne MM, et al. Menthol cigarette smoking and health, Florida 2007 BRFSS. Am J Health Behav. 2011;35:3–14. doi: 10.5993/ajhb.35.1.1. [DOI] [PubMed] [Google Scholar]
- 104.Reitzel LR, Li Y, Stewart DW, et al. Race moderates the effect of menthol cigarette use on short-term smoking abstinence. Nicotine Tob Res. 2013;15:883–9. doi: 10.1093/ntr/nts335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Brody AL, Mukhin AG, La Charite J, et al. Up-regulation of nicotinic acetylcholine receptors in menthol cigarette smokers. Int J Neuropsychopharmacol. 2013;16:957–66. doi: 10.1017/S1461145712001022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zedler BK, Kinser R, Oey J, et al. Biomarkers of exposure and potential harm in adult smokers of 3–7 mg tar yield (Federal Trade Commission) cigarettes and in adult non-smokers. Biomarkers. 2006;11:201–20. doi: 10.1080/13547500600576260. [DOI] [PubMed] [Google Scholar]
- 107.World Medical Association. 2000.
- 108.Wackowski OA, Delnevo CD. Menthol cigarettes and indicators of tobacco dependence among adolescents. Addict Behav. 2007;32:1964–9. doi: 10.1016/j.addbeh.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 109.Hersey JC, Ng SW, Nonnemaker JM, et al. Are menthol cigarettes a starter product for youth? Nicotine Tob Res. 2006;8:403–13. doi: 10.1080/14622200600670389. [DOI] [PubMed] [Google Scholar]
- 110.Hersey JC, Nonnemaker JM, Homsi G. Menthol cigarettes contribute to the appeal and addiction potential of smoking for youth. Nicotine Tob Res. 2010;12(Suppl 2):S136–S146. doi: 10.1093/ntr/ntq173. [DOI] [PubMed] [Google Scholar]
- 111.Nonnemaker J, Hersey J, Homsi G, Busey A, Allen J, Vallone D. Initiation with menthol cigarettes and youth smoking uptake. Addiction. 2013;108:171–8. doi: 10.1111/j.1360-0443.2012.04045.x. [DOI] [PubMed] [Google Scholar]
- 112.Reitzel LR. Menthol cigarettes, tobacco dependence, and smoking cessation: Project MOM final report. U.S. Food and Drug Administration commissioned secondary analysis; 2010. http://www.fda.gov/downloavds/AdvisoryCommittees/CommitteesMeetingMaterials/TobaccoProductsScientificAdvisoryCommittee/UCM237558.pdf (accessed May 13, 2014) [Google Scholar]
- 113.Reitzel LR. Menthol cigarettes, tobacco dependence, and smoking cessation: Project CARE final report. U.S. Food and Drug Administration commissioned secondary analysis; 2010. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/TobaccoProductsScientificAdvisoryCommittee/UCM237557.pdf (accessed May 13, 2014) [Google Scholar]
- 114.Reitzel LR. Menthol cigarettes, tobacco dependence, and smoking cessation: Project BREAK FREE final report. U.S. Food and Drug Administration commissioned secondary analysis; 2010. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/TobaccoProductsScientificAdvisoryCommittee/UCM237556.pdf (accessed May 13, 2014) [Google Scholar]
- 115.Reitzel LR, Nguyen N, Cao Y, et al. Race/ethnicity moderates the effect of prepartum menthol cigarette use on postpartum smoking abstinence. Nicotine Tob Res. 2011;13:1305–10. doi: 10.1093/ntr/ntr095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.National Cancer Institute. Menthol cigarette use among current smokers ages 18 + years by socio-demographic characteristics, Tobacco Use Supplement to the Current Population Survey, 2006/07. 2013. http://cancercontrol.cancer.gov/tcrb/research_topic-menthol.html (accessed May 13, 2014)
- 117.Gardiner PS. The African Americanization of menthol cigarette use in the United States. Nicotine Tob Res. 2004;6(Suppl 1):S55–S65. doi: 10.1080/14622200310001649478. [DOI] [PubMed] [Google Scholar]
- 118.Unger JB, Allen B, Jr, Leonard E, Wenten M, Cruz TB. Menthol and non-menthol cigarette use among Black smokers in Southern California. Nicotine Tob Res. 2010;12:398–407. doi: 10.1093/ntr/ntq016. [DOI] [PubMed] [Google Scholar]
- 119.Cropsey KL, Weaver MF, Eldridge GD, Villalobos GC, Best AM, Stitzer MI. Differential success rates in racial groups: results of a clinical trial of smoking cessation among female prisoners. Nicotine Tob Res. 2009;11:690–7. doi: 10.1093/ntr/ntp051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Faseru B, Nollen NL, Mayo MS, et al. Predictors of cessation in African American light smokers enrolled in a bupropion clinical trial. Addict Behav. 2013;38:1796–803. doi: 10.1016/j.addbeh.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Foulds J, Gandhi KK, Steinberg MB, et al. Factors associated with quitting smoking at a tobacco dependence treatment clinic. Am J Health Behav. 2006;30:400–12. doi: 10.5555/ajhb.2006.30.4.400. [DOI] [PubMed] [Google Scholar]
- 122.Harris KJ, Okuyemi KS, Catley D, Mayo MS, Ge B, Ahluwalia JS. Predictors of smoking cessation among African-Americans enrolled in a randomized controlled trial of bupropion. Prev Med. 2004;38:498–502. doi: 10.1016/j.ypmed.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 123.Steinberg MB, Delnevo CD, Hrywna M. Update in New Jersey tobacco-dependence treatment. N J Med. 2002;99(11):21–6. [PubMed] [Google Scholar]


