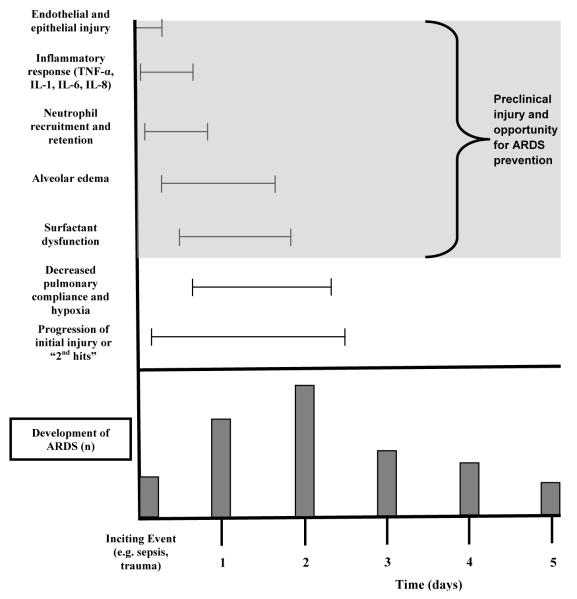
Figure 3.
Simplified schematic of the pathogenesis of acute respiratory distress syndrome (ARDS) with respect to time. After an inciting event, capillary endothelial and alveolar epithelial injury can occurs in minutes to hours. Activated immune cells (e.g. monocytes and macrophages) contribute to a cytokine-mediated inflammatory response. This serves to recruit neutrophils, which play a critical role in ARDS initiation and propagation, through the injured endothelium. Protein-rich pulmonary edema and subsequent surfactant loss lead to alveolar collapse, hypoxia, and reduced lung compliance [133,134]. If the primary injury is robust enough, or if modifiable secondary injuries occur (e.g. high tidal volume, transfusion, delayed sepsis treatment), ARDS develops, with a typical median onset of two days. Many of these pathogenic mechanisms for ARDS initiation occur prior to clinical evidence of the syndrome, and this window of pre-clinical injury forms the basis for ARDS preventive measures.
TNF: tumor necrosis factor; IL: interleukin; ARDS: acute respiratory distress syndrome